Managing the “difficult” gallbladder
The gold standard for the surgical treatment of symptomatic cholelithiasis is conventional laparoscopic cholecystectomy (LC). The “difficult gallbladder” is a scenario in which a cholecystectomy turns into an increased surgical risk compared with standard cholecystectomy. The procedure may be difficult due to processes that either obscure normal biliary anatomy (such as acute or chronic inflammation) or operative exposure (obesity or adhesions caused by prior upper abdominal surgery). So, when confronted with a difficult cholecystectomy, the surgeon has a must: to turn the operation into a safe cholecystectomy, which can mean conversion (to an open procedure), cholecystostomy, or partial/ subtotal cholecystectomy. The surgeon should understand that needs to rely on damage control, to prevent more serious complications if choosing to advance and progress to a complete cholecystectomy.
When to Predict a Difficult Laparoscopic Cholecystectomy
A difficult cholecystectomy may be predicted preoperatively based on patient characteristics and ultrasound and laboratory findings. This is probably a very important step in mitigating the high risk associated with a difficult procedure and may serve either to reschedule the procedure or design intraoperative strategies of management to guarantee a safe performance of the surgical procedure.
The following situations are associated with a higher chance of a difficult cholecystectomy:
• Acute cholecystitis (more than 5 days of onset)
• Previous cholecystitis episode
• Male sex
• Obesity
• Cirrhosis
• Sclero-atrophic gallbladder
• Thick walls (>5 mm)
• Previous signs of canalicular dwelling (clinical and laboratory)
Through multivariate analysis, Bourgoin identified these elements of predictive help to identify difficult LC: male sex, previous cholecystitis attack, fibrinogen, neutrophil, and alkaline phosphatase levels. Another important point is the fact of conversion from a laparoscopic procedure to an open and traditional cholecystectomy, usually through a right subcostal incision. Conversion should not be considered as a personal failure, and the surgeon needs to understand the concept of “safety first,” considering that conversion is performed in order to complete the procedure without additional risks and preventing complications and not solving intraoperative complications. It is also useful to define a time threshold to aid in the decision to convert. It is not worth taking an hour and a half and still dissecting adhesions, preventing the correct visualization of the cystic pedicle. This time limit represents a method to prevent inefficiencies in the operating room (OR) schedule as well as additional expenditures.
A smart surgeon should rely to conversion in the following situations:
• Lack of progress in the procedure
• Unclear anatomy/any grade of uncertainty
• CVS not achieved
• Bleeding/vascular injury
• BD injury
• Lack of infrastructure, expertise, and support
Final Remarks
The primary goal of a laparoscopic cholecystectomy in the treatment of symptomatic cholelithiasis is the safe remotion of the gallbladder and the absence of common bile duct injury. Some tips to take into account:
– Never perform a laparoscopic cholecystectomy without a skilled surgeon close by.
– Beware of the easy gallbladder.
– Slow down, take your time.
– Knowledge is power, conversión can be the salvation!
– Do not repair a bile duct injury (unless you have performed at least 25 hepaticojejunostomies).
– Do not ignore postoperative complaints (pain, jaundice, major abdominal discomfort, fever)
Other options when confronted with a difficult laparoscopic cholecystectomy are:
– A percutaneous cholecystostomy, if the risk was identified preoperatively or the patient is a poor surgical candidate;
– An intraoperative cholangiography, which may aid in identifying an injury to the bile duct and solve it, if you are an experienced surgeon;
– A subtotal or partial cholecystectomy;
– Ask for help;
– Conversion to an open procedure;
Liver Procurement
Donor Evaluation and Management
There are very few absolute contraindications for abdominal organ donation, which can be summarized in the short form CHUMP: (1) Creutzfeldt-Jakob disease, (2) active HIV infection, (3) uncontrolled donor sepsis, (4) history of melanoma or other malignancy that poses a risk for transmission regardless of the apparent disease – free period, and (5) past history of non-curable malignancy (curable malignancy such as localized small kidney tumors, localized prostate cancer, localized colon malignancy >5 years previously may be considered after careful risk/benefit assessment). In addition to these general criteria, there are organ-specific criteria for guiding the acceptance of a liver for transplantation. A history of hepatitis or alcoholism is certainly a warning sign, but both livers from HBsAg-positive and/or HCV-positive donors are currently used worldwide, and suitability for transplant must be judged on a case-by-case basis. In general, in the case of a marginal liver donor, the intraoperative assessment by the donor surgeon, in addition to liver biopsy pathological evaluation, is the best single piece of information.
Technical Aspects of Liver Procurement
A midline laparotomy from the xyphoid to the pubis is performed and the round ligament divided. The intra-abdominal organs are explored to check for eventual malignancies, and the quality of the liver is assessed: in the absence of contraindications for a transplant, a sternotomy can be performed. Of note, in the presence of prior heart surgery, the complete warm dissection should be made prior to the sternotomy. It is also prudential to isolate and encircle the aorta prior to sternotomy in order to be ready to cannulate in the event of cardiac arrest/injury at thoracotomy. A blunt dissection behind the sternum just below the jugular notch should be performed until the fingertip can be placed retrosternal around the jugular notch. The sternotomy is then performed in a cranial to caudal direction with the sternum saw to avoid left innominate vein injury. The division of the left triangular ligament allows the mobilization of the left lateral segments of the liver and the exposure of the supraceliac aorta just below the diaphragm to be encircled. The division of the falciform ligament up to the suprahepatic inferior vena cava (IVC) provides more mobility of the liver, necessary when the IVC must be divided from a cardiac graft. Before starting the dissection of the hepatoduodenal ligament, the hepatogastric ligament must be inspected by dividing the lesser omentum. This ligament is usually very thin and transparent so that any replaced or accessory left hepatic artery should be easily visible. In addition, palpation of the ventral border of the foramen of Winslow makes it possible to identify a possible accessory or replaced right hepatic artery. Variations in the hepatic arterial supply can complicate the hilar dissection in up to one third of donors.
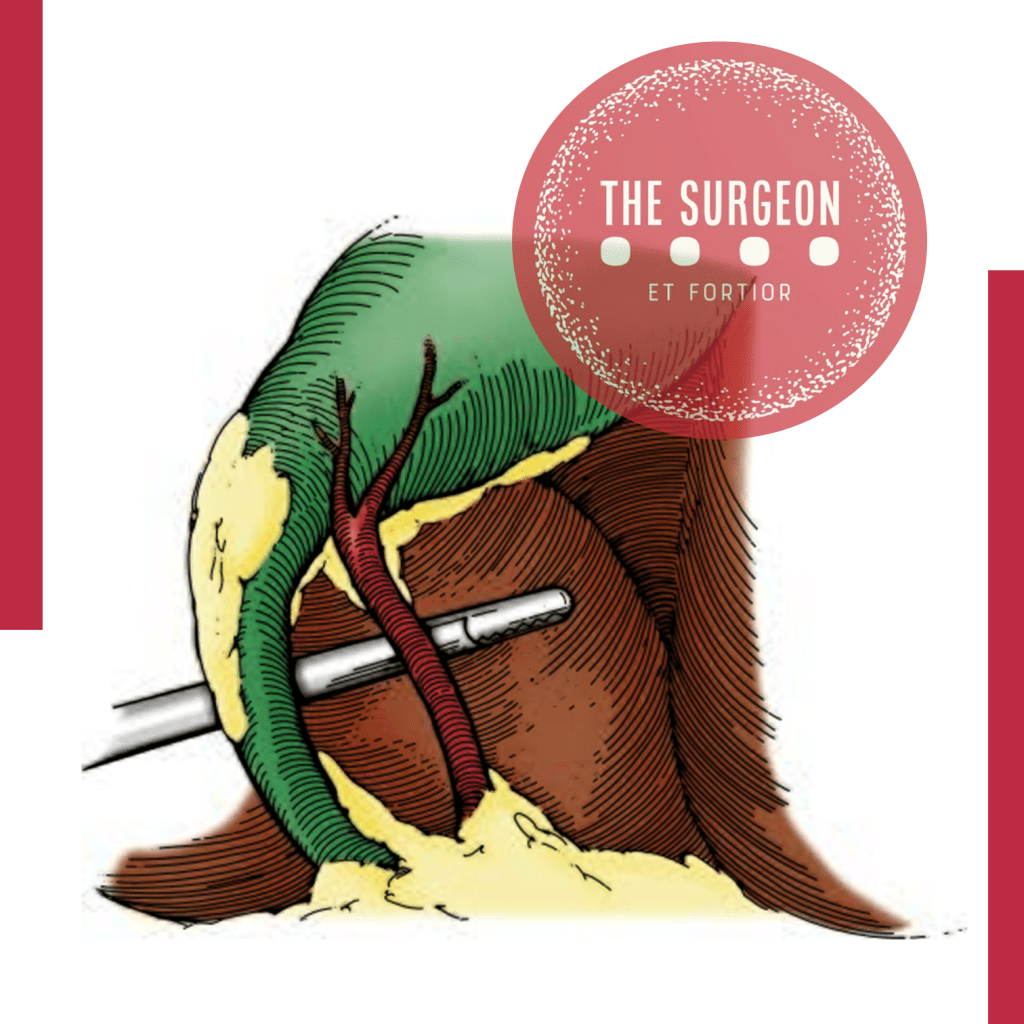
THE HILAR STRUCTURES
The hilar structures of the liver are then dissected free; the common bile duct (CBD) is dissected on the level of the edge of the second duodenal portion after opening of the peritoneum and visualization of the duct. In difficult cases, due to a high BMI, following the cystic duct out of the gall bladder can help to identify the CBD. The CBD should be encircled from the lateral border of the hepatoduodenal ligament in order to avoid injury of the portal vein. The CBD and the gallbladder are opened and flushed with normosaline solution. The origins of the gastroduodenal, gastric, and splenic arteries are then identified and encircled and, in the case of liver only procurement, will be taped just before cross-clamping in order to increase flushing through the hepatic artery to the liver.
VASCULAR CANULATION / SOLUTION PRESERVATION
The aorta can be isolated by two approaches. One approach requires mobilization of the right colon on top of Gerota’s fascia and should be extended into a Kocher maneuver to uncover both the inferior vena cava and the abdominal aorta; the other approach is performed by opening the root of the mesentery from the Treitz fascia, along the margin of the duodenum until visualization of the right iliac vessels and ureter is achieved. The inferior mesenteric artery can be tied and divided, and the abdominal aorta, just 2–3 cm above the bifurcation, isolated and encircled. The lumbar arteries could be either tied or clipped and then cut in order to provide mobility of the aorta and facilitate the cannulation. Two umbilical tapes are placed around the dissected segment of the aorta and secured by clamps and will be used to secure aortic cannulae to the vessel. The inferior mesenteric vein (IMV) is most commonly used for access into the portal system by ligating the distal part of it but leaving it uncut to retract the vein with a mosquito clamp. Another tie is then placed around the cranial portion of the vein, using it for occlusion of the vein by retracting it while a partial incision of the vein is performed. The portal cannula can be inserted into the IMV while the tension of the occluding tie is decreased before tying it around the vein and inserted cannula. At this point, 30,000-IU heparin should be given to prevent the blood from clotting after the cross-clamping. Once these preliminary procedures have been completed, the aortic cannulae (20-F armed cannulae) can be inserted into the distal abdominal aorta and secured with the umbilical tapes.
CROSS-CLAMP
The subdiaphragmatic aorta is now clamped (cross-clamp), and cold preservation solution is then rapidly infused through the aortic and portal cannulae; the liver flow is decompressed by dividing the inferior vena cava in the chest. The abdomen is filled with water and ice. The choice of solution for infusion and its amount varies from center to center. The quality of the flush can be assessed by evaluating the outflow of the supradiaphragmatic IVC which should become more transparent with time as the blood in the abdominal organs is replaced by the preservation solution. After the flush is completed, some of the ice is removed from the abdomen to allow the cold dissection of the structures. The gastroduodenal, gastric, and splenic arteries can now be divided. Just below the gastroduodenal artery, the portal vein can be found and can be followed back, if pancreas procurement is not performed, by dividing the head of the pancreas. The cannulae in the IMV can now be removed, the splenic vein ligated and divided, and the venous cannulae replaced in the superior mesenteric vein once it is divided from its distal branches. The superior mesenteric artery (SMA) can now be found in the retro-pancreatic laminae and should be ligated, secured to a clamp and divided in order to find the aortic plane by following back the SMA. This dissection must be made on the left side of the SMA in order to avoid damage to a possible replaced or accessory right hepatic artery. The renal arteries are usually just below the SMA. They should be visualized before the suprarenal aorta is divided. This section must be made in 45°, first looking for ostia of accessory renal arteries before performing complete separation of the aorta. By following back the splenic and gastric arteries, the celiac trunk can be visualized. The aorta must now be divided just below the diaphragm, obtaining a patch containing the celiac trunk and the origin of the mesenteric artery. At this time point, a finger is placed in the supradiaphragmatic IVC helping to identify it while the diaphragm is cut. A portion of the diaphragm should be kept with the liver to ensure that this gross and fast dissection does not damage the organ. The diaphragm is cut to the right, and the incision is then continued between the right kidney and the liver, usually dividing the adrenal gland which is a good sign that none of the adjacent organs are damaged. The location for division of the infrahepatic IVC depends on the renal veins. These are identified on both sides, and the IVC can be safely divided on the virtual line about 1 cm above the renal veins. The only structures now holding the liver in the abdomen are the diaphragmatic pillars. By keeping the liver to the right thoracic cavity and holding the aortic patch, the resected IVC, and the portal vein with its cannulae, the liver removal can be completed by cutting the diaphragmatic muscles. The liver is freed and taken out of the abdomen. A further perfusion with cool preservation solution should be performed on the back table before packing the liver in the transportation box usually with 1 l of preservation solution. The liver can now be packed in the transportation box.
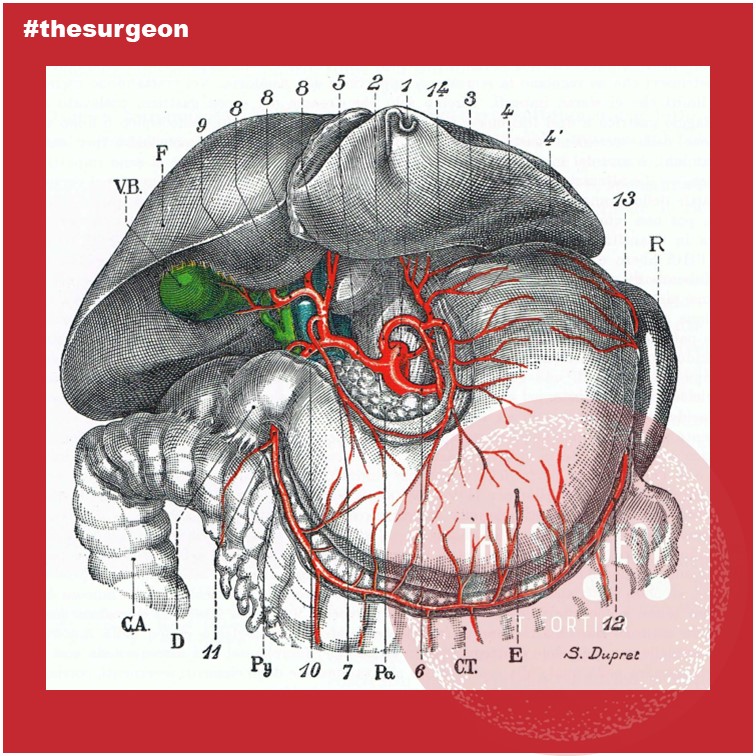
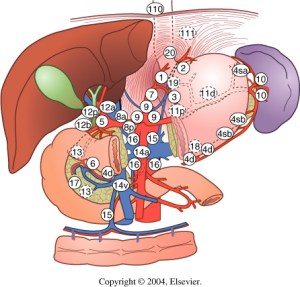
Biliary Tree Vascularization
The gallbladder lies at the equator between the right and left hemiliver, an imaginary line known as Cantlie’s line or the Rex-Cantlie line coursing between segments 4b and 5, through the bed of the gallbladder towards the vena cava posteriorly. The gallbladder is mostly peritonealized, except for its posterior surface which lies on the cystic plate, a fibrous area on the underside of the liver.
The proportion if its circumference varies, from a pedicled gallbladder with little to no contact with the cystic plate to a mostly intrahepatic gallbladder surrounded by liver parenchyma. The gallbladder carries no muscularis mucosa, no submucosa, and a discontinuous muscularis and only carries a serosa on the visceral peritonealized surface. These anatomical specificities facilitate the direct invasion of gallbladder cancer into the liver. This is why the surgical treatment of gallbladder cancer mandates a radical cholecystectomy, which includes resection of a wedge of segments 4b and 5, when the T stage is higher or equal to T1b. From the body of the gallbladder, a conical infundibulum becomes a cystic duct that extends as the lower edge of the hepatocystic triangle towards the porta hepatis and joins with the common hepatic duct (CHD) to form the CBD. As in the rest of the biliary system, variation is the rule when it comes to the cystic duct confluence with the CHD. It can variably run parallel to it for a distance prior to inserting or spiral behind it and insert on its medial aspect. It can variably insert into the RHD or the RPD, the latter in 4% of livers and particularly when the RPD inserts into the CHD (i.e., below the left-right ductal confluence). This configuration is notorious for exposing the RPD to a risk of injury at the time of cholecystectomy. Rare variations of gallbladder anatomy, including gallbladder duplication and gallbladder agenesis, are also described but are rare. The CBD courses anterolaterally within the hepatoduodenal ligament, usually to the right of the hepatic artery and anterolaterally to the portal vein. However, hepatic arterial anatomy can vary, and when an accessory or replaced hepatic artery is present arising from the superior mesenteric artery, the accessory or replaced vessel courses lateral to the CBD. In its conventional configuration, the right hepatic artery crosses posteriorly to the RHD as it heads towards the right liver, but 25% of the time it crosses anteriorly. These anatomical variants are all relevant to developing a sound surgical strategy to treat hilar CCA. Of note, while left hepatic artery anatomy can also be quite variable, rarely does it affect surgical decision-making in CCA to the same degree as right hepatic artery anatomy.
Distally, the CBD enters the head of the pancreas, joining the pancreatic duct to form the hepatopancreatic ampulla. Just distal to this is the sphincter of Oddi, which controls emptying of ampullary contents into the second portion of the duodenum. When the junction of the CBD and the pancreatic duct occurs before the sphincter complex, reflux of pancreatic enzymes into the biliary tree can lead to chronic inflammatory changes and anatomical distortion resulting in choledochal cysts, known risk factors for the development of CCA. Unlike the rest of the liver parenchyma, which receives dual supply from the arterial and portal venous circulation, the biliary tree is exclusively alimented by the arterial system. The LHD and RHD are alimented respectively by the left hepatic artery and right hepatic artery, which can frequently display replaced, accessory, and aberrant origins – the left artery arising conventionally from the hepatic artery proper but alternatively from the left gastric artery and the right hepatic artery arising from the hepatic artery proper but also variably from the superior mesenteric artery. In hilar CCA, variable combinations of hepatic arterial anatomy and tumor location can either favor resectability or make a tumor unresectable.
Within the hilum of the liver, a plexus of arteries connects the right and left hepatic arteries. Termed the “hilar epicholedochal plexus,” this vascular network provides collateral circulation that can maintain arterial supply to one side of the liver if the ipsilateral vessel is damaged. The preservation of arterial blood supply to the liver remnant is crucial, particularly when creating an enterobiliary anastomosis. Its absence leads to ischemic cholangiopathy and liver abscesses that can be difficult to treat. The CBD receives arterial supply inferiorly from paired arterioles arising from the gastroduodenal artery and the posterior superior pancreaticoduodenal artery, the most important and constant arterial supply to the distal CBD. Proximally the CBD is alimented by paired arterioles of the right hepatic artery. These vessels, known as the marginal arteries, run in parallel to the CBD, laterally and medially to it. Denuding the CBD of this arterial supply risks stricture formation after choledochoenteric anastomosis.
#OzimoGama #TheSurgeon #DigestiveSurgery
References : https://bit.ly/3fOmcv2
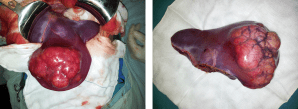
Hepatocellular ADENOMA
Benign liver tumours are common and are frequently found coincidentally. Most benign liver lesions are asymptomatic, although larger lesions can cause non-specific complaints such as vague abdominal pain. Although rare, some of the benign lesions, e.g. large hepatic adenomas, can cause complications such as rupture or bleeding. Asymptomatic lesions are often managed conservatively by observation. Surgical resection can be performed for symptomatic lesions or when there is a risk of malignant transformation. The type of resection is variable, from small, simple, peripheral resections or enucleations, to large resections or even liver transplantation for severe polycystic liver disease.
General Considerations
Hepatocellular adenomas (HCA) are rare benign hepatic neoplasms in otherwise normal livers with a prevalence of around 0.04% on abdominal imaging. HCAs are predominantly found in women of child-bearing age (2nd to 4th decade) with a history of oral contraceptive use; they occur less frequently in men. The association between oral contraceptive usage and HCA is strong and the risk for a HCA increases if an oral contraceptive with high hormonal potency is used, and if it is used for over 20 months. Long-term users of oral contraceptives have an estimated annual incidence of HCA of 3–4 per 100000. More recently, an increase in incidence in men has been reported, probably related to the increase in obesity, which is reported as another risk factor for developing HCA. In addition, anabolic steroid usage by body builders and metabolic disorders such as diabetes mellitus or glycogen storage disease type I are associated with HCAs. HCAs in men are generally smaller but have a higher risk of developing into a malignancy. In the majority of patients, only one HCA is found, but in a minority of patients more than 10 lesions have been described (also referred to as liver adenomatosis).
Clinical presentation
Small HCAs are often asymptomatic and found on abdominal imaging being undertaken for other purposes, during abdominal surgery or at autopsy. Some patients present with abdominal discomfort, fullness or (right upper quadrant) pain due to an abdominal mass. It is not uncommon that the initial symptoms of a HCA are acute onset of abdominal pain and hypovolaemic shock due to intraperitoneal rupture. In a series of patients who underwent resection, bleeding was reported in up to 25%. The risk of rupture is related to the size of the adenoma. Exophytic lesions (protruding from the liver) have a higher chance of bleeding compared to intrahepatic or subcapsular lesions (67% vs 11% and 19%, respectively, P<0.001). Lesions in segments II and III are also at higher risk of bleeding compared to lesions in the right liver (35% vs 19%, P = 0.049).
Management
There is no guideline for the treatment of HCAs, although there are general agreements. In men, all lesions should be considered for surgical resection independent of size, given the high risk of malignant transformation, while taking into account comorbidity and location of the lesion. Resection should also be considered in patients with HCAs due to a metabolic disorder. In women, lesions <5 cm can be observed with sequential imaging after cessation of oral contraceptive treatment. In larger tumours, treatment strategies vary. Some clinicians have proposed non-surgical management if hormone therapy is stopped and patients are followed up with serial radiological examinations. The time period of waiting is still under debate, however recent studies indicate that a waiting period of longer than 6 months could be justified.
More recently, the subtypes of the Bordeaux classification of HCA have been studied related to their risk of complications. Some groups report that percutaneous core needle biopsy is of limited value because the therapeutic strategy is based primarily on patient sex and tumour size. Others report a different therapeutic approach based on subtype. Thomeer et al. concluded that there was no evidence to support the use of subtype classification in the stratification and management of individual patients related to risk of bleeding. Size still remains the most important feature to predict those at risk of bleeding during follow-up. However, malignant transformation does seem to be related to differences in subtypes. β-catenin-mutated HCAs trigger a potent mitogenic signalling pathway that is prominent in HCC. Cases of inflammatory HCAs can also show activation of the β-catenin pathway with a risk of developing malignancy. Therefore, β-catenin-mutated and inflammatory HCAs are prone to malignant degeneration, and particularly if >5cm. In these circumstances, invasive treatment should be considered.
Liver Uptake on Cadaveric Donors for Transplant
Since the initial descriptions of orthotopic liver transplantation (OLT) in the 1960s, both the number of patients receiving transplants and the indications for the procedure have increased significantly. OLT represents the only treatment modality for many patients with a diverse spectrum of disease, with the predominant common factor end-stage liver failure. Advances in perioperative care of the donor and recipient, organ preservation methods, and surgical techniques have resulted in a 5 year overall survival of 78% for all recipients (Kim et al, 2015).
OPERATIVE TECHNIQUES
The first published description of human liver transplantation was by Starzl and colleagues in 1963 at the University of Colorado. In this seminal paper, the dismal outcomes of three OLT recipients were described, including one intraoperative death from uncorrectable coagulopathy and two survivors of 7 and 22 days. In addition to the pioneering conceptual framework and implementation of LT, the advanced techniques included grafts from non–heart-beating donors, venovenous bypass in the recipients, choledochocholedochostomy, and coagulation monitoring by using thromboelastography (TEG). Many of these concepts remain or have reentered the realm of LT more than 40 years after their initial description. Based largely on the initial body of work by Starzl and colleagues, this section describes the surgical procedures commonly used worlwide.
The typical deceased donor has had a catastrophic head injury or an intracerebral bleed, with brain death but without multisystem organ failure. Electrolyte imbalance and hepatic steatosis in the donor are predictors of graft nonfunction. A “donor risk index” has been derived to assess the likelihood of good graft function. Key adverse factors include older donor age (especially >60 years of age), use of a split or partial graft, and a non–heart-beating donor, from which the organs are harvested after the donor’s cardiac output ceases, in contrast to the more typical deceased donation in which the organs are harvested prior to cardiovascular collapse. Use of non–heart-beating donors is associated with reduced rates of long-term graft survival and increased risk of biliary complications, which correlate with the duration of “warm ischemia” after cardiovascular collapse and before retrieval of the organ. With the critical shortage of deceased organ donors, expansion of the donor pool has included acceptance of donors 70 years of age and older for selected recipients. Prior to hepatectomy, the harvesting team makes a visual and, if necessary, histologic assessment of the donor organ. Particular attention is paid to anatomic variants in the hepatic artery that may complicate the graft arterial anastomosis in the recipient. Once donor circulation is interrupted, the organ is rapidly infused with a cold preservation solution (e.g., University of Wisconsin, histidine-tryptophan-ketoglutarate, or Institut Georges Lopez solution). Donor iliac arteries and veins are also retrieved in case vascular grafting is required. After its arrival at the recipient institution, further vascular dissection, with arterial reconstruction if necessary, is performed before implantation.
Future Perspectives
Major challenges remain in LT, including the shortage of donor organs, threat of recurrent disease, and morbidity associated with lifelong therapeutic immunosuppression. Nevertheless, the availability of LT has transformed the lives of patients with advancing liver disease and their health care providers from an ultimately futile effort to manage the complications of cirrhosis into a life-prolonging and life-enhancing intervention.
POPF after Distal Pancreatectomy
Minimally Invasive Versus Open Techniques
Despite advances in laparoscopic and robotic approaches, the vast majority of distal pancreatectomies continue to be performed via an open approach. Recent retrospective data have demonstrated that minimally invasive distal pancreatectomy is associated with decreased blood loss and shorter hospital stays than open pancreatectomy. A large recent study utilizing the Nationwide Inpatient Sample database suggested, first, that the minimally invasive approach is becoming more widely utilized, increasing from 2.4 to 7.3 % over a study period from 1998 to 2009. Second, that study reported that the minimally invasive approach was associated with decreased length of stay as well as decreased incidence of infectious complications, bleeding complications, and blood transfusions. This population-based study echoes conclusions drawn by a large multi-institutional study performed several years previously. Drawing on a combined patient sample of 667 patients, with 24 % initially attempted laparoscopically, the authors were able to demonstrate lower overall complication rate, decreased blood loss, and shorter hospital stays among patients undergoing laparoscopic approach via a multivariate analysis.
Notably, there was no significant difference in the pancreatic leak rate between the open and laparoscopic approaches, although there was a nonsignificant trend favoring the laparoscopic approach. More recently, the robotic approach has generated significant interest as a technique for performing distal pancreatectomy. Retrospective analysis has suggested that the robotic approach is well suited for pancreatectomy. Fistula rates, however, remain a concern. A retrospective review of patients undergoing robotic pancreatic operations included 83 patients who underwent distal pancreatectomy. About 27 % were identified as having a ISPGF type A pancreatic leak; 12 and 4.8 % were identified as having a grade B or C leak, respectively.
Identifying Risk Factors
For pancreaticoduodenectomy (PTD) , a fistula risk score has been recently developed that has been shown to be highly predictive of POPF. This score assigns points based on gland texture, gland pathology, duct diameter, and intraoperative blood loss. In general, high blood loss, soft gland texture, and smaller duct diameter confer increased risk of POPF, whereas pancreatic adenocarcinoma and pancreatitis as the indication for PTD confer protection for the development of pancreatic fistula versus other diagnoses. Also of note, higher fistula risk scores correlated with greater incidence of clinically relevant (ISGPF grade B or C) fistula. The adaptation of this risk score to patients undergoing distal pancreatectomy is yet to be validated; however, at least one published study indicates that this scoring system may have limitations in the setting of distal pancreatectomy. In that study, risk factors for pancreatic fistula after stapled gland transection in patients undergoing distal pancreatectomy were examined, and in a multivariate analysis, only the presence of diabetes and the use of a 4.1-mm staple cartridge were associated with increased risk of pancreatic fistula formation.
PhD THESIS (Ozimo Gama, MD)
COMPARATIVE STUDY BETWEEN THE SLEEVE GASTRECTOMY AND GASTRIC PLICATION IN OBESE RATS
INTRODUCTION: Obesity results from a prolonged imbalance between energy intake and energy expenditure. Studies with experimental models of bariatric surgery provided a fundamental contribution to the understanding of morphological and functional changes in obesity and after bariatric surgery. The restrictive bariatric surgery techniques currently used are gastric banding, sleeve gastrectomy and the gastric plication. The latter is considered an experimental technique and has therefore not yet enough studies that shed light on the postoperative rates of weight loss, surgical complications, resolution of comorbidities and the mechanisms responsible for weight loss. The aim of this study was to conduct a comparative study in rats with cafeteria diet-induced, between gastric plication and sleeve gastrectomy in variation late postoperative in body weight ,plasma biochemistry and gross and microscopic alterations gastric effects obesity.
MATERIAL AND METHOD: 28 male Wistar rats were randomized into three groups after induction period of obesity by cafeteria diet and underwent sleeve gastrectomy (GV group), gastric plication (GP group) and sham operation (control group). The animals were assessed daily postoperatively and the variables were recorded: (initial seven days, 14 and 21 days) body weight and presence of complications until day 21 postoperatively, when they were euthanized and evaluated: biochemistry (glucose, insulin, HDL, total cholesterol, triglycerides, AST, ALT and serum ghrelin), degree of intra-abdominal adhesions, resistance testing will air insufflation in the stomach and microscopic evaluation of the gastric mucosa.

RESULTS: In relation to body weight variation of animals GV group (initial weight: 318 ± 7.89 g / Final weight: 213 ± 9.03g) was significantly decreased (p<0.05) at 21 post-surgery day compared to the GP group (initial weight: 314.11 ± 20.79 g / final weight: 239.16 ± 14.71 g) and control (initial weight: 315.16±17.54g / final weight: 317.91±16.06 g). The animals in the GV group had a significant decrease (p<0.001) in blood glucose, insulin, transaminases, serum HDL and ghrelin compared to animals in GP and control. Was also significantly lower the burst pressure of the stomach in the GV group, the insufflation test the atmospheric air in relation to the GP and control groups. The GP and GV groups showed even different histological grade of inflammation
(subacute inflammation) and control group (chronic inflammation).
CONCLUSIONS: The sleeve gastrectomy is more effective than gastric plication weight loss, metabolic control and reduction of serum ghrelin in obesity rats, and presents the same rates of postoperative complications (adhesions, deaths and grade inflammation).
KEYWORDS: 1. Obesity; 2. Bariatric Surgery; 3.Wistar rats.
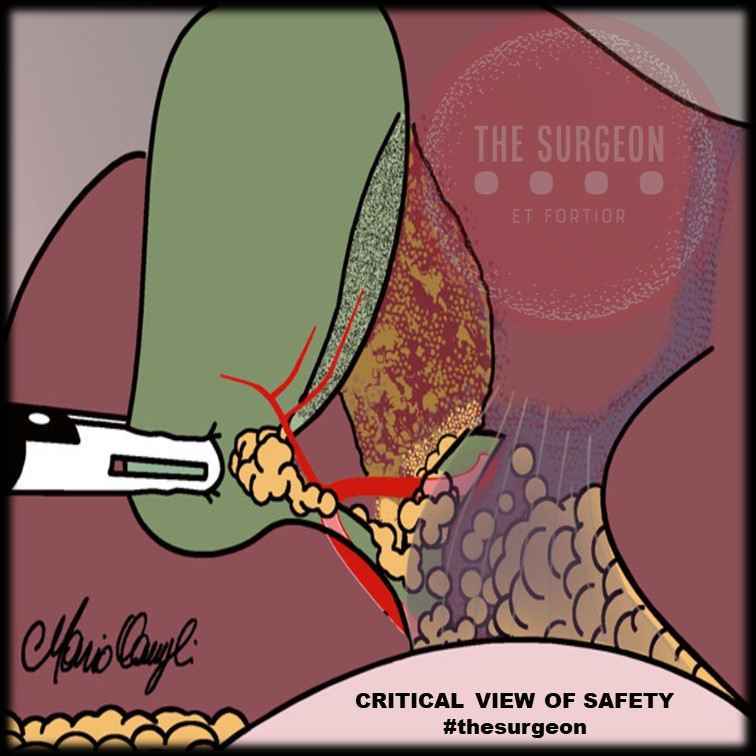
Critical View Of Safety
“The concept of the critical view was described in 1992 but the term CVS was introduced in 1995 in an analytical review of the emerging problem of biliary injury in laparoscopic cholecystectomy. CVS was conceived not as a way to do laparoscopic cholecystectomy but as a way to avoid biliary injury. To achieve this, what was needed was a secure method of identifying the two tubular structures that are divided in a cholecystectomy, i.e., the cystic duct and the cystic artery. CVS is an adoption of a technique of secure identification in open cholecystectomy in which both cystic structures are putatively identified after which the gallbladder is taken off the cystic plate so that it is hanging free and just attached by the two cystic structures. In laparoscopic surgery complete separation of the body of the gallbladder from the cystic plate makes clipping of the cystic structures difficult so for laparoscopy the requirement was that only the lower part of the gallbladder (about one-third) had to be separated from the cystic plate. The other two requirements are that the hepatocystic triangle is cleared of fat and fibrous tissue and that there are two and only two structures attached to the gallbladder and the latter requirements were the same as in the open technique. Not until all three elements of CVS are attained may the cystic structures be clipped and divided. Intraoperatively CVS should be confirmed in a “time-out” in which the 3 elements of CVS are demonstrated. Note again that CVS is not a method of dissection but a method of target identification akin to concepts used in safe hunting procedures. Several years after the CVS was introduced there did not seem to be a lessening of biliary injuries.
Operative notes of biliary injuries were collected and studied in an attempt to determine if CVS was failing to prevent injury. We found that the method of target identification that was failing was not CVS but the infundibular technique in which the cystic duct is identified by exposing the funnel shape where the infundibulum of the gallbladder joins the cystic duct. This seemed to occur most frequently under conditions of severe acute or chronic inflammation. Inflammatory fusion and contraction may cause juxtaposition or adherence of the common hepatic duct to the side of the gallbladder. When the infundibular technique of identification is used under these conditions a compelling visual deception that the common bile duct is the cystic duct may occur. CVS is much less susceptible to this deception because more exposure is needed to achieve CVS, and either the CVS is attained, by which time the anatomic situation is clarified, or operative conditions prevent attainment of CVS and one of several important “bail-out” strategies is used thus avoiding bile duct injury.
CVS must be considered as part of an overall schema of a culture of safety in cholecystectomy. When CVS cannot be attained there are several bailout strategies such a cholecystostomy or in the case of very severe inflammation discontinuation of the procedure and referral to a tertiary center for care. The most satisfactory bailout procedure is subtotal cholecystectomy of which there are two kinds. Subtotal fenestrating cholecystectomy removes the free wall of the gallbladder and ablates the mucosa but does not close the gallbladder remnant. Subtotal reconstituting cholecystectomy closes the gallbladder making a new smaller gallbladder. Such a gallbladder remnant is undesirable since it may become the site of new gallstone formation and recurrent symptoms . Both types may be done laparoscopically.”
Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 1995;180:101-25.
BASICS OF SURGICAL TECHNIQUE

This e-book was designed to assist in learning related to experimental surgical technique, during the training of health professionals. Concisely and objectively, it presents the basic principles for professional practice in surgery and in basic techniques of the most relevant surgical procedures. It is directed to the training of general practitioners, through the technical base, illustrated in procedures described step by step, with reference to the routines of the discipline of Surgical Technique, at the Federal University of Maranhão. It is not a work aimed at surgical clinic nor does it presuppose a descriptive detail that definitively supplies the necessary information for the execution of procedures in patients. This book is specially dedicated to undergraduate students, to serve as a guide during the Experimental Surgical Technique. It was designed and structured in order to facilitate theoretical study and encourage practical learning. Assisting your training, we seek professionals better prepared for health care.
Good Studies.
Laparoscopic Liver Resection
INTRODUCTION
Laparoscopic hepatic resection is an emerging option in the field of hepatic surgery. With almost 3000 laparoscopic hepatic resections reported in the literature for benign and malignant tumors, with a combined mortality of 0.3% and morbidity of 10.5%, there will be an increasing demand for minimally invasive liver surgery. Multiple series have been published on laparoscopic liver resections; however, no randomized controlled trial has been reported that compares laparoscopic with open liver resection. Large series, meta-analyses, and reviews have thus far attested to the feasibility and safety of minimally invasive hepatic surgery for benign and malignant lesions.
THECNICAL ASPECTS
The conversion rate from a laparoscopic approach to an open procedure was 4.1%. The most common type of laparoscopic liver resection performed is a wedge resection or segmentectomy (45%), followed by left lateral sectionectomy (20%). Major anatomic hepatectomies are still less frequently performed: right hepatectomy (9%) and left hepatectomy (7%). Cumulative morbidity and mortality was 10.5% and 0.3%.
BENEFITS OF LAPAROSCOPIC APPROACH
More importantly, almost all the studies comparing laparoscopic with open liver resection consistently showed a significant earlier discharge to home after laparoscopic liver resection. Lengths of stay were variable based on the country of origin of the studies but were consistently shorter for laparoscopic liver resection. Three studies published in the United States presented a length of stay of 1.9 to 4.0 days after laparoscopic liver resection. Studies from Europe showed an average length of stay of 3.5 to 10 days whereas those from Asia reported an average of length of stay of 4 to 20 days after laparoscopic liver resection.
COST ANALYSIS
Vanounou and colleagues used deviation-based cost modeling to compare the costs of laparoscopic with open left lateral sectionectomy at the University of Pittsburgh Medical Center. They compared 29 laparoscopic with 40 open cases and showed that patients who underwent the laparoscopic approach faired more favorably with a shorter length of stay (3 vs 5 days, P<.0001), significantly less postoperative morbidity (P 5 .001), and a weighted-average median cost savings of $1527 to $2939 per patient compared with patients who underwent open left lateral sectionectomy.
SURGICAL MARGINS
Initial concerns about the adequacy of surgical margins and possible tumor seeding prevented the widespread adoption of laparoscopic resection approaches for liver cancers. In comparison studies, there were no differences in margin-free resections between laparoscopic and open liver resection. In addition, no incidence of port-site recurrence or tumor seeding has been reported. With more than 3000 cases of minimally invasive hepatic resection reported in the literature (and no documentation of any significant port-site or peritoneal seeding), the authors conclude that this concern should not prevent surgeons from accepting a laparoscopic approach.
SURVIVAL OUTCOMES
There were no significant differences in overall survival in the 13 studies that compared laparoscopic liver resection with open liver resection for cancer. For example, Cai and colleagues showed that the 1-, 3-, and 5-year survival rates after laparoscopic resection of HCC were 95.4%, 67.5%, and 56.2% versus 100%, 73.8%, and 53.8% for open resection. For resection of colorectal cancer liver metastasis, Ito and colleagues showed a 3-year survival of 72% after laparoscopic liver resection and 56% after open liver resection whereas Castaing and colleagues51 showed a 5-year survival of 64% after laparoscopic liver resection versus 56% after open liver resection.
CONCLUSION
Compared with open liver resections, laparoscopic liver resections are associated with less blood loss, less pain medication requirement, and shorter length of hospital stay. A randomized controlled clinical trial is the best method to compare laparoscopic with open liver resection; however, such a trial may be difficult to conduct because patients are unlikely to subject themselves to an open procedure when a minimally invasive approach has been shown feasible and safe in experienced hands. In addition, many patients would have to be accrued to detect a difference in complications that occur infrequently. Short of a large randomized clinical trial, meta-analysis and matched comparisons provide the next best option to compare laparoscopic with open liver resection. For laparoscopic resection of HCC or colorectal cancer metastases, there has been no difference in 5-year overall survival compared with open hepatic resection. In addition, from a financial standpoint, the minimally invasive approach to liver resection may be associated with higher operating room costs; however, the total hospital costs were offset or improved due to the associated shorter length of hospital stay with the minimally invasive approach.
Medically-Necessary, Time Sensitive: (MeNTS) Score
Operating During The COVID-19 Coronavirus Pandemic
“At the University of Chicago, members of the Department of Surgery decided to investigate this issue more precisely. As stay-at-home restrictions in some states are easing, and as non-emergency medical care is being reconsidered, how does one possibly triage the thousands upon thousands of patients whose surgeries were postponed? Instead of the term “elective,” the University of Chicago’s Department of Surgery chose the phrase “Medically-Necessary, Time Sensitive” (MeNTS). This concept can be utilized to better assess the acuity and safety when determining which patients can get to the operating room in as high benefit/low risk manner as possible. And unlike in any recent time in history, risks to healthcare staff as well as risks to the patient from healthcare staff, are now thrown into the equation. The work was published in the April issue of the Journal of the American College of Surgeons.
On March 17, 2020, the American College of Surgeons recommended that all “elective” surgeries be canceled indefinitely. These guidelines were published, stating that only patients with “high acuity” surgical issues, which would include aggressive cancers and severely symptomatic disease, should proceed. Based on the Elective Surgery Acuity Scale (ESAS), most hospitals were strongly encouraged to cancel any surgery that was not high acuity, including slow-growing cancers, orthopedic and spine surgeries, airway surgeries, and any other surgeries for non-cancerous tumors. Heart surgeries for stable cardiac issues were also put on hold. Patients and surgeons waited. Some patients did, indeed undergo non-Covid-19-related surgeries. But most did not. Redeployment is gradually turning to re-entry.
The re-entry process for non-urgent (yet necessary) surgeries is a complicated one. Decisions and timing, based on a given hospital’s number and severity of Covid-19 patients, combined with a given city or state’s current and projected number of Covid-19 cases, how sick those patients will be, and whether or not a second surge may come, involves a fair amount of guesswork. As we have all seen, data manipulation has become a daily sparring match in many arenas. The authors of the study created an objective surgical risk scoring system, in order to help hospitals across this country, as well as others across the world, better identify appropriate timing regarding which surgeries can go ahead sooner rather than later, and why. They factored several variables into their equation, to account for the multiple potential barriers to care, including health and safety of hospital personnel. They created scoring systems based on three factors: Procedure, Disease and Patient Issues.
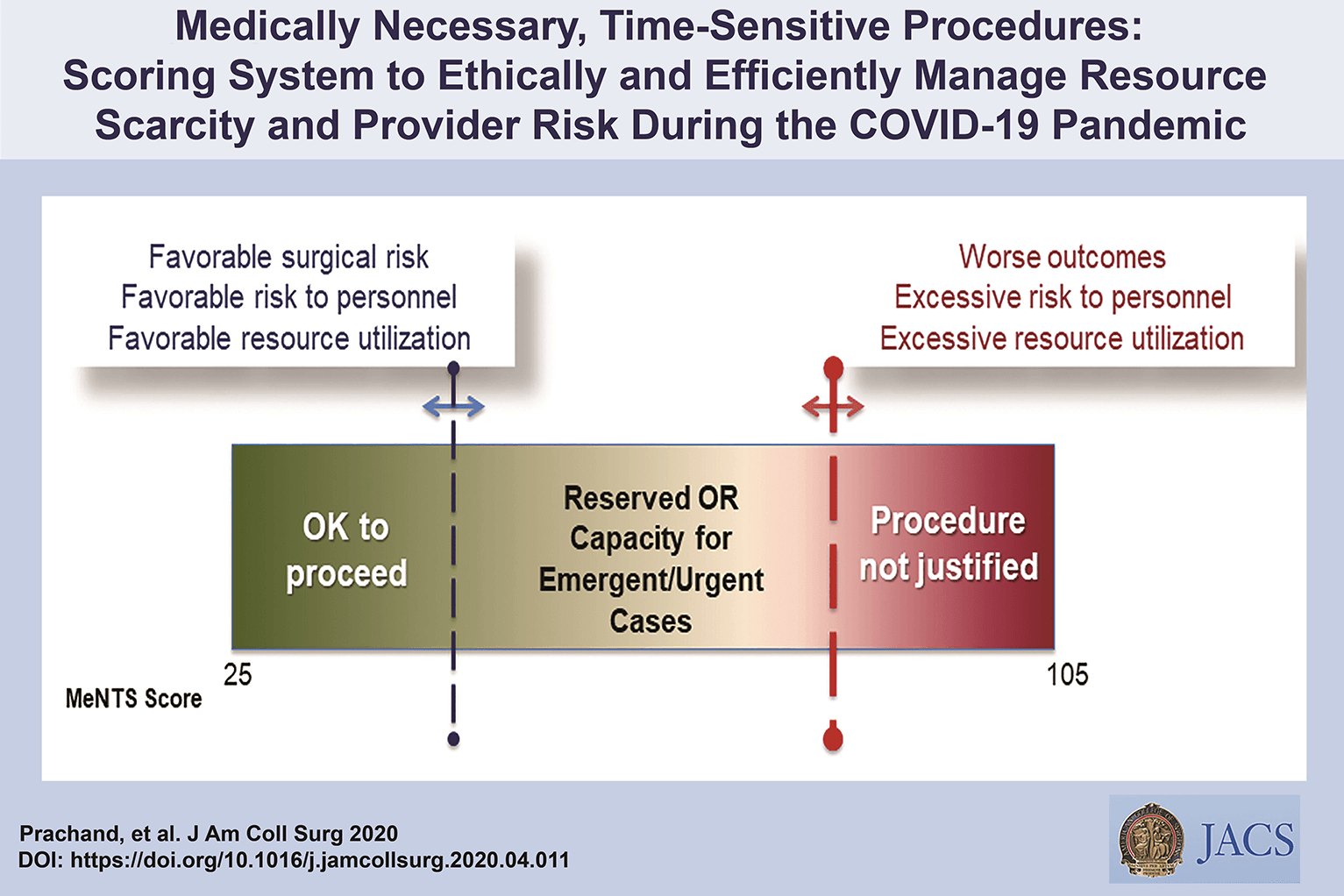
CALCULATE MeNTS SCORE HERE
The authors of the study created an objective surgical risk scoring system, in order to help hospitals across this country, as well as others across the world, better identify appropriate timing regarding which surgeries can go ahead sooner rather than later, and why. They factored several variables into their equation, to account for the multiple potential barriers to care, including health and safety of hospital personnel. Each patient would receive an overall conglomerate score, based on all of these factors, with the lower risks giving them more favorable scores to proceed with surgery soon, and the higher risks giving patients a higher score, or higher risk regarding proceeding with surgery, meaning it may be safest, for now, to wait.
Dr. Jeffrey Matthews, senior author of the paper, and Department Chair at the University of Chicago, stated that this model is reproducible across hospital systems, in urban, rural, and academic settings. And in the event of potential unpredictable surges of Covid-19 cases, the scoring system “helps prioritize cases not only from the procedure/disease standpoint but also from the pandemic standpoint with respect to available hospital resources such as PPE, blood, ICU beds, and [regular hospital] beds.”
The scoring system is extremely new, and the coming weeks will reveal how patients, surgeons and hospitals are faring as patients without life-and-death emergencies and/or Covid-19 complications gradually begin filling the operating rooms and hospital beds. In addition, and perhaps just as important, the study authors note that creating systems whereby healthcare resources, safety, and impact on outcomes need to be considered more carefully for each patient intervention, the larger impact of each intervention on public health will be better understood: not only for today’s pandemic, but also in future, as yet unknown, global events.”
Source: Nina Shapiro, 2020
Discover our surgical video channel and lectures associated with the surgeon blog.
Share and Join: https://linktr.ee/TheSurgeon
Covid-19 and Digestive Surgery
The current world Covid-19 pandemic has been the most discussed topic in the media and scientific journals. Fear, uncertainty, and lack of knowledge about the disease may be the significant factors that justify such reality. It has been known that the disease presents with a rapidly spreading, it is significantly more severe among the elderly, and it has a substantial global socioeconomic impact. Besides the challenges associated with the unknown, there are other factors, such as the deluge of information. In this regard, the high number of scientific publications, encompassing in vitro, case studies, observational and randomized clinical studies, and even systematic reviews add up to the uncertainty. Such a situation is even worse when considering that most healthcare professionals lack adequate knowledge to critically appraise the scientific method, something that has been previously addressed by some authors. Therefore, it is of utmost importance that expert societies supported by data provided by the World Health Organization and the National Health Department take the lead in spreading trustworthy and reliable information.
Discover our surgical video channel and lectures associated with the surgeon blog.
Share and Join: https://linktr.ee/TheSurgeon
#Medicine #Surgery #GeneralSurgery #DigestiveSurgery
#TheSurgeon #OzimoGama
Laparoscopic JEJUNOSTOMY
Many oncological patients with upper gastrointestinal (GI) tract tumours, apart from other symptoms, are malnourished or cachectic at the time of presentation. In these patients feeding plays a crucial role, including as part of palliative treatment. Many studies have proved the benefits of enteral feeding over parenteral if feasible. Depending on the tumour’s location and clinical stage there are several options of enteral feeding aids available. Since the introduction of percutaneous endoscopic gastrostomy (PEG) and its relatively easy application in most patients, older techniques such as open gastrostomy or jejunostomy have rather few indications.
The majority of non-PEG techniques are used in patients with upper digestive tract, head and neck tumours or trauma that renders the PEG technique unfeasible or unsafe for the patient. In these patients, especially with advanced disease requiring neoadjuvant chemotherapy or palliative treatment, open gastrostomy and jejunostomy were the only options of enteral access. Since the first report of laparoscopic jejunostomy by O’Regan et al. in 1990 there have been several publications presenting techniques and outcomes of laparoscopic feeding jejunostomy. Laparoscopic jejunostomy can accompany staging or diagnostic laparoscopy for upper GI malignancy when the disease appears advanced, hence avoiding additional anaesthesia and an operation in the near future.
In this video the author describe the technique of laparoscopic feeding jejunostomy applied during the staging laparoscopy in patient with advanced upper gastrointestinal tract cancer with co-morbid cachexy, requiring enteral feeding and neoadjuvant chemotherapy.
Welcome and get to know our Social Networks through the following link
Ozimo Gama’s Social Medias
#AnatomiaHumana #CirurgiaGeral #CirurgiaDigestiva #TheSurgeon
Traqueostomia
Basicamente, existem quatro situações que indicam a realização de traqueostomia: prevenção de lesões laringotraqueais pela intubação translaríngea prolongada; desobstrução da via aérea superior, em casos de tumores, corpo estranho ou infecção; acesso à via aérea inferior para aspiração e remoção de secreções; e aquisição de via aérea estável em paciente que necessita de suporte ventilatório prolongado.
A substituição do tubo endotraqueal pela cânula de traqueostomia ainda acrescenta benefícios, proporcionando conforto e segurança do paciente. Algumas sociedades americanas sugerem que a traqueostomia deva ser sempre considerada para pacientes que necessitarão de ventilação mecânica prolongada, ou seja, por mais de 14 dias.
Muitas vezes, a decisão de se realizar uma traqueostomia é tomada pelo julgamento clínico de médicos, principalmente aqueles que trabalham em unidades de terapia intensiva. Isso envolve a análise de múltiplos fatores, tais como as características de cada paciente, o motivo pelo qual ocorreu a intubação, doenças associadas, resposta ao trata-mento e prognóstico individualizado. Embora haja uma tendência de indicação de traqueostomia precoce em pacientes neurocríticos e com trauma grave.
Benefícios Clínicos:
- Diminuição do trabalho respiratório
- Melhora da aspiração das vias aéreas
- Permitir a fonação
- Permitir a alimentação por via oral
- Menor necessidade de sedação
- Redução do risco de pneumonia associada à ventilação
mecânica - Diminuição do tempo de ventilação mecânica
- Diminuição do tempo de internação em unidades de terapia
intensiva - Redução da mortalidade
Tratamento Cirúrgico do Abscesso Hepático Piogênico
Introdução
O abscesso hepático piogênico (AHP) é uma condição infecciosa grave caracterizada por uma coleção encapsulada de material purulento no fígado. Frequentemente, essa condição é resultante de infecções bacterianas, originárias do trato biliar ou de fontes intra-abdominais, como diverticulite. O manejo do AHP requer uma abordagem multidisciplinar, combinando diagnóstico rápido, antibioticoterapia e, em muitos casos, intervenção cirúrgica. No Brasil, a mortalidade associada a essa condição pode variar de 10% a 20%, sendo particularmente elevada em pacientes com comorbidades, como diabetes e cirrose. A presente revisão discute as abordagens cirúrgicas no tratamento do AHP, com ênfase nos critérios de intervenção, técnicas cirúrgicas e melhores práticas para o cirurgião do aparelho digestivo.
Diagnóstico e Classificação
O diagnóstico precoce do AHP é essencial para determinar a abordagem terapêutica mais adequada. Exames de imagem, como ultrassonografia (USG) e tomografia computadorizada (TC), são as ferramentas primárias para identificar a extensão da lesão e guiar a tomada de decisões. A classificação dos abscessos hepáticos baseia-se em seu tamanho e características morfológicas:
- Abscessos pequenos (menores que 3 cm) podem, muitas vezes, ser tratados com antibioticoterapia isolada.
- Abscessos maiores (geralmente >5 cm) e multiloculados exigem drenagem percutânea ou intervenção cirúrgica.
A etiologia do AHP no Brasil é predominantemente associada a bactérias como Escherichia coli e Klebsiella pneumoniae, e pacientes imunocomprometidos, como diabéticos, estão em maior risco de desenvolver complicações graves.
Abordagem Terapêutica
O tratamento do AHP é multimodal e deve ser adaptado à gravidade do caso, com o uso combinado de antibióticos, drenagem percutânea e intervenção cirúrgica, quando necessário. As diretrizes atuais propõem um algoritmo terapêutico baseado no tamanho e nas características dos abscessos.
1. Antibioticoterapia
A antibioticoterapia empírica deve ser iniciada imediatamente após o diagnóstico, visando cobertura para bactérias gram-negativas e anaeróbias. Ciprofloxacina ou cefixima combinadas com metronidazol são frequentemente utilizadas no manejo de abscessos hepáticos não complicados. A escolha do antibiótico deve ser ajustada conforme os resultados das culturas de sangue e de amostras do abscesso, garantindo uma abordagem personalizada.
2. Drenagem Percutânea
A drenagem percutânea, guiada por USG ou TC, é o tratamento de escolha para abscessos maiores que 3 cm e uniloculares (Tipo II). Esse método minimamente invasivo apresenta uma alta taxa de sucesso, próxima a 90%, sendo eficaz na maioria dos casos. No entanto, falhas podem ocorrer em abscessos multiloculados ou com conteúdo viscoso ou necrótico, situações em que a drenagem percutânea se torna inadequada, necessitando de intervenção cirúrgica.
3. Intervenção Cirúrgica
A cirurgia está indicada em abscessos multiloculados grandes (>3 cm, Tipo III), em abscessos que não respondem à drenagem percutânea ou na presença de complicações, como ruptura do abscesso. A cirurgia pode envolver drenagem minimamente invasiva ou ressecção hepática, dependendo da complexidade do abscesso e da experiência do cirurgião. Abscessos maiores que 10 cm apresentam maior risco de complicações, e nesses casos, a drenagem cirúrgica pode ser preferível. A laparotomia é recomendada em situações de peritonite ou quando o abscesso é de difícil acesso para drenagem percutânea.
4. Laparoscopia
A laparoscopia é uma alternativa minimamente invasiva à cirurgia aberta, indicada em abscessos uniloculares de tamanho moderado. Essa técnica oferece vantagens significativas, como menor tempo de internação e recuperação mais rápida, além de menor risco de complicações pós-operatórias.
Aplicação na Cirurgia Digestiva
O papel do cirurgião do aparelho digestivo é central no manejo dos abscessos hepáticos, especialmente em casos que requerem intervenção cirúrgica. A drenagem percutânea deve ser considerada a primeira linha de tratamento sempre que viável, mas o cirurgião deve estar preparado para realizar intervenções mais invasivas quando necessário. A laparoscopia tem demonstrado resultados promissores, reduzindo o tempo de internação e o risco de complicações. No Brasil, as infecções intra-abdominais complicadas são uma das principais causas de internação em emergências cirúrgicas, e o manejo adequado desses casos depende de uma sólida formação técnico-cirúrgica.
Algoritmo de Tratamento
Com base nas evidências disponíveis, um algoritmo de tratamento para o AHP pode ser delineado da seguinte forma:
- Abscessos pequenos (<3 cm, Tipo I): Tratamento com antibióticos isolados.
- Abscessos grandes uniloculares (>3 cm, Tipo II): Drenagem percutânea associada a antibioticoterapia.
- Abscessos grandes multiloculados (>3 cm, Tipo III): Intervenção cirúrgica.
Pontos-Chave
- Diagnóstico Precoce: O uso da TC com contraste é fundamental para o diagnóstico preciso do tamanho e da localização dos abscessos hepáticos, orientando a decisão terapêutica.
- Intervenção Cirúrgica: Abscessos multiloculados ou maiores que 5 cm frequentemente requerem intervenção cirúrgica, especialmente quando a drenagem percutânea falha.
- Abordagem Minimamente Invasiva: A laparoscopia oferece uma alternativa eficaz à cirurgia aberta, proporcionando uma recuperação mais rápida e com menor morbidade.
- Manejo Integral pelo Cirurgião Digestivo: O conhecimento técnico-cirúrgico é essencial para o manejo de abscessos hepáticos complexos, garantindo uma abordagem eficaz e personalizada.
Conclusão
O manejo do abscesso hepático piogênico exige uma abordagem multidisciplinar, sendo o cirurgião digestivo uma peça-chave no tratamento de casos complexos. A decisão entre drenagem percutânea e intervenção cirúrgica deve considerar múltiplos fatores, como o tamanho do abscesso, a resposta ao tratamento conservador e as condições clínicas do paciente. Como afirmou o Prof. Henri Bismuth: “Le traitement chirurgical n’est pas seulement une question de technique, mais de jugement. Le moment de l’intervention est aussi important que l’intervention elle-même.” Assim, o domínio técnico e a tomada de decisões precisas são fundamentais para o sucesso terapêutico no tratamento do AHP.
Gostou ❔Nos deixe um comentário ✍️, compartilhe em suas redes sociais e|ou mande sua dúvida pelo 💬 Chat On-line em nossa DM do Instagram.
#AbscessoHepatico #CirurgiaDigestiva #TratamentoAbscesso #DrenagemPercutanea #AparelhoDigestivo
Ebook: Princípios da Anatomia Topográfica
Os conceitos fundamentais da Anatomia Topográfica Humana através do estudo das regiões anatômicas com maior relevância Médico-Cirúrgica. Agora com amplo material multimídia disponibilizado através de acesso on-line dentro do livro e com isso creditamos que este trabalho será útil como mais uma ferramenta didática na preparação profissional dos estudantes de Medicina.
Link para Download
Fale Conosco
Ischaemic Preconditioning applied to LIVER SURGERY
- INTRODUCTION
The absence of oxygen and nutrients during ischaemia affects all tissues with aerobic metabolism. Ischaemia of these tissues creates a condition which upon the restoration of circulation results in further inflammation and oxidative damage (reperfusion injury). Restoration of blood flow to an ischaemic organ is essential to prevent irreversible tissue injury, however reperfusion of the organ or tissues may result in a local and systemic inflammatory response augmenting tissue injury in excess of that produced by ischaemia alone. This process of organ damage with ischaemia being exacerbated by reperfusion is called ischaemia-reperfusion (IR). Regardless of the disease process, severity of IR injury depends on the length of ischaemic time as well as size and pre-ischaemic condition of the affected tissue. The liver is the largest solid organ in the body, hence liver IR injury can have profound local and systemic consequences, particularly in those with pre-existing liver disease. Liver IR injury is common following liver surgery and transplantation and remains the main cause of morbidity and mortality.
2. AETIOLOGY
The liver has a dual blood supply from the hepatic artery (20%) and the portal vein (80%). A temporary reduction in blood supply to the liver causes IR injury. This can be due to a systemic reduction or local cessation and restoration of blood flow. Liver resections are performed for primary or secondary tumours of the liver and carry a substantial risk of bleeding especially in patients with chronic liver disease. Significant blood loss is associated with increased transfusion requirements, tumour recurrence, complications and increased morbidity and mortality. Several methods of hepatic vascular control have been described in order to minimise blood loss during elective liver resection. The simplest and most common method is inflow occlusion by applying a tape or vascular clamp across the hepatoduodenal ligament (Pringle Manoeuvre). This occludes both the arterial and portal vein inflow to the liver and leads to a period of warm ischaemia (37 °C) to the liver parenchyma resulting in ‘warm’ IR injury when the temporary inflow occlusion is relieved. In major liver surgery, extensive mobilisation of the liver itself without inflow occlusion results in a significant reduction in hepatic oxygenation.

3. PATOPHYSIOLOGY and RISK FACTORS
A complex cellular and molecular network of hepatocytes, Kupffer cells, liver sinusoidal endothelial cells (LSEC), leukocytes and cytokines play a role in the pathogenesis of IR injury. In general, both warm and cold ischaemia share similar mechanisms of injury. Hepatocyte injury is a predominant feature of warm ischaemia, whilst endothelial cells are more susceptible to cold ischaemic injury. There are currently no proven treatments for liver IR injury. Understanding this complex network is essential in developing therapeutic strategies in prevention and treatment of IR injury. Identifying risk factors for IR injury are extremely important in patient selection for liver surgery and transplantation. The main factors are the donor or patient age, the duration of organ ischaemia, presence or absence of liver steatosis and in transplantation whether the donor organ has been retrieved from a brain dead or cardiac death donor.
4. PREVENTION and TREATMENT
There is currently no accepted treatment for liver IR injury. Several pharmacological agents and surgical techniques have been beneficial in reducing markers of hepatocyte injury in experimental liver IR, however, they are yet to show clinical benefit in human trials. The following is an outline of current and future strategies which may be effective in reducing the detrimental effects of liver IR injury in liver surgery and transplantation.
4.1 SURGICAL STRATEGIES
Inflow occlusion or portal triad clamping (PTC) can be continuous or intermittent; alternating between short periods of inflow occlusion and reperfusion. Intermittent clamping (IC) increases parenchymal tolerance to ischaemia. Hence, prolonged continuous inflow occlusion rather than short intermittent periods results in greater degree of post-operative liver dysfunction. IC permits longer total ischaemia times for more complex resections. Alternating between 15 min of inflow occlusion and 5 min reperfusion cycles can be performed safely for up to 120 min total ischaemia time. There is a potential risk of increased blood loss during the periods of no inflow occlusion. However, these intervals provide an opportunity for the surgeon to check for haemostasis and control small bleeding areas from the cut surface of the liver. The optimal IC cycle times are not clear, although intermittent cycles of up to 30 min inflow occlusion have also been reported with no increase in morbidity, blood loss or liver dysfunction compared to 15 min cycles. IC is particularly beneficial in reducing post-operative liver dysfunction in patients with liver cirrhosis or steatosis.
In liver surgery, IPC ( Ischaemic Preconditioning) involves a short period of ischaemia (10 min) and reperfusion (10 min) intraoperatively by portal triad clamping prior to parenchymal transection during which a longer continuous inflow occlusion is applied to minimise blood loss. It allows continuous ischaemia times of up to 40 min without significant liver dysfunction. However, the protective effect of IPC decreases with increasing age above 60 years old and compared to IC it is less effective in steatotic livers. Moreover, IPC may impair liver regeneration capacity and may not be tolerated by the small remnant liver in those with more complex and extensive liver resections increasing the risk of post-operative hepatic insufficiency.
In order to avoid direct ischaemic insult to the liver by inflow occlusion, remote ischaemic preconditioning (RIPC) has been used. RIPC involves preconditioning a remote organ prior to ischaemia of the target organ. It has been shown to be reduce warm IR injury to the liver in experimental studies. A recent pilot randomised trial of RIPC in patients undergoing major liver resection for colorectal liver metastasis used a tourniquet applied to the right thigh with 10 min cycles of inflation-deflation to induce IR injury to the leg for 60 min. This was performed after general anaesthesia prior to skin incision. A reduction in post-operative transaminases and improved liver function was shown without the use of liver inflow occlusion. These results are promising but require validation in a larger trial addressing clinical outcomes.
5. FUTURE PERSPECTIVES
Hepatic IR injury remains the main cause of morbidity and mortality in liver surgery and transplantation. Despite over two decades of research in this area, therapeutic options to treat or prevent liver IR are limited. This is primarily due to the difficulties in translation of promising agents into human clinical studies. Recent advances in our understanding of the immunological responses and endothelial dysfunction in the pathogenesis of liver IR injury may pave the way for the development of new and more effective and targeted pharmacological agents.
Femoral Hernia REPAIR
Femoral hernia is not as common as inguinal hernia. It is often associated with incarceration or strangulation, resulting in peritonitis and mortality.
ANATOMY

The pelvicrural interval (the opening from the abdomen to the thigh) is divided into two spaces: a lateral space, the lacuna musculosa, through which the iliopsoas muscles pass; and a medial space, the lacuna vasculosa, for the femoral vessels. The external iliac vessels run along the anterior surface of the iliopsoas muscle in the pelvis, pass between the iliopubic tract and Cooper’s ligament, and finally course beneath the inguinal ligament to become the femoral vessels. Where the external iliac vessels run down into the lacuna vasculosa, transversalis fascia covers the vessels to form the femoral sheath. It extends approximately 4 cm caudally and ends as the adventitia of the femoral vessels. The medial compartment of the femoral sheath is called the femoral canal, which is ordinarily less than 2 cm in diameter and contains lymphatic vessels and glands. The true opening of the femoral canal is a musculoaponeurotic ring, consisting of Cooper’s ligament inferiorly, the femoral vein laterally, and iliopubic tract superiorly and medially. In the past, the medial border of the femoral ring was for the lacunar ligament. The lacunar ligament is an attachment of the inguinal ligament to the pubic bone, however, and lies in the outer layer of the transversalis fascia.
McVay demonstrated that the medial boundary of the femoral ring is the lateral edge of the aponeurosis of the insertion of the transversus abdominis muscle with transversalis fascia onto the pectin of the pubis, not the lacunar ligament. Condon also demonstrated that the iliopubic tract bridges the femoral canal and then curves posteriorly and inferiorly, its fibers spreading fanwise to insert adjacent to Cooper’s ligament into a broad area of the superior ramus of the pubis. Thus, the true inner ring of the femoral canal is bounded by the iliopubic tract anteriorly and medially, and by Cooper’s ligament posteriorly. If a surgeon incises the inguinal ligament in a tightly incarcerated femoral hernia, he or she will find that the hernia cannot be reduced because of the more deeply placed ring. The distal orifice has a rigid boundary—surrounded by the lacunar ligament medially; the inguinal ligament superiorly; and the fascia of the pectineal muscle—and is usually less than 1 cm in diameter. The rigidity of these structures is the reason why strangulation often occurs in femoral hernias.
ETIOLOGY
Currently, the ‘‘acquired’’ theory is widely accepted; however, the true cause of femoral hernia is not known. McVay demonstrated that the width of the femoral ring, which is determined by the length of the fanwise insertion of the iliopubic tract to Cooper’ ligament, is the main etiologic factor of the femoral hernia. Considering that the femoral hernia is very rare in children and most common in elderly women, however, McVay’s concept cannot be the only reason for the occurrence of femoral hernia. Nyhus noted the presence of a relatively large femoral defect without an accompanying femoral hernia during the preperitoneal approach. This may be caused by the acquired weakness of the transversalis fascia and a consequent predisposition to the development of the femoral hernia.
INCIDENCE
The ratio of femoral hernia relative to all groin hernias is reported to be 2% to 8% in adults . Femoral hernias are very rare in children, and most commonly observed between the ages of 40 and 70. The peak distribution is in the 50s, with a slight decrease in the 60s and 70s. As for sex distribution, femoral hernia is 4 to 5 times more common in female than in male; however, there are some reports that it is more common in men than in women. A right-sided presentation is more common than left, but the reason is not known.
TREATMENT
Finally, femoral hernia is usually thought of as requiring emergency surgical treatment. Only 30% of our cases were treated as emergency operations, however, whereas 70% were elective. Unless patients complain of severe abdominal pain or ileus, surgeons need not perform emergency operations. In summary, the mesh plug hernia repair for femoral hernia has resulted in a reduced recurrence rate, shortened hospital stay, and a low rate of postoperative complications.
Perioperative Fluid Management

In the setting of a normal ejection fraction, fluid is only administered when the expectation is that cardiac output will increase, and vasopressors are utilized if the aforementioned devices show fluid will not increase cardiac output. Excess fluid in certain general surgical cases can cause ileus and bowel edema, and in cardiac cases, it can cause hemodilution. Patients randomized to restricted and liberal fluid resuscitation strategies found a clear linear relationship between total fluids administered (and weight gain) and complications following colorectal surgery including pulmonary edema and tissue-healing complications. Further multiple studies exist demonstrating fewer complications with normovolemia than with liberal strategies of fluid resuscitation.
It must be understood that goal-directed therapy does, in no way, mean reduction in fluid administration. For some procedures, it may be necessary to administer more than anticipated fluid volumes (orthopedics), while for others, the opposite may be true (abdominal). Normovolemia is important to maintain perfusion without volume overload. Thus, the idea behind goaldirected therapy is to maintain zero fluid balance coupled with minimal weight gain or loss. Hypovolemia is associated with reduced circulating blood volume, decreased renal perfusion, altered coagulation, microcirculation compromise, and endothelial dysfunction, among other processes. Hypervolemia is associated with splanchnic edema, decreased pulmonary gas exchange secondary to pulmonary edema, impaired wound healing, anastomotic dehiscence, decreased mobility, altered coagulation, and endothelial dysfunction, amidst others processes.
Classroom: Perioperative Medicine
From a recent Cochrane review, there is no evidence that colloids are superior to crystalloid for resuscitation in patients. Therefore, crystalloid fluids should generally be the primary intravenous fluid during the perioperative course. In cardiac surgery, the utilization of 0.9% normal saline solution was associated with hyperchloremia and poor postoperative outcomes, including higher length of stay and increased mortality.118 Further, a more balanced crystalloid, such as Plasma-Lyte, was associated with improved outcomes in 22,851 surgical patients. In this study, there was a 2.05 odds ratio predictor of mortality with normal saline. Other complications such as acute kidney injury, gastrointestinal complications, major hemorrhage, and major infection were also increased in the group of
patients that were hyperchloremic after normal saline administration. Based on such evidence, it would seem prudent to proceed with a more balanced solution, such as PlasmaLyte, to reduce complications.
A especialização e a busca pela excelência

“Onde quer que a arte de curar é amada, também há um amor pela humanidade.” — Hipócrates
A especialização em órgãos e o volume de casos têm sido temas centrais nos últimos anos, revelando uma relação direta entre alto volume de procedimentos e melhores desfechos, conforme evidenciado pela literatura recente. Estudos mostram que a concentração de procedimentos de alto risco, como esofagectomias, pancreatectomias e ressecções hepáticas, em centros especializados pode reduzir significativamente a mortalidade pós-operatória anual. Embora procedimentos como tireoidectomias e ressecções do cólon mostrem um efeito semelhante, mas em menor escala, a redução da mortalidade pós-operatória em 5% pode ser tão eficaz quanto tratamentos adjuvantes tóxicos e deve ser uma prioridade na busca pela mais alta qualidade em cirurgia oncológica e digestiva. Além da redução da morbidade e mortalidade, há evidências de que a especialização pode levar a melhores resultados funcionais e financeiros. Às vezes, a atenção excessiva aos números anuais obscurece o fato de que hospitais menores, com equipes dedicadas, também podem alcançar bons resultados. É provável que não apenas o volume, mas também o treinamento e a especialização resultem em melhores desfechos. Definir um número absoluto de casos pode ser improdutivo e desviar a atenção de fatores essenciais, como reuniões multidisciplinares organizadas, infraestrutura adequada e disponibilidade de técnicas modernas.
O Foco na Otimização do Processo
O foco deve ser direcionado para a análise e otimização de todo o processo de diagnóstico e tratamento, já que este processo pode colocar o paciente em grave risco, especialmente durante o período hospitalar. A prevenção de erros tem recebido atenção significativa, levando ao surgimento do conceito de segurança do paciente. Desde a publicação do relatório To Err Is Human pelo Institute of Medicine, a abordagem para erros mudou drasticamente.
Em vez de focar exclusivamente no indivíduo, a abordagem sistêmica considera as condições em que as pessoas trabalham e tenta construir defesas para mitigar os efeitos dos erros. O modelo de queijo suíço ilustra bem essa abordagem: várias camadas de defesa, cada uma com suas falhas, são colocadas em torno de um procedimento. As falhas ativas e condições latentes criam buracos em cada camada. Em vez de apenas fechar os buracos na última camada de defesa, redesenhar o processo e fechar um buraco em uma camada anterior pode ser mais eficaz.
A análise de causa raiz é essencial para identificar pontos fracos no procedimento. Um exemplo é a colocação incorreta de uma colostomia após uma resseção abdominoperineal. Em vez de culpar o residente por não selecionar a posição correta durante a cirurgia ou marcar o ponto errado no dia anterior, uma solução mais eficaz seria o treinamento adequado do junior ou a marcação do ponto certo por um terapeuta de estomas durante a clínica ambulatorial.
A marcação do local correto no corpo tornou-se uma medida de segurança e o paciente deve ser instruído a exigir essa prática para sua própria segurança. É crucial eliminar a cultura de ‘culpa e vergonha’ e promover um ambiente mais aberto, onde erros e quase erros possam ser relatados. O clima de segurança em um departamento cirúrgico pode ser medido de forma validada e é um elemento essencial para uma cultura onde a segurança do paciente possa prosperar.
O Cuidado com os Detalhes e a Otimização de Resultados
A atenção meticulosa a cada detalhe durante o período pré-operatório e clínico pode reduzir eventos adversos. O que é chamado de “primeira vez em risco” deve ser considerado. Há também exemplos de ações para otimizar resultados que são mais específicas para o câncer. Por exemplo, o uso de técnicas que estimulam a cicatrização de feridas após uma resseção abdominoperineal, como a omentoplastia ou o retal abdominal flap, pode evitar atrasos no tratamento adjuvante para câncer retal.
A atenção cuidadosa à cicatrização de feridas em sarcoma pode evitar o adiamento da necessária radioterapia adjuvante. Omissão de uma tomografia computadorizada com contraste contendo iodo no diagnóstico de câncer de tireoide pode possibilitar um tratamento radioativo com iodo mais precoce, resultando em possíveis melhores resultados. A coleta de um número suficiente de linfonodos em câncer de cólon pode evitar discussões sobre a indicação de quimioterapia adjuvante.
A maioria dos exemplos de segurança do paciente no período clínico está relacionada ao uso ótimo de tratamento multimodal ou aos efeitos gerais da cirurgia. Às vezes, é necessário equilibrar o risco de aceitar um procedimento cirúrgico mais extenso, com uma morbidade mais alta, para alcançar um melhor resultado a longo prazo. O oposto também é possível, quando um bom resultado de curto prazo de uma excisão local em câncer retal deve ser equilibrado com uma maior taxa de recorrência local. A garantia de qualidade para todas as disciplinas participantes (diagnósticas e terapêuticas) é um elemento chave na configuração de ensaios clínicos prospectivos e randomizados.
“A prática é a maior professora, e o mais sábio cirurgião é aquele que aprende a valorizar o conhecimento não apenas pela sua acumulação, mas pela sua aplicação.” — William Osler
Principles of Surgical Resection of Hepatocellular Carcinoma
INTRODUCTION
There has been significant improvement in the perioperative results following liver resection, mainly due to techniques that help reduce blood loss during the operation. Extent of liver resection required in HCC for optimal oncologic results is still controversial. On this basis, the rationale for anatomically removing the entire segment or lobe bearing the tumor, would be to remove undetectable tumor metastases along with the primary tumor.
SIZE OF TUMOR VERSUS TUMOR FREE-MARGIN
Several retrospective studies and meta-analyses have shown that anatomical resections are safe in patients with HCC and liver dysfunction, and may offer a survival benefit. It should be noted, that most studies are biased, as non-anatomical resections are more commonly performed in patients with more advanced liver disease, which affects both recurrence and survival. It therefore remains unclear whether anatomical resections have a true long-term survival benefit in patients with HCC. Some authors have suggested that anatomical resections may provide a survival benefit in tumors between 2 and 5 cm. The rational is that smaller tumors rarely involve portal structures, and in larger tumors presence of macrovascular invasion and satellite nodules would offset the effect of aggressive surgical approach. Another important predictor of local recurrence is margin status. Generally, a tumor-free margin of 1 cm is considered necessary for optimal oncologic results. A prospective randomized trial on 169 patients with solitary HCC demonstrated that a resection margin aiming at 2 cm, safely decreased recurrence rate and improved long-term survival, when compared to a resection margin aiming at 1 cm. Therefore, wide resection margins of 2 cm is recommended, provided patient safety is not compromised.
THECNICAL ASPECTS
Intraoperative ultrasound (IOUS) is an extremely important tool when performing liver resections, specifically for patients with HCC and compromised liver function. IOUS allows for localization of the primary tumor, detection of additional tumors, satellite nodules, tumor thrombus, and define relationship with bilio-vascular structures within the liver. Finally, intraoperative US-guided injection of dye, such as methylene-blue, to portal branches can clearly define the margins of the segment supplied by the portal branch and facilitate safe anatomical resection.
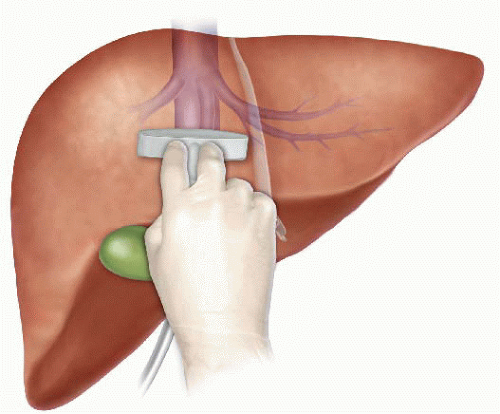
The anterior approach to liver resection is a technique aimed at limiting tumor manipulation to avoid tumoral dissemination, decrease potential for blood loss caused by avulsion of hepatic veins, and decrease ischemia of the remnant liver caused by rotation of the hepatoduodenal ligament. This technique is described for large HCCs located in the right lobe, and was shown in a prospective, randomized trial to reduce frequency of massive bleeding, number of patients requiring blood transfusions, and improve overall survival in this setting. This approach can be challenging, and can be facilitated by the use of the hanging maneuver.

Multiple studies have demonstrated that blood loss and blood transfusion administration are significantly associated with both short-term perioperative, and long-term oncological results in patients undergoing resection for HCC. This has led surgeons to focus on limiting operative blood loss as a major objective in liver resection. Transfusion rates of <20 % are expected in most experienced liver surgery centers. Inflow occlusion, by the use of the Pringle Maneuver represents the most commonly performed method to limit blood loss. Cirrhotic patients can tolerate total clamping time of up to 90 min, and the benefit of reduced blood loss outweighs the risks of inflow occlusion, as long as ischemia periods of 15 min are separated by at least 5 min of reperfusion. Total ischemia time of above 120 min may be associated with postoperative liver dysfunction. Additional techniques aimed at reducing blood loss include total vascular isolation, by occluding the inferior vena cava (IVC) above and below the liver, however, the hemodynamic results of IVC occlusion may be significant, and this technique has a role mainly in tumors that are adjacent to the IVC or hepatic veins.

Anesthesiologists need to assure central venous pressure is low (below 5 mmHg) by limiting fluid administration, and use of diuretics, even at the expense 470 N. Lubezky et al. of low systemic pressure and use of inotropes. After completion of the resection, large amount of crystalloids can be administered to replenish losses during parenchymal dissection.
LAPAROSCOPIC RESECTIONS
Laparoscopic liver resections were shown to provide benefits of reduced surgical trauma, including a reduction in postoperative pain, incision-related morbidity, and shorten hospital stay. Some studies have demonstrated reduced operative bleeding with laparoscopy, attributed to the increased intra-abdominal pressure which reduces bleeding from the low-pressured hepatic veins. Additional potential benefits include a decrease in postoperative ascites and ascites-related wound complications, and fewer postoperative adhesions, which may be important in patients undergoing salvage liver transplantation. There has been a delay with the use of laparoscopy in the setting of liver cirrhosis, due to difficulties with hemostasis in the resection planes, and concerns for possible reduction of portal flow secondary to increased intraabdominal pressure. However, several recent studies have suggested that laparoscopic resection of HCC in patients with cirrhosis is safe and provides improved outcomes when compared to open resections.

Resections of small HCCs in anterior or left lateral segments are most amenable for laparoscopic resections. Larger resections, and resection of posterior-sector tumors are more challenging and should only be performed by very experienced surgeons. Long-term oncological outcomes of laparoscopic resections was shown to be equivalent to open resections on retrospective studies , but prospective studies are needed to confirm these findings. In recent years, robotic-assisted liver resections are being explored. Feasibility and safety of robotic-assisted surgery for HCC has been demonstrated in small non-randomized studies, but more experience is needed, and long-term oncologic results need to be studied, before widespread use of this technique will be recommended.
ALPPS: Associating Liver Partition with Portal vein ligation for Staged hepatectomy
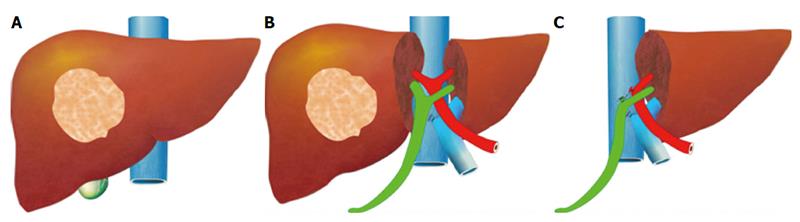
The pre-operative options for inducing atrophy of the resected part and hypertrophy of the FLR, mainly PVE, were described earlier. Associating Liver Partition with Portal vein ligation for Staged hepatectomy (ALPPS) is another surgical option aimed to induce rapid hypertrophy of the FLR in patients with HCC. This technique involves a 2-stage procedure. In the first stage splitting of the liver along the resection plane and ligation of the portal vein is performed, and in the second stage, performed at least 2 weeks following the first stage, completion of the resection is performed. Patient safety is a major concern, and some studies have reported increased morbidity and mortality with the procedure. Few reports exist of this procedure in the setting of liver cirrhosis. Currently, the role of ALPPS in the setting of HCC and liver dysfunction needs to be better delineated before more widespread use is recommended.
Anatomia Cirúrgica Hepática
O Mapa Fundamental para Ressecções e Transplantes
Autor: Prof. Dr. Ozimo Gama
Categoria: Cirurgia Hepatobiliar / Anatomia Aplicada / Transplante Hepático Tempo de Leitura: 12 minutos
“Um bom conhecimento da anatomia do fígado é um pré-requisito para a cirurgia moderna do fígado.” — H. Bismuth
Introdução
O fígado, o maior órgão sólido do corpo humano (representando 2-3% do peso corporal), é uma estrutura de complexidade arquitetônica fascinante. Para o cirurgião geral, e imperativamente para o cirurgião hepatobiliar, o domínio da anatomia hepática transcende a memorização de nomes; trata-se de compreender as relações tridimensionais que ditam a segurança de uma hepatectomia e o sucesso de um transplante. Neste artigo, dissecaremos a anatomia hepática sob uma ótica cirúrgica, indo além da morfologia externa para explorar a segmentação funcional e as nuances vasculares vitais para a prática operatória de excelência.
1. Meios de Fixação e Mobilização Cirúrgica
O fígado é envolto pela cápsula de Glisson e peritônio, exceto na “área nua” diafragmática e no hilo. Seus ligamentos não são apenas estruturas de sustentação, mas marcos anatômicos cruciais para a mobilização segura do órgão:
-
Ligamentos Coronários e Triangulares: A mobilização destes permite a exposição da veia cava inferior (VCI) e das veias hepáticas.
-
Ligamento Venoso (Arantius): Remanescente do ducto venoso fetal. Sua dissecção é uma manobra chave. Ao isolá-lo, o cirurgião ganha acesso ao tronco das veias hepáticas esquerda e média, facilitando o controle vascular em hepatectomias esquerdas ou transplantes.
-
Ligamento Hepatocaval (Makuuchi): Uma estrutura fibrosa (por vezes contendo parênquima) que fixa o lobo caudado à veia cava. Sua divisão cuidadosa é obrigatória para expor a veia hepática direita e para a mobilização completa do lobo direito em transplantes intervivos.
2. A Revolução de Couinaud
A anatomia clássica, que dividia o fígado em lobos direito, esquerdo, quadrado e caudado baseada apenas em marcos externos (como o ligamento falciforme), é insuficiente para a cirurgia moderna. A verdadeira divisão funcional segue a Linha de Cantlie, um plano imaginário que vai do leito da vesícula biliar à veia cava inferior. Esta linha divide o fígado em metades funcionalmente independentes (Direita e Esquerda), cada uma com sua própria irrigação arterial, portal e drenagem biliar.
Adotamos a Segmentação de Couinaud (1954), que organiza o fígado em 8 segmentos baseados na distribuição das veias hepáticas e pedículos portais:
-
Fígado Direito (Setores Anterior e Posterior): Segmentos V, VIII (Anterior) e VI, VII (Posterior).
-
Fígado Esquerdo: Segmentos II, III (Lateral) e IV (Medial).
-
Lobo Caudado (Segmento I): Uma entidade autônoma. Localizado dorsalmente, recebe sangue de ambos os ramos portais (direito e esquerdo) e drena diretamente na VCI através de veias curtas. Esta drenagem direta confere ao caudado uma “proteção” relativa em casos de Síndrome de Budd-Chiari, onde ele frequentemente se hipertrofia.
3. O Hilo Hepático e a Tríade Portal
A dissecção do hilo exige precisão milimétrica, especialmente em transplantes com doador vivo (LDLT). As estruturas da tríade portal seguem uma organização anteroposterior constante que guia o cirurgião:
-
Ducto Biliar: Mais ventral (anterior) e lateral.
-
Artéria Hepática: Medial e na camada intermédia.
-
Veia Porta: A estrutura mais dorsal (posterior).
Variações Vasculares Importantes
-
Artéria Hepática: A anatomia “clássica” (artéria hepática comum saindo do tronco celíaco) está presente em apenas 60% dos casos. Variações críticas incluem a Artéria Hepática Direita Substituída (da Mesentérica Superior), que passa posterior à veia porta, e a Artéria Hepática Esquerda Substituída (da Gástrica Esquerda). O não reconhecimento pode levar à necrose do enxerto ou isquemia biliar.
-
Veia Porta: Variações na bifurcação, como a ausência do tronco principal da veia porta direita (trifurcação), exigem reconstruções complexas em transplantes.
4. Drenagem Venosa: O Escoamento
As três veias hepáticas principais (Direita, Média e Esquerda) correm nas fissuras intersegmentares:
-
Veia Hepática Direita (RHV): Drena o setor posterior. É a maior veia.
-
Veia Hepática Média (MHV): Corre na fissura principal (Linha de Cantlie). Fundamental para a drenagem dos segmentos V e VIII. Em transplantes de lobo direito, a gestão dos tributários da MHV é crítica para evitar congestão do enxerto.
-
Veias Acessórias: Cerca de metade da população possui veias hepáticas acessórias inferiores (drenando os segmentos VI e VII diretamente na cava). Se calibrosas (>5mm), devem ser reimplantadas para garantir a função do enxerto.
5. A Via Biliar e sua Vascularização: O “Tendão de Aquiles”
A anatomia biliar é a mais variável e propensa a complicações.
-
Irrigação Biliar: Diferente do parênquima, os ductos biliares extra-hepáticos são irrigados exclusivamente por um plexo arterial peribiliar (artérias das 3h e 9h), derivado principalmente da artéria hepática direita e retroduodenal.
-
Pérola Cirúrgica: Durante a captação do fígado, a dissecção excessiva do ducto biliar pode desvascularizá-lo, levando a estenoses isquêmicas tardias. Preservar a bainha peribiliar e o tecido hilar é mandatório.
6. A Vesícula Biliar e o Triângulo de Calot
Embora a colecistectomia seja um procedimento comum, ela exige respeito absoluto à anatomia. O Triângulo de Calot (delimitado pelo ducto cístico, ducto hepático comum e borda hepática) é a zona de segurança. A artéria cística deve ser identificada aqui. Variações, como um ducto cístico curto ou inserção no ducto direito, ou uma artéria hepática direita tortuosa (“Hump”) invadindo o triângulo, são armadilhas para o cirurgião desatento.
Conclusão
A cirurgia hepática evoluiu de ressecções em cunha não anatômicas para segmentectomias precisas e transplantes de doadores vivos. Essa evolução foi sustentada por um aprofundamento do conhecimento anatômico. Para o cirurgião em formação, o estudo exaustivo destas estruturas, suas variações e suas relações vasculares não é apenas acadêmico — é a base ética para oferecer segurança e cura aos pacientes portadores de doenças hepatobiliares.
Gostou ❔Nos deixe um comentário ✍️ , compartilhe em suas redes sociais e|ou mande sua dúvida pelo 💬 Chat On-line em nossa DM do Instagram.
Hashtags: #AnatomiaHepatica #CirurgiaDoFigado #TransplanteHepatico #Couinaud #CirurgiaHPB
Pringle Maneuver
After the first major hepatic resection, a left hepatic resection, carried out in 1888 by Carl Langenbuch, it took another 20 years before the first right hepatectomy was described by Walter Wendel in 1911. Three years before, in 1908, Hogarth Pringle provided the first description of a technique of vascular control, the portal triad clamping, nowadays known as the Pringle maneuver. Liver surgery has progressed rapidly since then. Modern surgical concepts and techniques, together with advances in anesthesiological care, intensive care medicine, perioperative imaging, and interventional radiology, together with multimodal oncological concepts, have resulted in fundamental changes. Perioperative outcome has improved significantly, and even major hepatic resections can be performed with morbidity and mortality rates of less than 45% and 4% respectively in highvolume liver surgery centers. Many liver surgeries performed routinely in specialized centers today were considered to be high-risk or nonresectable by most surgeons less than 1–2 decades ago.Interestingly, operative blood loss remains the most important predictor of postoperative morbidity and mortality, and therefore vascular control remains one of the most important aspects in liver surgery.
“Bleeding control is achieved by vascular control and optimized and careful parenchymal transection during liver surgery, and these two concepts are cross-linked.”
First described by Pringle in 1908, it has proven effective in decreasing haemorrhage during the resection of the liver tissue. It is frequently used, and it consists in temporarily occluding the hepatic artery and the portal vein, thus limiting the flow of blood into the liver, although this also results in an increased venous pressure in the mesenteric territory. Hemodynamic repercussion during the PM is rare because it only diminishes the venous return in 15% of cases. The cardiovascular system slightly increases the systemic vascular resistance as a compensatory response, thereby limiting the drop in the arterial pressure. Through the administration of crystalloids, it is possible to maintain hemodynamic stability.

In the 1990s, the PM was used continuously for 45 min and even up to an hour because the depth of the potential damage that could occur due to hepatic ischemia was not yet known. During the PM, the lack of oxygen affects all liver cells, especially Kupffer cells which represent the largest fixed macrophage mass. When these cells are deprived of oxygen, they are an endless source of production of the tumour necrosis factor (TNF) and interleukins 1, 6, 8 and 10. IL 6 has been described as the cytokine that best correlates to postoperative complications. In order to mitigate the effects of continuous PM, intermittent clamping of the portal pedicle has been developed. This consists of occluding the pedicle for 15 min, removing the clamps for 5 min, and then starting the manoeuvre again. This intermittent passage of the hepatic tissue through ischemia and reperfusion shows the development of hepatic tolerance to the lack of oxygen with decreased cell damage. Greater ischemic tolerance to this intermittent manoeuvre increases the total time it can be used.
Management of gallbladder cancer

Gallbladder cancer is uncommon disease, although it is not rare. Indeed, gallbladder cancer is the fifth most common gastrointestinal cancer and the most common biliary tract cancer in the United States. The incidence is 1.2 per 100,000 persons per year. It has historically been considered as an incu-rable malignancy with a dismal prognosis due to its propensity for early in-vasion to liver and dissemination to lymph nodes and peritoneal surfaces. Patients with gallbladder cancer usually present in one of three ways: (1) advanced unresectable cancer; (2) detection of suspicious lesion preoperatively and resectable after staging work-up; (3) incidental finding of cancer during or after cholecystectomy for benign disease.
SURGICAL MANAGEMENT
Although, many studies have suggested improved survival in patients with early gallbladder cancer with radical surgery including en bloc resection of gallbladder fossa and regional lymphadenectomy, its role for those with advanced gallbladder cancer remains controversial. First, patients with more advanced disease often require more extensive resections than early stage tumors, and operative morbidity and mortality rates are higher. Second, the long-term outcomes after resection, in general, tend to be poorer; long-term survival after radical surgery has been reported only for patients with limited local and lymph node spread. Therefore, the indication of radical surgery should be limited to well-selected patients based on thorough preoperative and intra-operative staging and the extent of surgery should be determined based on the area of tumor involvement.
Surgical resection is warranted only for those who with locoregional disease without distant spread. Because of the limited sensitivity of current imaging modalities to detect metastatic lesions of gallbladder cancer, staging laparoscopy prior to proceeding to laparotomy is very useful to assess the
abdomen for evidence of discontinuous liver disease or peritoneal metastasis and to avoid unnecessary laparotomy. Weber et al. reported that 48% of patients with potentially resectable gallbladder cancer on preoperative imaging work-up were spared laparotomy by discovering unresectable disease by laparoscopy. Laparoscopic cholecystectomy should be avoided when a preoperative cancer is suspected because of the risk of violation of the plane between tumor and liver and the risk of port site seeding.
The goal of resection should always be complete extirpation with microscopic negative margins. Tumors beyond T2 are not cured by simple cholecystectomy and as with most of early gallbladder cancer, hepatic resection is always required. The extent of liver resection required depends upon whether involvement of major hepatic vessels, varies from segmental resection of segments IVb and V, at minimum to formal right hemihepatectomy or even right trisectionectomy. The right portal pedicle is at particular risk for advanced tumor located at the neck of gallbladder, and when such involvement is suspected, right hepatectomy is required. Bile duct resection and reconstruction is also required if tumor involved in bile duct. However, bile duct resection is associated with increased perioperative morbidity and it should be performed only if it is necessary to clear tumor; bile duct resection does not necessarily increase the lymph node yield.
Hepatic Surgery: Portal Vein Embolization

INTRODUCTION
Portal vein Embolizations (PVE) is commonly used in the patients requiring extensive liver resection but have insufficient Future Liver Remanescent (FLR) volume on preoperative testing. The procedure involves occluding portal venous flow to the side of the liver with the lesion thereby redirecting portal flow to the contralateral side, in an attempt to cause hypertrophy and increase the volume of the FLR prior to hepatectomy.
PVE was first described by Kinoshita and later reported by Makuuchi as a technique to facilitate hepatic resection of hilar cholangiocarcinoma. The technique is now widely used by surgeons all over the world to optimize FLR volume before major liver resections.
PHYSIOPATHOLOGY
PVE works because the extrahepatic factors that induce liver hypertrophy are carried primarily by the portal vein and not the hepatic artery. The increase in FLR size seen after PVE is due to both clonal expansion and cellular hypertrophy, and the extent of post-embolization liver growth is generally proportional to the degree of portal flow diversion. The mechanism of liver regeneration after PVE is a complex phenomenon and is not fully understood. Although the exact trigger of liver regeneration remains unknown, several studies have identified periportal inflammation in the embolized liver as an important predictor of liver regeneration.

THECNICAL ASPECTS
PVE is technically feasible in 99% of the patients with low risk of complications. Studies have shown the FLR to increase by a median of 40–62% after a median of 34–37 days after PVE, and 72.2–80% of the patients are able to undergo resection as planned. It is generally indicated for patients being considered for right or extended right hepatectomy in the setting of a relatively small FLR. It is rarely required before extended left hepatectomy or left trisectionectomy, since the right posterior section (segments 6 and 7) comprises about 30% of total liver volume.
PVE is usually performed through percutaneous transhepatic access to the portal venous system, but there is considerable variability in technique between centers. The access route can be ipsilateral (portal access at the same side being resected) with retrograde embolization or contralateral (portal access through FLR) with antegrade embolization. The type of approach selected depends on a number of factors including operator preference, anatomic variability, type of resection planned, extent of embolization, and type of embolic agent used. Many authors prefer ipsilateral approach especially for right-sided tumors as this technique allows easy catheterization of segment 4 branches when they must be embolized and also minimizes the theoretic risk of injuring the FLR vasculature or bile ducts through a contralateral approach and potentially making a patient ineligible for surgery.
However, majority of the studies on contralateral PVE show it to be a safe technique with low complication rate. Di Stefano et al. reported a large series of contralateral PVE in 188 patients and described 12 complications (6.4%) only 6 of which could be related to access route and none precluded liver resection. Site of portal vein access can also change depending on the choice of embolic material selected which can include glue, Gelfoam, n-butyl-cyanoacrylate (NBC), different types and sizes of beads, alcohol, and nitinol plus. All agents have similar efficacy and there are no official recommendations for a particular type of agent.
RESULTS
Proponents of PVE believe that there should be very little or no tumor progression during the 4–6 week wait period for regeneration after PVE. Rapid growth of the FLR can be expected within the first 3–4 weeks after PVE and can continue till 6–8 weeks. Results from multiple studies suggest that 8–30% hypertrophy over 2–6 weeks can be expected with slower rates in cirrhotic patients. Most studies comparing outcomes after major hepatectomy with and without preoperative PVE report superior outcomes with PVE. Farges et al. demonstrated significantly less risk of postoperative complications, duration of intensive care unit, and hospital stay in patients with cirrhosis who underwent right hepatectomy after PVE compared to those who did not have preoperative PVE. The authors also reported no benefit of PVE in patients with a normal liver and FLR >30%. Abulkhir et al. reported results from a meta-analysis of 1088 patients undergoing PVE and showed a markedly lower incidence of Post Hepatectomy Liver Failure (PHLF) and death compared to series reporting outcomes after major hepatectomy in patients who did not undergo PVE. All patients had FLR volume increase, and 85% went on to have liver resection after PVE with a PHLF incidence of 2.5% and a surgical mortality of 0.8%. Several studies looking at the effect of systemic neoadjuvant chemotherapy on the degree of hypertrophy after PVE show no significant impact on liver regeneration and growth.
VOLUMETRIC RESPONSE

The volumetric response to PVE is also a very important factor in understanding the regenerative capacity of a patient’s liver and when used together with FLR volume can help identify patients at risk of poor postsurgical outcome. Ribero et al. demonstrated that the risk of PHLF was significantly higher not only in patients with FLR ≤ 20% but also in patients with normal liver who demonstrated ≤5% of FLR hypertrophy after PVE. The authors concluded that the degree of hypertrophy >10% in patients with severe underlying liver disease and >5% in patients with normal liver predicts a low risk of PHLF and post-resection mortality. Many authors do not routinely offer resection to patients with borderline FLR who demonstrate ≤5% hypertrophy after PVE.
Predicting LIVER REMNANT Function
Careful analysis of outcome based on liver remnant volume stratified by underlying liver disease has led to recommendations regarding the safe limits of resection. The liver remnant to be left after resection is termed the future liver remnant (FLR). For patients with normal underlying liver, complications, extended hospital stay, admission to the intensive care unit, and hepatic insufficiency are rare when the standardized FLR is >20% of the TLV. For patients with tumor-related cholestasis or marked underlying liver disease, a 40% liver remnant is necessary to avoid cholestasis, fluid retention, and liver failure. Among patients who have been treated with preoperative systemic chemotherapy for more than 12 weeks, FLR >30% reduces the rate of postoperative liver insufficiency and subsequent mortality.
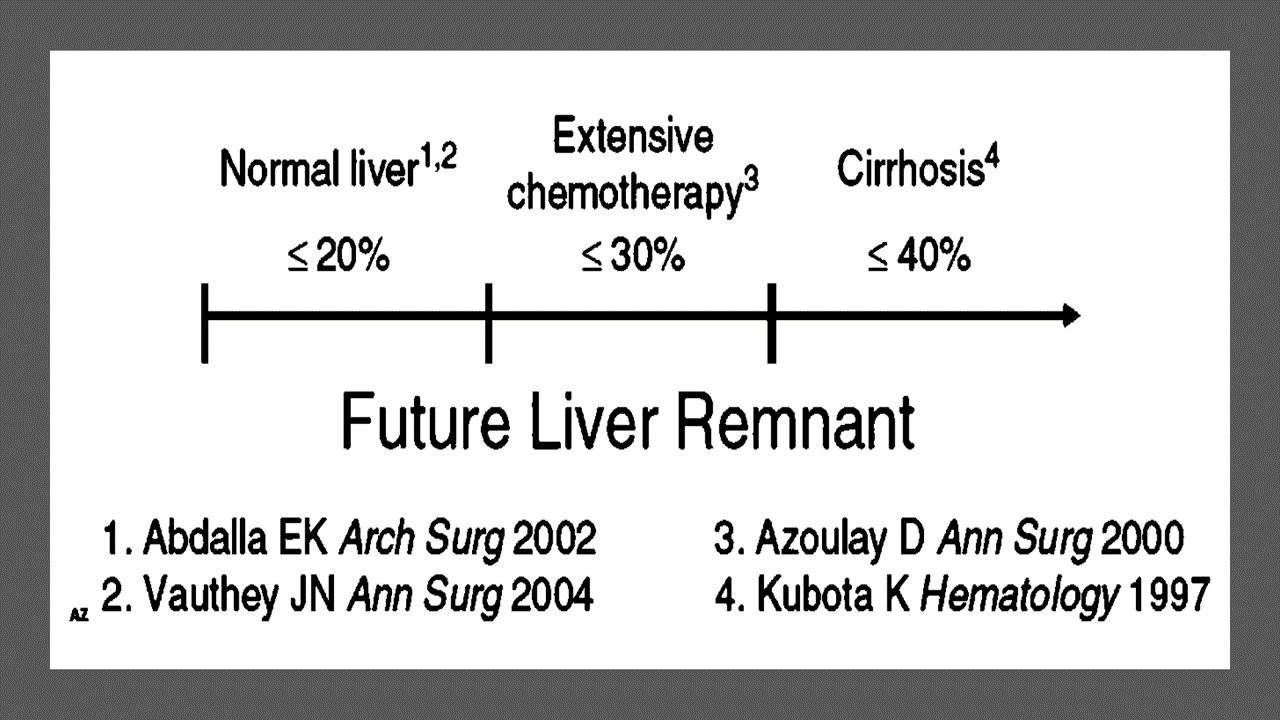
When the liver remnant is normal or has only mild disease, the volume of liver remnant can be measured directly and accurately with threedimensional computed tomography (CT) volumetry. However, inaccuracy may arise because the liver to be resected is often diseased, particularly in patients with cirrhosis or biliary obstruction. When multiple or large tumors occupy a large volume of the liver to be resected, subtracting tumor volumes from liver volume further decreases accuracy of CT volumetry. The calculated TLV, which has been derived from the association between body surface area (BSA) and liver size, provides a standard estimate of the TLV. The following formula is used:
TLV (cm3) = –794.41 + 1267.28 × BSA (square meters)
Thus, the standardized FLR (sFLR) volume calculation uses the measured FLR volume from CT volumetry as the numerator and the calculated TLV as the denominator: Standardized FLR (sFLR) = measured FLR volume/TLV Calculating the standardized TLV corrects the actual liver volume to the individual patient’s size and provides an individualized estimate of that patient’s postresection liver function. In the event of an inadequate FLR prior to major hepatectomy, preoperative liver preparation may include portal vein embolization (PVE).
Classroom: Principles of Hepatic Surgery
Videos of Surgical Procedures

This page provides links to prerecorded webcasts of surgical procedures. These are actual operations performed at medical centers in the Brazil. Please note that you cannot send in questions by email, though the webcast may say that you can, because you are not seeing these videos live. The videos open in a second window. If you have a pop-up blocker, you will need to disable it to view the programs.
Videos of Surgical Procedures
Strangulation in GROIN HERNIAS
Importance
Declining Mortality Rates
In both the UK and the USA, the annual death rate due to inguinal and femoral hernias has significantly decreased over the past two to three decades. In the UK, deaths from these hernias declined by 22% to 55% between 1975 and 1990. Similarly, in the USA, the annual deaths per 100,000 population for patients with hernia and intestinal obstruction decreased from 5.1 in 1968 to 3.0 in 1988. For patients with obstructed inguinal hernias, 88% underwent surgery, with a remarkably low mortality rate of 0.05%. These improvements suggest that elective groin hernia surgery has played a crucial role in reducing overall mortality rates.
Elective Surgery and Strangulation Rates
Supporting this observation, the USA has lower rates of strangulation compared to the UK, possibly due to the threefold higher rate of elective hernia surgeries in the USA. Nevertheless, statistics indicate that the rate of elective hernia surgeries in the USA per 100,000 population decreased from 358 to 220 between 1975 and 1990, although this may be an artifact of data collection rather than a genuine decline.
Mortality Analysis from UK and Denmark Studies
During 1991–1992, the UK National Confidential Enquiry Into Perioperative Deaths investigated 210 deaths following inguinal hernia repair and 120 deaths following femoral hernia repair. This inquiry, which focuses on the quality of surgery, anesthesia, and perioperative care, found that many patients were elderly (45 were aged 80–89 years) and significantly infirm; 24 were ASA grade III and 21 ASA grade IV. The majority of postoperative mortality was attributed to preexisting cardiorespiratory issues.
A nationwide study in Denmark of 158 patients who died after acute groin hernia repair by Kjaergaard et al. also found that these patients were old (median age 83 years) and frail (>80% with significant comorbidity), with frequent delays in diagnosis and treatment. These findings highlight the need for high-quality care by experienced surgeons and anesthetists, especially for patients with high ASA grades.
Postoperative Care Recommendations
Postoperative care for these patients should occur in a high-dependency unit or intensive therapy unit. This might necessitate transferring selected patients to appropriate hospitals and facilities. Decisions about interventional surgery should be made in consultation with the relatives of extremely elderly, frail, or moribund patients, adopting a humane approach that may rule out surgery.
Emergency Admissions and Prioritization
Forty percent of patients with femoral hernias are admitted as emergency cases with strangulation or incarceration, while only 3% of patients with direct inguinal hernias present with strangulation. This disparity has implications for prioritizing patients on waiting lists when these hernias present electively in outpatient clinics.
Risk of Strangulation
A groin hernia is at its greatest risk of strangulation within three months of onset. For inguinal hernias, the cumulative probability of strangulation is 2.8% at three months after presentation, rising to 4.5% after two years. The risk is much higher for femoral hernias, with a 22% probability of strangulation at three months, rising to 45% at 21 months. Right-sided hernias have a higher strangulation rate than left-sided hernias, potentially due to anatomical differences in mesenteric attachment. The decline in hernia-related mortality in both the UK and USA underscores the importance of elective hernia surgery. Ensuring timely surgery, especially for high-risk femoral hernias, and providing high-quality perioperative care for elderly and frail patients are crucial steps in further reducing mortality and improving patient outcomes.
Evidence-Based Medicine
In a randomized trial, evaluating an expectative approach to minimally symptomatic inguinal hernias, Fitzgibbons et al. in the group of patients randomized to watchful waiting found a risk of an acute hernia episode of 1.8 in 1,000 patient years. In another trial, O’Dwyer and colleagues, randomizing patients with painless inguinal hernias to observation or operation, found two acute episodes in 80 patients randomized to observation. In both studies, a large percentage of patients randomized to nonoperative care were eventually operated due to symptoms. Neuhauser, who studied a population in Columbia where elective herniorrhaphy was virtually unobtainable, found an annual rate of strangulation of 0.29% for inguinal hernias.
Management of Strangulation
The diagnosis of hernias is primarily based on clinical symptoms and signs, supplemented by imaging studies when necessary. Pain at the hernia site is a constant symptom. In cases of obstruction with intestinal strangulation, patients may present with colicky abdominal pain, distension, vomiting, and constipation. Physical examination may reveal signs of dehydration, with or without central nervous system depression, especially in elderly patients with uremia, along with abdominal signs of intestinal obstruction.
Femoral hernias can be easily missed, particularly in obese women, making a thorough physical examination essential for an accurate diagnosis. However, physical examination alone is often insufficient to confirm the presence of a strangulated femoral hernia versus lymphadenopathy or a lymph node abscess. In such cases, urgent radiographic studies, such as ultrasound or CT scan, may be necessary.
The choice of incision depends on the type of hernia if the diagnosis is clear. When there is doubt, a half Pfannenstiel incision, 2 cm above the pubic ramus extending laterally, provides adequate access to all types of femoral or inguinal hernias. The fundus of the hernia sac is exposed, and an incision is made to assess the viability of its contents. If nonviability is detected, the transverse incision should be converted into a laparotomy incision, followed by the release of the constricting hernia ring, reduction of the sac’s contents, resection, and reanastomosis. Precautions must be taken to avoid contamination of the general peritoneal cavity by gangrenous bowel or intestinal contents.
In most cases, once the constriction of the hernia ring is released, circulation to the intestine is restored, and viability returns. The intestine that initially appears dusky or non-peristaltic may regain color with a short period of warming with damp packs. If viability is doubtful, resection should be performed. Resection rates are highest for femoral or recurrent inguinal hernias and lowest for simple inguinal hernias. Other organs, such as the bladder or omentum, should be resected as needed.
After peritoneal lavage and formal closure of the laparotomy incision, specific repair of the hernia should be performed. Prosthetic mesh should not be used in a contaminated operative field due to the high risk of wound infection. Hernia repair should follow the general principles of elective hernia repair. It is important to remember that in this predominantly frail and elderly patient group with a high postoperative mortality risk, the primary objective of the operation is to stop the vicious cycle of strangulation, with hernia repair being a secondary objective.
Key Point
The risk of an acute groin hernia episode is of particular relevance, when discussing indication for operation of painless or minimally symptomatic hernias. A sensible approach in groin hernias would be, in accordance with the guidelines from the European Hernia Society to advise a male patient, that the risk of an acute operation, with an easily reducible (“disappears when lying down”) inguinal hernia with little or no symptoms, is low and that the indication for operation in this instance is not absolute, but also inform, that usually the hernia after some time will cause symptoms, eventually leading to an operation. In contrast, female patients with a groin hernia, due to the high frequency of femoral hernias and a relatively high risk of acute hernia episodes, should usually be recommended an operation.
Wound Healing

There are many local and systemic factors that affect wound healing. The physician should be actively working to correct any abnormality that can prevent or slow wound healing.
Local Factors
A health care provider can improve wound healing by controlling local factors. He or she must clean the wound, debride it, and close it appropriately. Avulsion or crush wounds below under general management of wounds) need to be debrided until all nonviable tissue is removed. Grossly contaminated wounds should be cleaned as completely as possible to remove particulate matter (foreign bodies) and should be irrigated copiously. Bleeding must be controlled to prevent hematoma formation, which is an excellent medium for bacterial growth. Hematoma also separates wound edges, preventing the proper contact of tissues that is necessary for healing.
Radiation affects local wound healing by causing vasculitis, which leads to local hypoxia and ischemia. Hypoxia and ischemia impede healing by reducing the amount of nutrients and oxygen that are available at the wound site. Infection decreases the rate of wound healing and detrimentally affects proper granulation tissue formation, decreases oxygen delivery, and depletes the wound of needed nutrients. Care must be taken to clean the wound adequately. All wounds have some degree of contamination, if the body is able to control bacterial proliferation in a wound, that wound will heal. The use of cleansing agents (the simplest is soap and water) can help reduce contamination. A wound that contains the highly virulent streptococci species should not be closed. Physicians should keep in mind the potential for Clostridium tetani in wounds with devitalized tissue and use the proper prophylaxis.
Systemic Factors
In addition to controlling local factors, the physician must address systemic issues that can affect wound healing. Nutrition is an extremely important factor in wound healing. Patients need adequate nutrition to support protein synthesis, collagen formation, and metabolic energy for wound healing. Patients need adequate vitamins and nutrients to facilitate healing; folic acid is critical to the proper formation of collagen. Adequate fat intake is required for the absorption of vitamins D, A, K, and E. Vitamin K is essential for the
carboxylation of glutamate in the synthesis of clotting factors II, VII, IX, and X. Decreasing clotting factors can lead to hematoma formation and altered wound healing. Vitamin A increases the inflammatory response, increases collagen synthesis, and increases the influx of macrophages into a wound. Magnesium is required for protein synthesis, and zinc is a cofactor for RNA and DNA polymerase. Lack of any one of these vitamins or trace elements will adversely affect wound healing. Uncontrolled diabetes mellitus results in uncontrolled hyperglycemia, impairs wound healing, and alters collagen
formation. Hyperglycemia also inhibits fibroblast and endothelial cell proliferation within the wound. Medications will also affect wound healing. For example, steroids blunt the inflammatory response, decrease the available vitamin A in the wound, and alter the deposition and remodeling of collagen. Chronic illness (immune deficiency, cancer, uremia, liver disease, and jaundice) will predispose to infection, protein deficiency, and malnutrition, which, as noted previously, can affect wound healing. Smoking has a systemic effect by decreasing the oxygencarrying capacity of hemoglobin. Smoking may also decrease collagen formation within a wound. Hypoxia results in a decrease in oxygen delivery to a wound and retards healing.
Abdominal Surgical Anatomy

The abdomen is the lower part of the trunk below the diaphragm. Its walls surround a large cavity called the abdominal cavity. The abdominal cavity is much more extensive than what it appears from the outside. It extends upward deep to the costal margin up to the diaphragm and downward within the bony pelvis. Thus, a considerable part of the abdominal cavity is overlapped by the lower part of the thoracic cage above and by the bony pelvis below. The abdominal cavity is subdivided by the plane of the pelvic inlet into a larger upper part, i.e., the abdominal cavity proper, and a smaller lower part, i.e., the pelvic cavity. Clinically the importance of the abdomen is manifold. To the physician, the physical examination of the patient is never complete until he/she thoroughly examines the abdomen. To the surgeon, the abdomen remains an enigma because in number of cases the cause of abdominal pain and nature of abdominal lump remains inconclusive even after all possible investigations. To summarize, many branches of medicine such as general surgery and gastroenterology are all confined to the abdomen.
Classroom: Abdominal Surgical Anatomy
Minimally Invasive Approach to Choledocholithiasis
Introduction
The incidence of choledocholithiasis in patients undergoing cholecystectomy is estimated to be 10 %. The presence of common bile duct stones is associated with several known complications including cholangitis, gallstone pancreatitis, obstructive jaundice, and hepatic abscess. Making the diagnosis early and prompt management is crucial. Traditionally, when choledocholithiasis is identified with intraoperative cholangiography during the cholecystectomy, it has been managed surgically by open choledochotomy and place- ment of a T-tube. This open surgical approach has a morbidity rate of 10–15 %, mortality rate of <1 %, with a <6 % incidence of retained stones. Patients who fail endoscopic retrieval of CBD stones, as well as cases in which an endoscopic approach is not appropriate, should be explored surgically.
Clinical Manifestation
Acute obstruction of the bile duct by a stone causes a rapid distension of the biliary tree and activation of local pain fibers. Pain is the most common presenting symptom for choledocholithiasis and is localized to either the right upper quadrant or to the epigastrium. The obstruction will also cause bile stasis which is a risk factor for bacterial over- growth. The bacteria may originate from the duodenum or the stone itself. The combination of biliary obstruction and colo- nization of the biliary tree will lead to the development of fevers, the second most common presenting symptom of cho- ledocholithiasis. Biliary obstruction, if unrelieved, will lead to jaundice. When these three symptoms (pain, fever, and jaundice) are found simultaneously, it is known as Charcot’s triad. This triad suggests the diagnosis of acute ascending cholangitis, a potentially life-threatening condition. If not treated promptly, this can lead to hypotension and decreased metal status, both signs of severe sepsis. When combined with Charcot’s triad, this constellation of symptoms is commonly referred to as Reynolds pentad.
Laparoscopic common bile duct exploration
Laparoscopic common bile duct exploration (LCBDE) allows for single stage treatment of gallstone disease, reducing overall hospital stay, improving safety and cost-effectiveness when compared to the two-stage approach of ERCP and laparoscopic cholecystectomy. Bile duct clearance can be confirmed by direct visualization with a choledochoscope. But, before the advent of choledochoscope, bile duct clearance was uncertain, and blind instrumentation of the duct resulted in accentuated edema and inflammation. Due to advancement in instruments, optical magnification, and direct visualization, laparoscopic exploration of the CBD results in fewer traumas to the bile duct. This has led to an increasing tendency to close the duct primarily, reducing the need for placement of T-tubes. Still, laparoscopic bile duct exploration is being done in only a few centers. Apart from the need for special instruments, there is also a significant learning curve to acquire expertise to be able to perform a laparoscopic bile duct surgery.
Morbidity and mortality rates of laparoscopic exploration are comparable to ERCP (2–17 and 1–5 %), and there is no clear difference in primary success rates between the two approaches. However, the endoscopic approach may be preferable for elderly and frail patients, who are at higher risk with surgery. Patients older than 70–80 years of age have a 4–10 % mortality rate with open duct exploration. It may be as high as 20 % in elderly patients undergoing urgent procedures. In comparison, advanced age and comor- bidities do not have a significant impact on overall complication rates for ERCP. A success rate of over 90 % has been reported with laparoscopic CBD exploration. Availability of surgical expertise and appropriate equipment affect the success rate of laparoscopic exploration, as does the size, number of the CBD stones, as well as biliary anatomy. Over the years, laparoscopic exploration has become efficient, safe, and cost effective. Complications include CBD laceration, stricture formation, bile leak, abscess, pancreatitis, and retained stones.
In cases of failure of laparoscopic CBD exploration, a guidewire or stent can be passed through the cystic duct, common bile duct, and through the ampulla into the duodenum followed by cholecystectomy. This makes the identification and cannulation of the ampulla easier during the post- operative ERCP. Laparoscopic common bile duct exploration is traditionally performed through a transcystic or transductal approach. The transcystic approach is appropriate under certain circumstances. These include a small stone (<10 mm) located in the CBD, presence of small common bile duct (<6 mm), or if there is poor access to the common duct. The transductal approach is preferable in cases of large stones, stones in proximal ducts (hepatic ducts), large occluding stones in a large duct, presence of multiple stones, or if the cystic duct is small (<4 mm) or tortuous. Contraindications for laparoscopic approach include lack of training, and severe inflammation in the porta hepatis making the exploration difficult and risky.
Key Points
With advancement in imaging technology, laparoscopic and endoscopic techniques, management of common bile duct stone has changed drasti- cally in recent years. This has made the treatment of this condition safe and more efficient. Many options are now available to manage this condition, and any particular modality for treatment should be chosen carefully based on the patient related factors, institutional protocol, available expertise, resources, and cost-effectiveness.
Classroom: M.I.A. of Choledocholithiasis
Management of Complicated Appendicitis: Open or Laparoscopic Surgery?
Patients with acute appendicitis can present at different stages of the disease process, ranging from mild mucosal inflammation to frank perforation with abscess formation. The reported overall incidence of acute appendicitis varies with age, gender, and geographical differences. Interestingly, while the incidence of non-perforated appendicitis in the United States decreased between 1970 and 2004, no significant decline in the rate of perforated appendicitis was observed despite the increasng use of computed tomography (CT) and fewer negative appendectomies.
Of 32,683 appendectomies sampled from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) hospitals between 2005 and 2008, 5,405 patients (16.5%) had a preoperative diagnosis of acute appendicitis with peritonitis/abscess.
The definition of complicated appendicitis varies slightly in the literature. Clinicopathological diagnoses (gangrenous, perforated, appendiceal abscess/phlegmon) of acute appendicitis are commonly used for its definition. Classically, patients at the extremes of age are more likely to present with complicated appendicitis. Similarly, pre-morbid conditions including diabetes and type of medical insurance are significantly associated with the risk of perforation.
The importance of early appendectomy has also been emphasized to prevent perforation of the appendix and the sub- sequent negative impact on patient outcomes. However, more recent meta-analysis data supports the safety of a relatively short (12–24 h) delay before appendectomy, which was not significantly associated with increased rate of complicated appendicitis. Teixeira et al. also showed that the time to appendectomy was not a significant risk factor for perforated appendicitis but did result in a significantly increased risk of surgical site infection.
The outcome of patients with complicated appendicitis is significantly worse than patients with uncomplicated appendicitis. A population-based study from Sweden showed that, in a risk-adjusted model, patients with perforated appendicitis were 2.34 times more likely to die after appendectomy than non- perforated appendicitis patients. Because of its higher mortality and morbidity in patients with complicated appendicitis, the management of complicated appendicitis has evolved significantly over the last few decades.
Open or Laparoscopic Surgery
Since the first laparoscopic appendectomy was described by Semm in 1983, multiple studies have compared operative time, complication rates, length of hospital stay, hospital cost, and other outcomes between open and laparoscopic appendectomy for acute appendicitis. The most recent Cochrane review included 67 studies showing that laparoscopic appendectomy was associated with a lower incidence of wound infection, reduced postoperative pain, shorter postoperative length of hospital stay, and faster recovery to daily activity. In contrast, reduced risk of intra-abdominal abscesses and shorter operative time were found as the advantages of open appendectomy.
Due to increased surgeon experience in uncomplicated appendicitis, laparoscopic appendectomy is more frequently attempted even in complicated appendicitis cases as an alternative approach to open appendectomy. Although the general surgical steps for complicated appendicitis are similar to those for uncomplicated appendicitis, the laparoscopic procedure can be more technically demanding. Therefore, conversion from laparoscopic appendectomy to open appendectomy can be expected.
Despite these concerns, the laparoscopic approach in patients with com- plicated appendicitis has been proven to be safe and comparable to open appendectomy. Retrospective studies using a large database in the United States uniformly showed more favorable clinical outcomes (mortality, morbidity, length of hospital stay, readmission rate) and hospital costs in patients who underwent laparoscopic appendectomy when compared to open appendectomy. The real risk of developing an intra- abdominal abscess after laparoscopic appendectomy remains unclear. A meta-analysis by Markides et al. found no significant difference in the intra-abdominal abscess rate between laparoscopic and open appendectomy for complicated appendicitis, whereas Ingraham et al. showed a higher likelihood of developing an organ-space surgical site infection in patients undergoing laparoscopic appendectomy.
How to Choose a Mesh in Hernia Repair

Since the introduction of polypropylene (PP) mesh for hernia repair, surgeons continue to discuss the use of mesh in a variety of settings for one of the most common operations performed by general surgeons—hernia repair. This discussion has involved raw materials, cost, and outcomes and for many years referred to only a few products, as manufacturing was limited. Nowadays, with multiple permanent, absorbable, biologic, and hybrid products on the market, the choice of mesh for a hernia repair can be daunting. Increasing clinical complexity further emphasizes the need for individualizing care, but more frequently, hospital supply chain personnel institute product procurement procedures for cost control, limiting mesh choice for surgeons. This can force surgeons into a “one-size-fits-all” practice regarding mesh choice, which may not be ideal for some patients. Conversely, current literature lacks definitive evidence supporting the use of one mesh over another, a fact that has not escaped the radar screen of the hospital supply chain and mesh industry, both of which attempt to limit vendor and mesh choice for financial gain. It is unlikely that this type of “proof” will ever come to fruition. This leaves us with choosing a mesh based on an algorithm that is centered on the patient and the patient’s unique clinical scenario.
Article: Mesh in Hernia Repair
Modern Concepts of Pancreatic Surgery
 Operations on the gallbladder and bile ducts are among the surgical procedures most commonly performed by general surgeons. In most hospitals, cholecystectomy is the most frequently performed operation within the abdomen. Pancreatic surgery is less frequent , but because of the close relation between the biliary system and the pancreas, knowledge of pancreatic problems is equally essential to the surgeon. Acute and chronic pancreatitis and cancer of the pancreas are often encountered by surgeons, with apparently increasing frequency; their treatment remains difficult and perplexing. This review demonstrates the modern aspects of pancreatic surgery. Good study.
Operations on the gallbladder and bile ducts are among the surgical procedures most commonly performed by general surgeons. In most hospitals, cholecystectomy is the most frequently performed operation within the abdomen. Pancreatic surgery is less frequent , but because of the close relation between the biliary system and the pancreas, knowledge of pancreatic problems is equally essential to the surgeon. Acute and chronic pancreatitis and cancer of the pancreas are often encountered by surgeons, with apparently increasing frequency; their treatment remains difficult and perplexing. This review demonstrates the modern aspects of pancreatic surgery. Good study.
AULA: PRÍNCIPIOS MODERNOS DA CIRURGIA PANCREÁTICA
FERIDA PÓS-OPERATÓRIA

A avaliação e os cuidados de feridas pós-operatórias deve ser do domínio de todos os profissionais que atuam na clínica cirúrgica. O conhecimento a cerca dos processos relacionados a cicatrização tecidual é importante tanto nos cuidados como na prevenção de complicações, tais como: infecções e deiscência. Como tal, todos os profissionais médicos, sendo eles cirurgiões ou de outras especialidades, que participam do manejo clínico dos pacientes no período perioperatório devem apreciar a fisiologia da cicatrização de feridas e os princípios de tratamento de feridas pós-operatório. O objetivo deste artigo é atualizar os profissionais médicos de outras especialidades sobre os aspectos importantes do tratamento de feridas pós-operatório através de uma revisão da fisiologia da cicatrização de feridas, os métodos de limpeza e curativo, bem como um guia sobre complicações de feridas pós-operatórias mais prevalentes e como devem ser manejados nesta situação.
Causas de conversão da VIDEOCOLECISTECTOMIA
Atualmente, a colecistectomia laparoscópica é a abordagem preferida para o tratamento da litíase biliar, representando cerca de 90% dos procedimentos realizados, uma marca alcançada nos Estados Unidos em 1992. A popularidade dessa técnica se deve a suas vantagens evidentes: menos dor no pós-operatório, recuperação mais rápida, redução dos dias de trabalho perdidos e menor tempo de hospitalização. Apesar de ser considerada o padrão-ouro na cirurgia biliar, a colecistectomia laparoscópica não está isenta de desafios. Entre 2% e 15% dos casos podem exigir a conversão para cirurgia convencional. Os motivos mais comuns para essa conversão incluem dificuldades na identificação da anatomia, suspeita de lesão da árvore biliar e controle de sangramentos. Identificar os fatores que contribuem para uma maior taxa de conversão é essencial para a equipe cirúrgica. Isso não apenas permite uma avaliação mais precisa da complexidade do procedimento, mas também ajuda na preparação do paciente para possíveis riscos e na mobilização de cirurgiões mais experientes quando necessário. Em um cenário onde a precisão e a segurança são cruciais, a compreensão dos desafios e a preparação adequada podem fazer toda a diferença no resultado da cirurgia.
Relacionados ao Paciente: 1. Obesidade (IMC > 35), 2. Sexo Masculino, 3. Idade > 65 anos, 4. Diabetes Mellitus e 5. ASA > 2.
Relacionadas a Doença: 1. Colecistite Aguda, 2. Líquido Pericolecístico, 3. Pós – CPRE, 4. Síndrome de Mirizzi e 5. Edema da parede da vesícula > 5 mm.
Relacionadas a Cirurgia: 1. Hemorragia, 2. Aderências firmes, 3. Anatomia obscura, 4. Fístulas internas e 5. Cirurgia abdominal prévia.
POST-HEPATECTOMY ADVERSE EVENTS
Hepatic resection had an impressive growth over time. It has been widely performed for the treatment of various liver diseases, such as malignant tumors, benign tumors, calculi in the intrahepatic ducts, hydatid disease, and abscesses. Management of hepatic resection is challenging. Despite technical advances and high experience of liver resection of specialized centers, it is still burdened by relatively high rates of postoperative morbidity and mortality. Especially, complex resections are being increasingly performed in high risk and older patient population. Operation on the liver is especially challenging because of its unique anatomic architecture and because of its vital functions. Common post-hepatectomy complications include venous catheter-related infection, pleural effusion, incisional infection, pulmonary atelectasis or infection, ascites, subphrenic infection, urinary tract infection, intraperitoneal hemorrhage, gastrointestinal tract bleeding, biliary tract hemorrhage, coagulation disorders, bile leakage, and liver failure. These problems are closely related to surgical manipulations, anesthesia, preoperative evaluation and preparation, and postoperative observation and management. The safety profile of hepatectomy probably can be improved if the surgeons and medical staff involved have comprehensive knowledge of the expected complications and expertise in their management.
Classroom: Hepatic Resections
The era of hepatic surgery began with a left lateral hepatic lobectomy performed successfully by Langenbuch in Germany in 1887. Since then, hepatectomy has been widely performed for the treatment of various liver diseases, such as malignant tumors, benign tumors, calculi in the intrahepatic ducts, hydatid disease, and abscesses. Operation on the liver is especially challenging because of its unique anatomic architecture and because of its vital functions. Despite technical advances and high experience of liver resection of specialized centers, it is still burdened by relatively high rates of postoperative morbidity (4.09%-47.7%) and mortality (0.24%-9.7%). This review article focuses on the major postoperative issues after hepatic resection and presents the current management.
REVIEW_ARTICLE_HEPATECTOMY_COMPLICATIONS
Review of POSTGASTRECTOMY SYNDROMES

The first postgastrectomy syndrome was noted not long after the first gastrectomy was performed: Billroth reported a case of epigastric pain associated with bilious vomiting as a sequel of gastric surgery in 1885. Several classic treatises exist on the subject; we cannot improve on them and merely provide a few references for the interested reader. Surgical procedures on the stomach, performed for reasons such as peptic ulcer disease, cancer, obesity, or gastroesophageal reflux disease, can result in various post-gastrectomy syndromes. These syndromes include chronic symptoms that range from mild discomfort to life-altering conditions. This guide covers the most common syndromes and their characteristics.
GASTRECTOMY VIDEO SURGERY
Dumping Syndrome
Dumping Syndrome is characterized by gastrointestinal and vasomotor symptoms that occur after food intake due to rapid gastric emptying. This syndrome can occur after surgeries that alter the regulation of gastric emptying or gastric compliance, such as gastrectomy, proximal vagotomy, sleeve gastrectomy, fundoplication, pyloroplasty, and gastrojejunostomy (GJ). Depending on the speed of emptying and the osmolarity of gastric contents, symptoms can vary.
- Early Dumping: Occurs within 30 minutes after food intake and is characterized by palpitations, tachycardia, fatigue, a need to lie down after meals, flushing or pallor, sweating, dizziness, hypotension, headache, and possibly syncope. Abdominal symptoms include early satiety, epigastric fullness, abdominal pain, bloating, hypermotility, and splenic blood pooling.
- Late Dumping: Appears 1 to 3 hours after eating, due to reactive hypoglycemia caused by an initially high glucose load leading to an inappropriately high insulin response. Symptoms include sweating, faintness, difficulty concentrating, and altered levels of consciousness.
Diagnosis is confirmed through an oral glucose tolerance test or a gastric emptying scintigraphy study.
Post-Vagotomy Diarrhea
Post-vagotomy diarrhea is a common complication after vagotomy, characterized by frequent episodes of watery diarrhea. It can be attributed to changes in intestinal motility and bile secretion.
Gastric Stasis
Gastric stasis or delayed gastric emptying can occur due to disruption of normal gastric motility. Symptoms include nausea, vomiting, and a feeling of fullness. Diagnosis is confirmed through gastric emptying studies.
Bile Reflux Gastritis
Bile reflux gastritis is caused by the reflux of bile into the stomach, resulting in epigastric pain and bilious vomiting. Diagnosis can be confirmed through upper endoscopy and gastric pH monitoring.
Afferent and Efferent Loop Syndromes
Afferent loop syndrome occurs after Billroth II reconstruction and is characterized by abdominal pain, bilious vomiting, and distention. Efferent loop syndrome occurs when there is an obstruction of the efferent loop, leading to similar symptoms.
Roux Syndrome
Roux syndrome is a complication of Roux-en-Y procedures, characterized by postprandial abdominal pain and vomiting. Diagnosis is made through a contrast gastrointestinal transit study.
Therapeutic Approach
Management of post-gastrectomy syndromes includes dietary modifications, such as eating small frequent meals, separating liquids and solids, increasing protein and fat intake, and reducing simple sugars. In some cases, additional pharmacological or surgical interventions may be necessary. Understanding these syndromes and their therapeutic approaches is crucial to providing effective care and improving the quality of life for post-gastrectomy patients.
This article focuses on the small proportion of patients with severe, debilitating symptoms; these symptoms can challenge the acumen of the surgeon who is providing the patient’s long-term follow-up and care.
POSTGASTRECTOMY_SYNDROMES_REVIEW_ARTICLE
Laparoscopic Surgery for Morbid Obesity
The morbid obesity epidemic continues to spread throughout industrialized nations. It is a condition with a heterogeneous etiology, including genetic, psychosocial, and environmental factors. Prevention methods have currently been unable to halt the further spread of this disease. Obesity has been linked to increased healthcare costs, common physiologic derangements, reduced quality of life, and increased overall mortality. More than one third of adults and almost 17% of children in the United States are obese.
Medical therapy that can cause sustained significant weight loss may be years away. Bariatric surgery, when combined with a multidisciplinary team, continues to be the only proven method to achieve sustained weight loss in most patients. Bariatric procedures modify gastrointestinal anatomy and, in some cases, enteric hormone release to reduce caloric intake, reduce absorption, and alter metabolism to achieve weight loss. Currently, the three most common bariatric operations in the United States are Roux-en-Y gastric bypass, adjustable gastric band, and the vertical sleeve gastrectomy.
GOSSIPIBOMA
O termo “gossipiboma” refere-se a uma matriz de matéria têxtil envolvida por reacção de corpo estranho. O termo é derivado do latim “Gossypium”, algodão, e o Swahili “boma”, que significa “esconderijo”. Também conhecida como textiloma, originada de “textilis” (tecer em latim) e “oma” (doença, tumor ou inchaço em grego). O primeiro caso foi descrito por Wilson em 1884. Gossipibomas foram relatados após operações em muitos processos, e em diferentes órgãos e localização. Mas, o local mais comum é o abdominal. Gaze e compressas são os materiais mais comumente retidos após laparotomia. A incidência de gossipibomas é variável e subnotificada, principalmente devido às implicações legais de sua detecção, mas também porque muitos pacientes permanecem assintomáticos. A apresentação clínica é também variável. O tratamento recomendado é a excisão que pretende evitar as complicações que conduzem a taxa de mortalidade entre11-35%.
Epidemiologia
Ele ocorre entre 1/1000 a 1/1500 nas operações intra-abdominais. A apresentação clínica é variável e depende da localização do corpo estranho e sobre o tipo de reação inflamatória apresentada pela hospedeiro. Podem existir formas agudas e crônicas. A forma aguda tende a apresentar-se com fístulas e abcessos cutâneos, enquanto que a crônica como massa encapsulada (granuloma de corpo estranho) e sintomas inespecíficos. Gossipibomas ocorrem mais comumente após operação abdominal e pélvica. Eles são mais frequentes em pacientes obesos e quando a operação é realizada em emergência. A incidência é maior em nove vezes após operação de emergência, e de quatro em procedimentos não planejados no decorrer de uma intervenção, mudando o que se pretendia realizar. Outros fatores predisponentes incluem operações em campo de batalha, complicações intra-operatórias, tais como perda intensa de sangue, a incapacidade de realizar contagem de materiais cirúrgicos no final do processo, tempo de operação prolongado e as mudanças no pessoal médico e de enfermagem durante o operação.
Evolução clínica
O tempo entre a operação e aparecimento de manifestações clínicas de Gossipiboma é variável, em particular se o material permanecer estéril. Ele depende da localização do material retido e do tipo de reação orgânica, e foi estimado em entre 10 dias a vários anos. Em patologia, duas reações de corpo estranho pode occorer. A primeira resposta é a produção asséptica de fibrina, o que leva à formação de aderências, material de encapsulamento e à formação de granulomas de corpo estranho. Nesta apresentação, o paciente pode permanecer assintomático por meses ou anos. A segunda resposta é exsudativa, com formação de abcessos, fístulas aos órgãos internos como o estômago, intestino, bexiga, cólon ou vagina, ou também fístula externa para a parede abdominal. Os sintomas dependem do órgão afetado principalmente e podem resultar da compressão, obstrução, síndrome de má absorção, ou crescimento bacteriano. Eles incluem dor abdominal, tumor palpável, náuseas, vômitos, sangramento retal, diarréia, disúria, piúria, hematúria e urgência urinária. Os sintomas sistêmicos como febre, anorexia, anemia e perda de peso também podem occurer. No entanto, a resposta inflamatória e aderências podem formar uma cápsula com o bloqueio omental e órgãos adjacentes, podendo o paciente permanecer assintomático. A falta de sintomas pode dificultar ou retardar o diagnóstico, que muitas vezes é realizado incidentalmente.
Possibilidades diagnósticas
O diagnóstico pode ser difícil. Suspeita clínica e o uso de estudos de imagem são importantes, pois é a regra a inexistência ou inespecificidade de sintomas em vários anos após a operação. No pré-operatório pode ser levantada suspeita por meio de estudos radiológicos ou endoscópicos. Muitos casos só são descobertos no intra-operatório. Tomografia computadorizada é o exame complementar de escolha para o diagnóstico e avaliação dessas complicações. Ele fornece informações detalhadas sobre a lesão na maioria dos casos. A aparência pode ser lesão cística espongiforme, cápsula hiperdensa em camadas concêntricas, ou calcificações murais. A presença de gás é indicativa de perfuração do intestino ou à formação de abcessos. Os principais diagnósticos diferenciais são: aderências pós-operatórias, fecalomas, contusões, hematomas, intussuscepção, volvo, tumores e abscessos intracavitários.
Tratamento e Prognóstico
O tratamento de escolha é a remoção cirúrgica que pode ser realizada por laparoscopia ou laparotomia, e visa prevenir complicações. O prognóstico da gossipiboma é variável com taxas de mortalidade de 11 para 35%. Quando a remoção ocorre no período pós-operatório imediato, a morbidade e mortalidade são baixas; no entanto, se o material foi mantido por um longo tempo a remoção pode exigir operação extensa e ter elevado índice de complicações.
Implicações médico-legais
Há muitas implicações médico-legais com gossypiboma. Revisão de negligência médica impetradas entre 1988 e 1994 revelou 40 casos de gossipiboma, que representaram 48% de todos os corpos estranhos. Não foi possível determinar se o material esquecimento representou falta de qualidade do cirurgião ou quadro de enfermagem.
Procedimentos preventivos
A abordagem mais importante é a prevenção. As medidas preventivas necessárias incluem o uso de material têxtil com marcadores radiopacos e contagem minuciosa de materiais cirúrgicos. São recomendadas quatro contagens: na montagem do material, antes da operação, no início do fechamento da cavidade e durante a síntese da pele. Dhillon e Park reforçam a importância da exploração dos quatro quadrantes abdominais no final da operação em todos os casos, mesmo após a contagem das compressas. No caso de contagem incorreta, a menos que o paciente seja considerado instável, a síntese da cavidade não deve ser realizada até que todas elas estejam localizados.
CONCLUSÃO
Gossipiboma é um problema médico-legal sério e sua incidência está aparentemente aumentando. Por isso, os meios e métodos nos procedimentos cirúrgicos durante o ato operatório e no contexto geral da sala de operações precisam ser revistos para tomarem-se medidas preventivas. Formação continuada de profissionais da área médica e estrita adesão à técnica operatória são primordiais para a prevenção de gossipiboma.
Ebook: Princípios da Cirurgia Hepatobiliar

Cirurgia Hepatobiliar
Considera-se que a cirurgia hepática começou após o advento da anestesia e da anti-sepsia. No entanto, muito antes disso, diversos autores já relatavam suas experiências com ressecções do fígado. As primeiras descrições de “cirurgias hepáticas” consistiam no relato de avulsões parciais ou totais de porções do fígado após lesões traumáticas do abdome. O relato de Elliot (1897) exemplifica muito dos temores dos cirurgiões da época: “O fígado (…) é tão friável, tão cheio de vasos e tão evidentemente impossível de ser suturado que parece ser improvável o manejo bem sucedido de grandes lesões de seu parênquima”.
CIRURGIA HEPATOBILIAR_ASPECTOS BÁSICOS
Lymph Node Dissection in Gastric Adenocarcinoma
Extent of lymph node dissection has been an area of controversy in gastric adenocarcinoma for many years. Some surgeons believe that cancer metastasizes through a stepwise progression, and an extensive lymphadenectomy is necessary to improve survival and/or cure the patient. Other physicians argue that extensive ly-mphadenectomies only add pe-rioperative morbidity and mor-tality and do not improve survival. Asian countries have been performing extended lymphadenectomies routinely for many years with promising survival data, although Western countries have not been able to reproduce those results. Much of the controversy surrounding lymphadenectomies started in the 1980s when Japanese studies reported superior survival rates matched stage for stage, compared to the United States. This was theorized to be secondary to the more extensive lymphadenectomy performed in Japan compared to the United States.

A United Kingdom study randomized 400 patients to either a D1 or a D2 lymph node dissection. Those patients with tumors in the upper or middle third of the stomach underwent a distal pancreaticosplenectomy to obtain retropancreatic and splenic hilar nodes. While the 5-year survival rates were not statistically significant between the two groups, on multivariate analyses it was noted that those patients in the D2 group that did not undergo the distal pancreaticosplenectomy had an increased survival compared with the D1 group. A trial in the Netherlands randomized 380 gastric cancer patients to a D1 lymphadenectomy and 331 patients to a D2 lymphadenectomy. Similar to the United Kingdom study, there was not a significant difference in survival between the two groups, even when followed out to 11 years. There was a significant increase in postoperative complications in the D2 group compared with the D1 group (43 % vs. 25 %, respectively) as well as mortality (10 % vs. 4 %, respectively).
The data from these two studies suggest that a pancreaticosplenectomy performed to harvest lymph nodes seems to only add morbidity and mortality while not improving survival. One concern raised about the prior two studies was the variation in surgical technique and lack of standardization of surgeon experience. A Taiwanese study accounted for this by performing the study at a single institution with three surgeons, each of whom had completed at least 25 D3 lymph node dissections prior to the study. Patients with gastric cancer were randomized to a D1 lymph node dissection (defined as resection of perigastric lymph nodes along the lesser and greater curves of the stomach) or a D3 lymph node dissection (defined as resection of additional lymph nodes surrounding the splenic, common hepatic, left gastric arteries, nodes in the hepatoduodenal ligament, and retropancreatic lymph nodes). There was an overall 5-year survival benefit with the D3 group of 60 % compared with the D1 group of 54 %. A Japanese study evaluated a more aggressive lymph node dissection and randomized patients to a D2 dissection or a para-aortic lymph node dissection (PAND). There was no significant difference in 5-year survival between the two groups with a trend toward an increase in complications in the PAND group. Multiple studies have shown that the number of positive lymph nodes is a significant predictor of survival. Current AJCC guidelines stipulate that at least 15 lymph nodes are needed for pathologic examination to obtain adequate staging.
Laparoscopic techniques have become an integral part of surgical practice over the past several decades. For gastric cancer, multiple retrospective studies have reported the advantages of laparoscopic gastrectomy (LG) over open gastrectomy (OG). A recent meta-analysis of 15 nonrandomized comparative studies has also shown that although LG had a longer operative time than OG, it was associated with lower intraoperative blood loss, overall complication rate, fewer wound-related complications, quicker recovery of gastrointestinal motility with shorter time to first flatus and oral intake, and shorter hospital stay. A randomized prospective trial comparing laparoscopic assisted with open subtotal gastrectomy reported that LG had a significantly lower blood loss (229 ± 144 ml versus 391 ± 136 ml; P< 0.001), shorter time to resumption of oral intake (5.1 ± 0.5 days versus 7.4 ± 2 days; P< 0.001), and earlier discharge from hospital (10.3 ± 3.6 days versus 14.5 ± 4.6 days; P< 0.001).
Como funciona o GRAMPEADOR INTESTINAL ?
A Busca pela Segurança e Eficiência na Cirurgia Moderna
Introdução O objetivo primordial de qualquer cirurgião, ao iniciar uma intervenção, é garantir que o procedimento seja seguro e eficiente. A “regra de ouro” da cirurgia moderna permanece clara: o ato operatório deve ser o mais breve possível, gerando o menor trauma tecidual e restaurando a função do órgão. O resultado esperado é sempre a minimização das intercorrências no pós-operatório. Embora a cirurgia atual atinja esses objetivos de forma bastante satisfatória, as complicações relacionadas às suturas e à cicatrização ainda são desafios presentes na rotina hospitalar.
A Evolução Histórica e os Desafios da Cicatrização A confiabilidade das suturas gastrointestinais, por exemplo, é uma conquista relativamente recente. Foi apenas no final do século XIX que a compreensão dos princípios básicos da cicatrização tecidual permitiu avanços significativos nesta área. Sabemos hoje que o sucesso do reparo tecidual não depende apenas da técnica empregada, mas é uma equação complexa que envolve o paciente e a área operada. Diversos fatores podem retardar ou prejudicar drasticamente a cicatrização, entre eles:
-
Isquemia (falta de suprimento sanguíneo);
-
Edema (inchaço excessivo);
-
Infecção local ou sistêmica;
-
Desnutrição do paciente.
O Fator Humano e o Surgimento da Tecnologia Existe uma variável crítica na cirurgia: a habilidade manual. Naturalmente, há uma variação na destreza e na técnica entre diferentes cirurgiões. Foi justamente essa disparidade que motivou o desenvolvimento de novos dispositivos cirúrgicos. O objetivo da inovação tecnológica na cirurgia é superar as diferenças individuais, funcionando como um equalizador. Ao utilizar dispositivos que padronizam etapas críticas (como as suturas mecânicas), permite-se que técnicas complexas sejam executadas adequadamente, independente de quem opera.
Conclusão Para que a medicina avance, uma técnica não pode depender apenas do talento de poucos. Ela deve ser reproduzível de forma confiável pelo maior número possível de cirurgiões. Somente através dessa padronização e do auxílio tecnológico é que os resultados cirúrgicos podem ser amplamente adotados, reconhecidos como eficazes e, acima de tudo, seguros para o paciente.
Laparoscopic Colorectal Surgery
With the introduction of laparoscopic colectomy nearly 20 years ago, a relatively slow adoption of laparoscopic colorectal surgery into surgical practice has taken place. It is estimated that 10% to 25% of all colorectal resections are performed utilizing laparoscopy. The persistent steep learning curve, the lack of high-volume colorectal surgery by general surgeons (who perform the bulk of colonic resection in the United States), and the modest advantages reported are but a few of the reasons that the percentage of laparoscopic colorectal procedures has not dramatically risen. With the publication of several large, prospective randomized trials for colon cancer, along with the interest in single-port surgery and natural orifice surgery, there appears to be a renewed interest in minimally invasive procedures for the colon and rectum. This chapter will provide an overview of these issues and offer a current assessment of the common diseases to which minimally invasive techniques have been applied.
Learning Curve
Numerous previous studies have evaluated the learning curve involved in laparoscopic colectomy. It is estimated by conventional laparoscopic techniques that the learning curve for laparoscopic colectomy is at least 20 cases but more likely 50 cases. The need to work in multiple quadrants of the abdomen, the need for a skilled laparoscopic assistant, and the lack of yearly volume has kept the learning curve relatively steep. The surgeon may also need to work in reverse angles to the camera. All of these combined add to the complexity of the procedure and result in the need to perform a number of cases before the surgeon and surgical team become proficient. More recent publications have suggested the learning curve is more than 20 cases. In a prospective randomized study of colorectal cancer in the United Kingdom, the CLASICC trial, surgeons had to perform at least 20 laparoscopic resections before they were allowed to enter the study. The study began in July 1996 and was completed in July 2002. Despite the surgeons’ prior experience, the rate of conversion dropped from 38% to 16% over the course of the study, suggesting that a minimum of 20 cases may not be enough to overcome the learning curve. In the COLOR trial from Europe, another prospective randomized study for colon cancer that required a prerequisite experience in laparoscopic colon resection before surgeons could enter patients in the study, surgeon and hospital volume were directly related to a number of operative and postoperative outcomes. The median operative time for high-volume hospitals (>10 cases/year) was 188 minutes, compared to 241 minutes for low-volume hospitals (<5 cases/year); likewise, conversion rates were 9% versus 24% for the two groups. High-volume groups also had more lymph nodes in the resected specimens, fewer complications, and shortened hospital stays. These two relatively recent multicenter studies suggest that the learning curve is clearly greater than 20 cases and that surgeons need to perform a minimum yearly number of procedures to maintain their skills.
Outcomes
There may not be another area in recent surgical history that has been more heavily scrutinized than laparoscopic colorectal surgery. The plethora of accumulated data allows a careful assessment of all outcome measures for nearly every colorectal disease and procedure. In comparison to conventional colorectal surgery, the benefits of laparoscopy for colorectal procedures compared to open techniques include a reduction in postoperative ileus, postoperative pain, and a concomitant reduction in the need for analgesics; an earlier tolerance of diet; a shortened hospital stay; a quicker resumption of normal activities; improved cosmesis; and possibly preservation of immune function. This is offset by a prolongation in operative time, the cost of laparoscopic equipment, and the learning curve for these technically challenging procedures. When reporting the outcomes of laparoscopic colectomy, a natural selection bias applies when comparing conventional and laparoscopic cases. The most complex cases are generally not suitable for a laparoscopic approach and therefore are performed via an open approach. Also, in many series the results of the successfully completed laparoscopic cases are compared to conventional cases, and the cases converted from a laparoscopic to a conventional procedure may be analyzed separately. Few studies, with the exception of the larger prospective randomized studies, leave the converted cases in the laparoscopic group as part of the “intention to treat” laparoscopic group. This clearly introduces selection bias.
Although the results of prospective randomized trials are available for almost every disease process requiring colorectal resection, the majority of studies of laparoscopic colectomy are retrospective case-control series or noncomparative reports. The conclusions regarding patient outcomes must therefore come from the repetitiveness of the results rather than the superiority of the study design. For any one study, the evidence may be weak; but collectively, because of the reproducibility of results by a large number of institutions, even with different operative techniques and postoperative management parameters, the preponderance of evidence favors a minimally invasive approach with respect to postoperative outcomes.
Operative Time
Nearly all the comparative studies provide information regarding operative times. The definition of the operative time may vary with each series, and there may be different groups of surgeons performing the laparoscopic and conventional procedures. With the exception of a few reports, nearly all studies demonstrated a prolonged operative time associated with laparoscopic procedures. In prospective randomized trials, the procedure was roughly 40 to 60 minutes longer in the laparoscopic groups. As the surgeon and team gain experience with laparoscopic colectomy, the operating times do reliably fall, but rarely do they return to the comparable time for a conventional approach.
Return of Bowel Activity and Resumption of Diet
Reduction in postoperative ileus is one of the proposed major advantages of minimally invasive surgery. Nearly all of the retrospective and prospective studies comparing open and laparoscopic colectomy have shown a statistically significant reduction in the time to passage of flatus and stool. Most series demonstrate a 1- to 2-day advantage for the laparoscopic group. Whether the reduction of ileus relates to less bowel manipulation or less intestinal exposure to air during minimally invasive surgery remains unknown. With the reduction in postoperative ileus, the tolerance by the patient of both liquids and solid foods is quicker following laparoscopic resection. The time to resumption of diet varies from 2 days to 7 days, but in the majority of comparative studies, this is still 1 to 2 days sooner than in patients undergoing conventional surgery. Again, the physician and patient were not blinded in nearly all studies, which may have altered patient expectations. However, the overwhelming reproducible data reported in both retrospective and prospective studies of laparoscopic procedures does likely favor a reduction of postoperative ileus and tolerance of liquid and solid diets.
Postoperative Pain
To measure postoperative pain, a variety of assessments have been performed to demonstrate a significant reduction in pain following minimally invasive surgery; some studies utilize an analog pain scale, and others measure narcotic requirements. Physician bias and psychologic conditioning of patients may interfere with the evaluation of postoperative pain. There are also cultural variations in the response to pain. Three of the early prospective randomized trials have evaluated pain postoperatively, and all three have found a reduction in narcotic requirements in patients undergoing laparoscopic colectomy. In the COST study, the need both for intravenous and oral analgesics was less in patients undergoing successfully completed laparoscopic resections. Numerous other nonrandomized studies have shown a reduction in postoperative pain and narcotic usage.
Length of Stay
The quicker resolution of ileus, earlier resumption of diet, and reduced postoperative pain has resulted in a shortened length of stay for patients after laparoscopic resection when compared to traditional procedures. Recovery after conventional surgery has also been shortened, but in the absence of minimally invasive techniques, it would seem unlikely that the length of stay could be further reduced. In nearly all comparative studies, the length of hospitalization was 1 to 6 days less for the laparoscopic group. Although psychological conditioning of the patient cannot be helped and likely has a desirable effect, the benefits of minimally invasive procedures on the overall length of stay cannot be discounted. The benefit, however, is more likely a 1 to 2 day advantage only. The more recent introduction of clinical pathways, both in conventional and laparoscopic surgery, has also narrowed the gap but appears to be more reliable in patients undergoing a minimally invasive approach.
Hospital Costs
One of the disadvantages of laparoscopy is the higher cost related to longer operative times and increased expenditures in disposable equipment. Whether the total cost of the hospitalization (operative and hospital costs) is higher following laparoscopic colectomy is debatable. A case-control study from the Mayo Clinic looked at total costs following laparoscopic and open ileocolic resection for Crohn’s disease (CD). In this study, 66 patients underwent laparoscopic or conventional ileocolic resection and were well matched. Patients in the laparoscopic group had less postoperative pain, tolerated a regular diet 1 to 2 days sooner, and had a shorter length of stay (4 vs. 7 days). In the cost analysis, despite higher operative costs, the overall mean cost was $3273 less in the laparoscopic group. The procedures were performed by different groups of surgeons at the institution, and although the surgeons may have introduced biases, this study was undertaken during the current era of cost containment, in which all physicians are encouraged to reduce hospital stays. The results are similar for elective sigmoid diverticular resection with a mean cost savings of $700 to $800. Clearly, if operative times and equipment expenditure are minimized, the overall cost of a laparoscopic resection should not exceed a conventional approach.
Tratamento Laparoscópica da DIVERTICULITE AGUDA
O aumento da prevalência de doença diverticular fez o seu adequado manuseio mais um assunto de debate constante. Especialmente para os casos de diverticulite, progresso considerável tem sido feito em termos de diagnóstico e tratamento. Diagnóstico apropriado em TC e técnicas intervencionistas são agora amplamente disponíveis, bem como agentes antimicrobianos eficazes. Finalmente, como a ressecção cirúrgica do cólon envolvido é a única maneira de erradicar definitivamente essa condição, a colectomia eletiva laparoscópica surgiu como uma opção segura e interessante entre as opções de tratamento. Embora tenha sido recentemente contestada sobre a sua progressão, a história natural da diverticulite é assumida como sendo a de recorrência ao longo do tempo, pelo menos, em um terço dos pacientes. O medo das complicações desta doença benigna e prevalente tem motivado sociedades médicas e cirúrgicas para produzir orientações e consensos sobre o assunto. A mortalidade geralmente vem de sepse recorrente e/ou operações de emergência para casos mais complicados. Como resultado, o procedimento cirúrgico mais realizado, a sigmoidectomia eletiva, é normalmente indicada para todos os casos complicados e muitos dos não-complicados. A abordagem laparoscópica para a colectomia esquerda tem evoluído e condições seguras são oferecidas aos pacientes, quando realizado por cirurgiões experientes em laparoscopia.
Retromuscular Prefascial Mesh Hernia Repair (Jean RIVES – René STOPPA)
An incisional hernia is usually defined as a chronic postoperative defect of the abdominal wall through which intra-abdominal viscera protrude. Progress in surgical techniques, even with laparoscopic surgery, has not led to the elimination of incisional hernias. On the contrary, the incidence of this complication seems to be increasing as more major and lengthy operations are being performed, especially in elderly patients with concomitant organic disease. The incidence of this condition has been reported to be as high as 11% of all laparotomies. Surgical repair is difficult in the patient with a large abdominal wall defect, especially if the herniated viscera has “lost its right of domain” in the abdominal cavity. It must be remembered that surgical repair of an incisional hernia is not the same thing as closure of a laparotomy. Weakening of the abdominal wall and the consequences of decreased abdominal pressure on diaphragmatic mobility and respiratory function must also be considered. Placement of a prosthetic mesh is essential because without mesh, the recurrence rate is prohibitive, varying from 30% to 60%. The which is the subject of this article, was popularized by Jean Rives and has been used in our department since 1966.
RIVES_STOPPA_HERNIA_REPAIR
BILIARY-ENTERIC ANASTOMOSIS
 The operative conduct of the biliary-enteric anastomosis centers around three technical steps: 1) identification of healthy bile duct mucosa proximal to the site of obstruction; 2) preparation of a segment of alimentary tract, most often a Roux-en-Y jejunal limb; and 3) construction of a direct mucosa-to-mucosa anastomosis between these two. Selection of the proper anastomosis is dictated by the indication for biliary decompression and the anatomic location of the biliary obstruction. A right subcostal incision with or without an upper midline extension or left subcostal extension provides adequate exposure for construction of the biliary-enteric anastomosis. Use of retractors capable of upward elevation and cephalad retraction of the costal edges are quite valuable for optimizing visual exposure of the relevant hilar anatomy.
The operative conduct of the biliary-enteric anastomosis centers around three technical steps: 1) identification of healthy bile duct mucosa proximal to the site of obstruction; 2) preparation of a segment of alimentary tract, most often a Roux-en-Y jejunal limb; and 3) construction of a direct mucosa-to-mucosa anastomosis between these two. Selection of the proper anastomosis is dictated by the indication for biliary decompression and the anatomic location of the biliary obstruction. A right subcostal incision with or without an upper midline extension or left subcostal extension provides adequate exposure for construction of the biliary-enteric anastomosis. Use of retractors capable of upward elevation and cephalad retraction of the costal edges are quite valuable for optimizing visual exposure of the relevant hilar anatomy.

Division of the ligamentum teres and mobilization of the falciform ligament off the anterior surface of the liver also facilitate operative exposure; anterocephalad retraction of the ligamentum teres and division of the bridge of tissue overlying the umbilical fissure are critical for optimal visualization of the vascular inflow and biliary drainage of segments II, III, and IV. Cholecystectomy also exposes the cystic plate, which runs in continuity with the hilar plate. Lowering of the hilar plate permits exposure of the left hepatic duct as it courses along the base of segment IVb. In cases of unilateral hepatic atrophy as a result of long-standing biliary obstruction or preoperative portal vein embolization, it is critical to understand that the normal anatomic relationships of the portal structures are altered. In the more common circumstance of right-sided atrophy, the portal and hilar structures are rotated posteriorly and to the right; as a result, the portal vein, which is typically most posterior, is often encountered first; meticulous dissection is necessary to identify the common bile duct and hepatic duct deep within the porta hepatis.
BILIARY-ENTERIC ANASTOMOSIS_THECNICAL ASPECTS
Lesão de Vias Biliares na Colecistectomia: Prevenção e Tratamento
A via laparoscópica tem sido reconhecida como padrão de excelência para a colecistectomias. Phillipe Mouret foi quem primeiro a realizou em 1987, mas outros procedimentos já haviam sido realizados por laparoscopia e foram descritos por ginecologistas. Desenvolvida no final da década de 80 e início dos anos 90, a videolaparoscopia mudou os conceitos de acesso cirúrgico e campo operatório, introduzindo a concepção de “cirurgia minimamente invasiva”.A colecistectomia é um dos procedimentos cirúrgicos mais realizados no mundo. Com o advento da videolaparoscopia, tornou-se uma cirurgia menos traumática, mais estética, com períodos mais curtos de internação. Em contrapartida, observou-se o aumento da incidência de lesões de via biliar extra-hepática quando comparado ao procedimento aberto, fato preocupante devido à morbidade elevada desse tipo de lesão, cuja mortalidade não é desprezível.