Prevention of Bile Duct Injury
Prevention of Bile Duct Injury During Laparoscopic Cholecystectomy
Introduction
Bile duct injury (BDI) during laparoscopic cholecystectomy is a significant surgical complication with profound clinical and medico-legal implications. The incidence of BDI ranges from 0.3% to 0.6%, despite advances in surgical techniques and imaging modalities. The prevalence of BDI remains concerning due to its association with high morbidity and mortality rates. Patients who suffer from BDI often face prolonged hospital stays, multiple surgeries, and long-term complications such as bile leakage, strictures, and secondary biliary cirrhosis. Medico-legally, BDI is one of the most common reasons for litigation against surgeons, often resulting in significant financial settlements and professional repercussions.
Questions and Answers
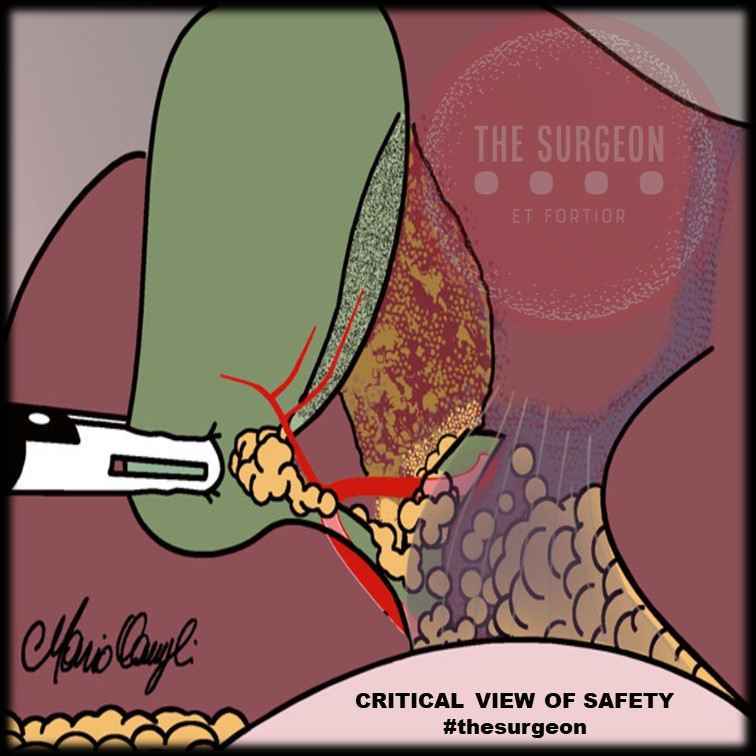
Question 1: What technique should be used to identify the anatomy during laparoscopic cholecystectomy?
Answer: The Critical View of Safety (CVS) is recommended for identifying the cystic duct and cystic artery.
Key Findings: The incidence of BDI was found to be 2 in one million cases using CVS, compared to 1.5 per 1000 cases with the infundibular technique.
Question 2: When should intraoperative cholangiography (IOC) be used?
Answer: IOC should be used in cases of anatomical uncertainty or suspicion of bile duct injury.
Key Findings: IOC aids in the prevention and immediate management of BDI by providing a precise assessment of biliary anatomy during surgery.
Question 3: What are the recommendations for managing patients with confirmed or suspected bile duct injury?
Answer: Patients with confirmed or suspected BDI should be referred to an experienced surgeon or a multidisciplinary hepatobiliary team.
Key Findings: Early referral to hepatobiliary specialists is associated with better long-term outcomes and lower complication rates.
Question 4: Should the “fundus-first” technique be used when CVS cannot be achieved?
Answer: Yes, the “fundus-first” technique is recommended when CVS cannot be achieved.
Key Findings: This technique is effective for safely dissecting the gallbladder in complex cases where anatomy is unclear.
Question 5: Should CVS be documented during laparoscopic cholecystectomy?
Answer: Yes, documenting CVS with double-static photographs is recommended.
Key Findings: Photographic documentation of CVS ensures correct anatomical identification and serves as a record for later review in case of complications.
Question 6: Should near-infrared biliary imaging be used intraoperatively?
Answer: The evidence for near-infrared biliary imaging is limited; thus, IOC is preferred.
Key Findings: IOC is more widely studied and proven effective in preventing BDI compared to near-infrared imaging.
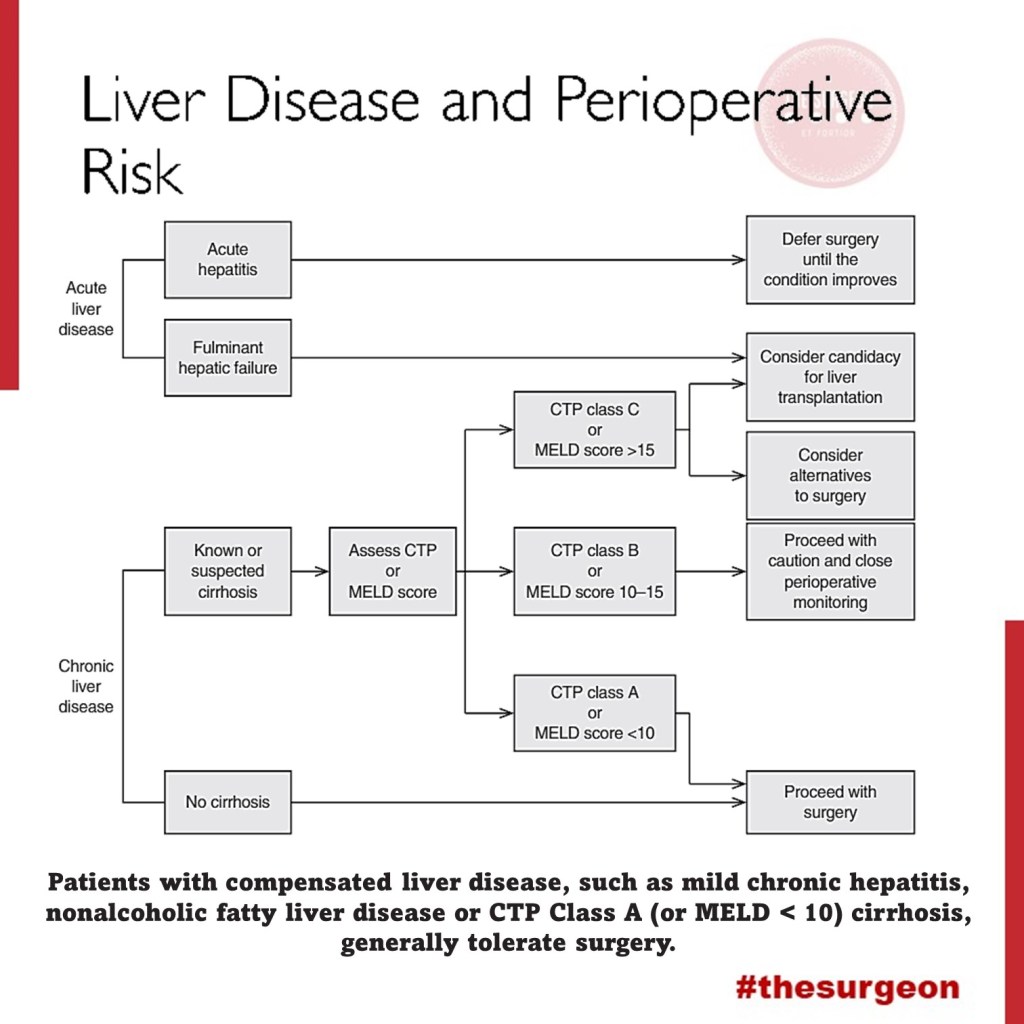
Question 7: Should surgical risk stratification be used to mitigate the risk of BDI?
Answer: Yes, surgical risk stratification is recommended.
Key Findings: Risk stratification helps identify patients at higher risk of complications, aiding in surgical planning and decision-making.
Question 8: Should the presence of cholecystolithiasis be considered in risk stratification?
Answer: Yes, the presence of cholecystolithiasis should be considered in risk stratification.
Key Findings: Patients with cholecystolithiasis have a higher risk of complications during cholecystectomy, making it important to include this condition in risk assessments.
Question 9: Should immediate cholecystectomy be performed in cases of acute cholecystitis?
Answer: Yes, immediate cholecystectomy within 72 hours is recommended.
Key Findings: Surgery within 72 hours of the onset of acute cholecystitis symptoms is associated with lower complication rates and better patient recovery.
Question 10: Should subtotal cholecystectomy be performed in cases of severe inflammation?
Answer: Yes, subtotal cholecystectomy is recommended in cases of severe inflammation where CVS cannot be obtained.
Key Findings: In severe inflammation scenarios, subtotal cholecystectomy can facilitate the surgery and reduce the risk of BDI.
Question 11: Which approach is preferable, four-port laparoscopic cholecystectomy or reduced-port/single-incision?
Answer: Four-port laparoscopic cholecystectomy is recommended as the standard approach.
Key Findings: The four-port technique is the most studied, showing effectiveness and safety in performing cholecystectomies with lower complication risks.
Question 12: Should interval cholecystectomy be performed following percutaneous cholecystostomy?
Answer: Yes, interval cholecystectomy is recommended after initial stabilization with percutaneous cholecystostomy.
Key Findings: Interval cholecystectomy offers better long-term outcomes and lower risk of recurrent complications compared to no additional treatment.
Question 13: Should laparoscopic cholecystectomy be converted to open in difficult cases?
Answer: Yes, conversion to open surgery is recommended in cases of significant difficulty.
Key Findings: Conversion to open surgery can prevent BDI in situations where laparoscopic dissection is extremely difficult or risky.
Question 14: Should a waiting time be implemented to verify CVS?
Answer: Yes, a waiting time to verify CVS is recommended.
Key Findings: A waiting time allows better anatomical evaluation before proceeding with dissection, reducing the risk of BDI.
Question 15: Should two surgeons be used in complex cases?
Answer: The presence of two surgeons can be beneficial in complex cases, although strong recommendations are not made due to limited evidence.
Key Findings: Some studies suggest that collaboration between two surgeons can improve anatomical identification and reduce complications in difficult cases.
Question 16: Should surgeons receive coaching on CVS to limit the risk or severity of BDI?
Answer: Yes, surgeons should receive coaching on CVS.
Key Findings: Surgeons who receive targeted coaching on CVS show improved anatomical identification and reduced rates of BDI.
Question 17: Should simulation or video-based education be used to train surgeons?
Answer: Yes, simulation or video-based education should be used.
Key Findings: These training methods enhance technical skills, increase surgical precision, and reduce the incidence of BDI during laparoscopic cholecystectomy.
Conclusion
The consensus recommendations provide evidence-based approaches to minimize bile duct injury during laparoscopic cholecystectomy. Practices such as the critical view of safety (CVS), intraoperative cholangiography (IOC), and early referral to specialists can significantly improve surgical outcomes and reduce complications. As famously stated, “The history of surgery is the history of the control of bleeding,” a phrase that underscores the importance of meticulous surgical technique and the prevention of complications like bile duct injuries.
Liderança no Campo da Cirurgia
O campo da cirurgia está em constante evolução, exigindo não apenas habilidades técnicas de alta qualidade, mas também capacidades de liderança excepcionais. No entanto, a formação tradicional dos cirurgiões raramente inclui treinamento formal em liderança, deixando muitos profissionais despreparados para assumir posições de liderança. Este artigo explora a importância da liderança na cirurgia, os diferentes tipos de liderança, suas características e oferece recomendações para o desenvolvimento de líderes cirúrgicos.
A Importância da Liderança na Cirurgia
Historicamente, os cirurgiões eram vistos como líderes incontestáveis dentro de um modelo de treinamento de aprendizado, onde a experiência pessoal e o julgamento clínico guiavam as práticas. No entanto, a modernização da medicina, impulsionada pela tecnologia e pela disponibilidade de dados, transformou o ambiente cirúrgico em um campo mais colaborativo e complexo. A liderança eficaz agora é crucial para navegar esse ambiente volátil, incerto, complexo e ambíguo. Como disse Napoleão Bonaparte, “Um líder é um negociador de esperanças.” Na cirurgia, liderar é guiar equipes em meio a incertezas, mantendo sempre a esperança e a confiança nos melhores resultados para os pacientes.
Desenvolvimento da Liderança Cirúrgica
Apesar da importância, muitos cirurgiões recém-formados não recebem treinamento formal em liderança durante a residência. Ao contrário de outras profissões, onde a liderança é um componente central da formação, os médicos devem aprender habilidades de liderança na prática ou através da observação de líderes bem-sucedidos. Programas de desenvolvimento de liderança, semelhantes aos oferecidos a oficiais militares e executivos de negócios, poderiam beneficiar grandemente os cirurgiões. George S. Patton afirmou: “Não diga às pessoas como fazer as coisas, diga-lhes o que fazer e deixe que elas surpreendam você com seus resultados.” Essa filosofia pode ser aplicada na cirurgia, incentivando a autonomia e a inovação dentro das equipes cirúrgicas.
Tipos de Liderança em Cirurgia
Diversos estilos de liderança podem ser aplicados no campo da cirurgia, cada um com suas características únicas:
- Liderança Autoritária:
- Caracterizada por decisões centralizadas e controle rígido.
- Pode ser eficaz em situações de emergência onde decisões rápidas são necessárias.
“O verdadeiro gênio reside na capacidade de avaliar informações incertas, conflitantes, e perigosas.” Winston Churchill
- Liderança Hierárquica:
- Baseada em uma estrutura de comando clara.
- Útil em ambientes estruturados com protocolos bem definidos.
Sun Tzu, em “A Arte da Guerra”, escreveu: “Aquele que é prudente e espera por um inimigo imprudente será vitorioso.”
2. Liderança Transacional:
- Focada em recompensas e punições para alcançar resultados.
- Pode ser útil para manter a eficiência e a produtividade.
Douglas MacArthur disse: “Os soldados devem ter ganho pessoal de suas ações; isso estimula o cumprimento do dever.”
3. Liderança Transformacional:
- Inspira e motiva a equipe a alcançar metas além das expectativas.
- Promove inovação e mudanças positivas na prática cirúrgica.
“O maior líder não é necessariamente aquele que faz as maiores coisas. Ele é aquele que faz as pessoas fazerem as maiores coisas.” – Ronald Reagan
4. Liderança Adaptativa:
- Envolve a capacidade de ajustar-se a novas situações e desafios.
- Crucial em ambientes cirúrgicos dinâmicos e em constante mudança.
Dwight D. Eisenhower afirmou: “Os planos são inúteis, mas o planejamento é tudo.”
5. Liderança Situacional:
- Adapta o estilo de liderança com base nas necessidades específicas da equipe e da situação.
- Proporciona flexibilidade e resposta eficaz a diferentes cenários clínicos.
Como observou Alexander, o Grande: “Não há nada impossível para aquele que tentará.”
6. Liderança Servidora:
- Foca no bem-estar e no desenvolvimento dos membros da equipe.
- Constrói uma cultura de apoio e colaboração.
“O melhor dos líderes é aquele cujo trabalho é feito, cujas pessoas dizem: ‘Nós fizemos isso sozinhos.'” – Lao-Tzu
Características de um Líder Cirúrgico Eficaz
Um líder cirúrgico eficaz deve possuir várias qualidades essenciais, incluindo visão, flexibilidade, motivação, inteligência emocional (EI), empatia, adaptabilidade, confiança, confiabilidade, responsabilidade e habilidades de gestão. A visão permite ao líder definir e perseguir objetivos claros, enquanto a flexibilidade e a adaptabilidade são necessárias para navegar em um ambiente em rápida mudança. Napoleão Bonaparte afirmou: “A liderança é uma combinação de estratégia e caráter. Se você precisar dispensar um, dispense a estratégia.” Essa citação reflete a importância do caráter e da integridade na liderança cirúrgica. A inteligência emocional e a empatia são fundamentais para a comunicação eficaz e para a construção de relacionamentos sólidos dentro da equipe. A confiabilidade e a responsabilidade asseguram que o líder seja um exemplo a ser seguido, promovendo uma cultura de confiança e responsabilidade mútua.
Recomendações para o Desenvolvimento de Líderes Cirúrgicos
Para desenvolver habilidades de liderança, os cirurgiões devem buscar oportunidades de treinamento formal em liderança, participar de workshops e seminários, e buscar orientação de mentores experientes. A autoavaliação honesta e o feedback contínuo são essenciais para o crescimento pessoal e profissional. Além disso, a incorporação de programas de liderança nos currículos de residência cirúrgica pode preparar melhor os futuros cirurgiões para os desafios do campo. Estabelecer um ambiente que encoraje a liderança colaborativa e o desenvolvimento contínuo também é crucial para a formação de líderes eficazes.
Conclusão
A liderança no campo da cirurgia é essencial para enfrentar os desafios de um ambiente médico moderno e complexo. Desenvolver habilidades de liderança em cirurgiões pode melhorar significativamente os resultados dos pacientes e promover uma prática cirúrgica mais eficiente e colaborativa. Ao reconhecer a importância da liderança e investir em seu desenvolvimento, a comunidade cirúrgica pode assegurar um futuro mais brilhante e inovador para a medicina.
Fricção Cirúrgica: Desafios e Realidades no Centro Cirúrgico
Fricção Cirúrgica: Desafios e Realidades no Centro Cirúrgico
No universo da teoria militar, Carl von Clausewitz introduziu o conceito de “fricção” para descrever as dificuldades e imprevistos que complicam a execução dos planos de guerra. Esse conceito, no entanto, transcende o campo de batalha e encontra paralelos surpreendentes em outros cenários complexos e de alta pressão, como o centro cirúrgico. A “fricção cirúrgica” refere-se às diversas dificuldades que cirurgiões e equipes médicas enfrentam durante procedimentos, afetando a eficiência e os resultados esperados.
Imprevisibilidade e Complexidade
Assim como na guerra, a cirurgia está repleta de elementos imprevisíveis. Mesmo com um planejamento meticuloso e uma equipe altamente treinada, fatores inesperados podem surgir. Complicações anatômicas, reações adversas a medicamentos e condições pré-existentes do paciente são apenas alguns exemplos de imprevistos que podem alterar drasticamente o curso de uma operação.
“Tudo na guerra é simples, mas a coisa mais simples é difícil.” – Carl von Clausewitz
Equipamentos e Tecnologia
Embora a tecnologia moderna tenha revolucionado a medicina, ela também introduz sua própria forma de fricção. Equipamentos sofisticados podem falhar ou não funcionar conforme esperado. A calibração inadequada de máquinas, falhas de software em dispositivos médicos e até problemas de energia podem criar obstáculos significativos durante uma cirurgia. Manter e operar esses equipamentos requer um nível elevado de expertise técnica e atenção constante.
“A fricção é o único conceito que distingue amplamente a guerra real da guerra no papel.” – Carl von Clausewitz
Comunicação e Coordenação
A comunicação é crucial em um centro cirúrgico, onde cada membro da equipe desempenha um papel vital. Qualquer falha na transmissão de informações pode ter consequências sérias. Mal-entendidos entre cirurgiões, anestesistas, enfermeiros e técnicos podem levar a erros críticos. A coordenação eficaz é essencial para garantir que todos os procedimentos sejam executados sem problemas, desde a preparação do paciente até a conclusão da cirurgia.
“A mais triviais coisas, vistas no contexto de uma operação militar, parecem ir contra você.” – Carl von Clausewitz
Fatores Humanos
A fricção também emerge das variáveis humanas. Fadiga, estresse e pressão emocional podem afetar o desempenho dos profissionais de saúde. Cirurgiões e enfermeiros frequentemente trabalham em turnos longos e intensos, o que pode levar a lapsos de concentração e julgamento. A capacidade de um profissional de saúde de manter a calma e tomar decisões rápidas e precisas é testada continuamente no ambiente cirúrgico.
“A guerra é o domínio da incerteza; três quartos dos fatores sobre os quais a ação é baseada estão enfiados na névoa de maior ou menor incerteza.” – Carl von Clausewitz
Logística e Suprimentos
A logística desempenha um papel crítico no funcionamento suave de um centro cirúrgico. A disponibilidade de instrumentos estéreis, medicamentos e outros suprimentos médicos é fundamental. Qualquer atraso na entrega de suprimentos ou problemas com a esterilização de instrumentos pode interromper um procedimento e aumentar os riscos para o paciente.
“A guerra é a área da atividade humana mais suscetível à fricção.” – Carl von Clausewitz
Mitigando a Fricção Cirúrgica
Assim como os comandantes militares desenvolvem estratégias para mitigar a fricção na guerra, as equipes cirúrgicas adotam várias práticas para reduzir as dificuldades inesperadas. Treinamento rigoroso e contínuo, simulações de procedimentos complexos e protocolos claros de comunicação são essenciais. Além disso, a manutenção regular de equipamentos e a implementação de sistemas de redundância podem ajudar a minimizar falhas técnicas.
“A habilidade de um líder militar reside na manutenção de uma visão clara e objetiva apesar da fricção.” – Carl von Clausewitz
A fricção cirúrgica, como descrita por Clausewitz em um contexto militar, reflete a realidade desafiadora do centro cirúrgico. Reconhecer e preparar-se para essas dificuldades é crucial para garantir a segurança do paciente e o sucesso das operações. Em última análise, a habilidade das equipes médicas em gerenciar a fricção cirúrgica determina a eficácia e a eficiência das intervenções cirúrgicas.
Charlie Munger’s 25 Cognitive Biases Applied to Digestive Surgery
In the demanding field of digestive surgery, excellence is not just a goal but a necessity. By integrating the profound insights of Charlie Munger on cognitive biases with the motivational principles of Zig Ziglar, surgeons can achieve superior performance and enhance patient care. This comprehensive guide offers actionable recommendations and illustrative examples tailored to the unique challenges of digestive surgery, ensuring that every decision is informed, balanced, and patient-centered. Charlie Munger is a renowned investor and philosopher known for his ability to identify and avoid judgment errors, often rooted in cognitive biases. For a digestive surgeon, understanding and mitigating these biases can significantly enhance clinical decision-making and performance. This summary outlines Munger’s 25 biases and provides specific examples and recommendations for surgical practice.
The 25 Cognitive Biases
- Reward and Punishment Super-Response Tendency
- Example: Opting for procedures with higher financial incentives despite less lucrative alternatives being more appropriate for the patient.
- Recommendation: Always evaluate the long-term benefits for the patient over immediate rewards.
- Liking/Loving Tendency
- Example: Ignoring a team member’s faults because you like them, compromising care quality.
- Recommendation: Maintain objective and impartial evaluations of all team members’ performance.
- Disliking/Hating Tendency
- Example: Dismissing valuable suggestions from colleagues due to personal dislike.
- Recommendation: Prioritize the efficacy of suggestions and patient safety, regardless of who proposes them.
- Doubt-Avoidance Tendency
- Example: Sticking to familiar procedures and avoiding new techniques with better outcomes due to fear of the unknown.
- Recommendation: Stay updated with best practices and be willing to explore new, evidence-based approaches.
- Inconsistency-Avoidance Tendency
- Example: Persisting with outdated surgical techniques to remain consistent with past practices.
- Recommendation: Regularly review clinical guidelines and adapt as necessary.
- Curiosity Tendency
- Example: Spending excessive time researching rare conditions not relevant to daily practice.
- Recommendation: Focus on continuous updates in areas directly related to daily clinical work.
- Kantian Fairness Tendency
- Example: Treating all cases identically without considering individual patient needs.
- Recommendation: Personalize care to meet the unique needs of each patient.
- Envy/Jealousy Tendency
- Example: Allowing jealousy of colleagues’ success to affect the work environment.
- Recommendation: Focus on personal and collaborative professional development, celebrating others’ successes.
- Reciprocity Tendency
- Example: Rewarding personal favors with clinical decisions, like preferences for shifts or cases.
- Recommendation: Maintain professionalism and base decisions on clinical and ethical criteria.
- Simple, Pain-Avoiding Psychological Denial
- Example: Avoiding discussions about poor prognoses to evade emotional discomfort.
- Recommendation: Address all clinical situations honestly and sensitively, providing appropriate support.
- Excessive Self-Regard Tendency
- Example: Overestimating personal skills and refusing assistance or second opinions.
- Recommendation: Recognize personal limitations and seek collaboration when necessary.
- Over-Optimism Tendency
- Example: Underestimating surgical risks and failing to prepare patients for potential complications.
- Recommendation: Conduct comprehensive risk assessments and communicate realistically with patients.
- Deprival-Superreaction Tendency
- Example: Overreacting to resource shortages impulsively.
- Recommendation: Plan ahead and stay calm to find effective solutions.
- Social-Proof Tendency
- Example: Adopting practices simply because they are popular among peers without assessing their efficacy.
- Recommendation: Base clinical decisions on robust evidence and recognized medical guidelines.
- Contrast-Misreaction Tendency
- Example: Underestimating a postoperative complication because it seems minor compared to a recent severe case.
- Recommendation: Evaluate each case individually and objectively, avoiding subjective comparisons.
- Stress-Influence Tendency
- Example: Making hasty decisions under high-pressure situations.
- Recommendation: Develop stress management techniques and make decisions calmly and deliberately.
- Availability-Misweighing Tendency
- Example: Making decisions based primarily on recent experiences instead of comprehensive historical data.
- Recommendation: Maintain detailed records and review long-term data to inform decisions.
- Use-It-or-Lose-It Tendency
- Example: Assuming surgical skills remain unchanged without regular practice.
- Recommendation: Regularly participate in training and simulations to keep skills up-to-date.
- Drug-Misinfluence Tendency
- Example: Underestimating the effects of postoperative analgesics.
- Recommendation: Carefully monitor medication use and adjust as needed.
- Senescence-Misinfluence Tendency
- Example: Resisting learning new surgical techniques due to age.
- Recommendation: Engage in continuous medical education and remain open to innovation.
- Authority-Misinfluence Tendency
- Example: Blindly following a senior colleague’s outdated practices.
- Recommendation: Question and validate all practices against current evidence and standards.
- Twaddle Tendency
- Example: Engaging in irrelevant discussions during surgical planning.
- Recommendation: Focus on relevant, evidence-based information.
- Reason-Respecting Tendency
- Example: Failing to explain the rationale behind surgical decisions to patients.
- Recommendation: Always provide clear, logical explanations to patients and their families.
- Lollapalooza Tendency
- Example: Multiple biases leading to a major error in patient care.
- Recommendation: Be vigilant about recognizing and mitigating multiple biases simultaneously.
- Tendency to Overweight Recent Information
- Example: Giving undue importance to the most recent piece of information received.
- Recommendation: Balance recent information with a thorough review of all relevant data.
Just as Charlie Munger highlights the importance of avoiding cognitive biases for effective decision-making, Zig Ziglar teaches us the significance of attitude and continuous improvement. For a digestive surgeon, applying these principles can transform clinical practice, leading to exceptional performance and superior patient care. Zig Ziglar said, “You don’t have to be great to start, but you have to start to be great.” Every step taken towards overcoming cognitive biases and adopting evidence-based practices is a step towards excellence. By recognizing and mitigating these 25 cognitive biases, you position yourself for an assistive performance that not only treats but truly cares for patients.
Recommendations from Zig Ziglar for Digestive Surgeons
- Believe in Yourself: “If you can dream it, you can achieve it.” Trust in your ability to learn and grow continually.
- Set Clear Goals: “A goal properly set is halfway reached.” Define clear objectives to enhance your skills and knowledge.
- Maintain a Positive Attitude: “Your attitude, not your aptitude, will determine your altitude.” Face challenges with a positive and resilient mindset.
- Learn from Every Experience: “Failure is an event, not a person.” Use every situation, good or bad, as a learning opportunity.
- Serve Others with Excellence: “You can have everything in life you want if you will just help enough other people get what they want.” Focus on patient well-being in all decisions.
By integrating Munger’s lessons and Ziglar’s motivational wisdom, you will not only become a better surgeon but also an inspiring leader and a true advocate for excellence in medicine. Remember always: “Success is doing the best we can with what we have.” Keep evolving, seeking knowledge, and above all, serving your patients with dedication and compassion. Together, let’s transform the practice of digestive surgery, one step at a time, towards the excellence our patients deserve.
Mondino de Luzzi (1270-1326) e o surgimento do MONITOR DE ANATOMIA
Mondino, oriundo de Bolonha, nasceu e concluiu seus estudos em sua cidade natal, obtendo sua graduação por volta do ano de 1290. A partir de 1306, tornou-se membro do corpo docente da universidade local. Ele recebeu instrução de Tadeu, compartilhando a mesma época de estudo com Mondeville, e dedicou-se de maneira sistemática à Anatomia, realizando dissecações públicas do corpo humano. Mondino é reconhecido como o pioneiro na “restauração” da Anatomia. Em 1316, publicou o tratado intitulado “Anothomia”, considerado o primeiro trabalho “moderno” na área, distinguindo-se por sua abordagem prática e original, diferenciando-se de simples traduções de textos clássicos.
A obra de Mondino apresenta desafios, conforme apontado por Singer (1996), destacando-se a nomenclatura confusa e as condições peculiares da dissecação naquela época. A ausência de conservantes apropriados, apesar do conhecimento acumulado pelos egípcios em técnicas de embalsamamento, tornava a dissecação um processo extenuante, preferencialmente realizado no inverno e em até quatro dias específicos para cada região do corpo.
Apesar de imprecisões anatômicas, como apontado por Friedman e Friedman (2001), Mondino desempenhou um papel crucial na instituição da dissecação como componente essencial do estudo anatômico. Essa prática foi posteriormente integrada ao currículo médico da Universidade de Bolonha, permitindo, até o final do século XVI, que as execuções de criminosos fossem realizadas de maneira que não comprometesse o trabalho anatômico, representando um avanço no uso do corpo humano na construção do conhecimento.
A contribuição de Mondino foi duradoura, pois sua obra foi uma das principais fontes de conhecimento em Anatomia humana por mais de duzentos anos, até o advento da obra de Vesalius no século XVI. Ao assumir a cátedra da disciplina, Mondino introduziu uma nova dinâmica nas aulas de Anatomia, afastando-se da dissecação e inserindo o ostensor (aluno) e o demonstrator ou incisore (técnico) para conduzirem os procedimentos, enquanto os alunos observavam.
As técnicas predominantes, como dissecação a fresco, maceração e preparações secas ao sol, eram utilizadas por Mondino e seus contemporâneos. Apesar de suas reservas quanto à maceração, essa técnica continuou a ser praticada, como confirmado pelos textos de Guido de Vigevano em 1345, representando a persistência do uso da dissecação para fins educacionais em Bolonha.
Mondino não expandiu significativamente o conhecimento anatômico existente, mas contribuiu para a formação de anatomistas que perpetuaram a tradição da disciplina em Bolonha, Pádua e em outros países. Notáveis estudiosos, como Gabrielle de Gerbi e Alessandro Achillini, aprimoraram e ampliaram as descrições anatômicas de Mondino em suas próprias contribuições.
A anatomia permanece como alicerce fundamental para o desenvolvimento da medicina ao oferecer conhecimentos cruciais para o adequada exercício profissional. O legado de anatomistas como Mondino, que enfrentaram desafios significativos em suas dissecações pioneiras, ecoa nas salas de aula modernas. A persistência do estudo anatômico é essencial para a formação médica, e os monitores de anatomia desempenham um papel vital nesse processo educativo. Atuando como elo entre a teoria e a prática, esses monitores, herdeiros contemporâneos do ostensor de Mondino, desempenham um papel crucial ao auxiliar na orientação dos alunos nas complexidades da dissecação e na compreensão da anatomia humana. Sua contribuição atual é inseparável do legado histórico, garantindo que o conhecimento anatômico continue a florescer, moldando as futuras gerações de profissionais de saúde e consolidando a anatomia como um pilar indispensável no edifício da medicina.
ODE AOS MESTRES ANATÔMICOS
Ser mestre é perpetuar juventude, Afrontando o inexorável fio do tempo, Desdobrando-se, multiplicando-se, Nas almas dos discípulos, criando ensejo.
Escolas germinam quando a maturidade, Se entrelaça à força do nobre sentimento, O mestre, sábio, fala à mente e coração, Exemplo luminoso, toque profundo, alento.
Na odisseia do saber, mestre é guia, Navegando oceanos de experiência viva, Com luz, desbrava trilhas no pensamento.
O mestre, como sol em seu zênite, Aquece a jornada do aprendizado, Conservando-se jovem, eternamente, erudito.
Assim, na sala de aula, é o comandante, Que com alma e sabedoria encanta, O mestre, semeando luz e meta.
Small desires have a life as short as the journey of those who pursue them.
The will is the road: those who want, move forward; those who don’t, justify.
Those who want find the way; those who don’t, know the reasons.
Those who want make sacrifice meaningful.
Those who don’t want declare the barriers that ease guilt.
Those who don’t want turn restriction into prohibition, limit into decision.
Those who want decide for the outcome to be achieved.
Those who don’t want decide based on the difficulty encountered.
What is challenging for one is motivating for another.
What is sacrifice for one is commitment for the other.
The challenge, for both, changes – irritating or exciting, obstacle or opportunity. Those who want accept and persist.
Those who don’t want retreat and give up.
The drive of man is his GREAT desire.
Small desires have a life as short as the journey of those who pursue them.
O Estoicismo Cirúrgico
Aplicando Princípios Filosóficos na Prática Cirúrgica
O campo da cirurgia, especialmente no tratamento das doenças do aparelho digestivo, exige não apenas habilidades técnicas refinadas, mas também resiliência emocional e ética sólida. A prática cirúrgica, por sua natureza, envolve decisões difíceis, momentos de pressão extrema e desafios inesperados. Nesse contexto, os princípios do estoicismo, filosofia praticada por pensadores como Sêneca, Epicteto e o imperador Marco Aurélio, oferecem ferramentas valiosas para que o cirurgião enfrente a complexidade emocional e ética de sua profissão.

Neste artigo, direcionado a estudantes de medicina, residentes de cirurgia geral e pós-graduandos em cirurgia do aparelho digestivo, vamos explorar como os princípios estoicos podem ser aplicados à prática cirúrgica, promovendo não apenas a eficiência técnica, mas também a excelência ética. Abordaremos as virtudes estoicas que podem moldar o comportamento de um cirurgião, aprimorando sua capacidade de lidar com adversidades e tomar decisões sábias no centro cirúrgico.
1. Aceitação das Limitações: “Primum non nocere” em Ação
O princípio estoico de aceitar o que não pode ser mudado é fundamental para o cirurgião. Em um procedimento cirúrgico, o inesperado pode surgir a qualquer momento. O estoicismo ensina que devemos focar no que está sob nosso controle – nossas ações e reações – e aceitar com serenidade aquilo que foge ao nosso alcance, como complicações imprevistas ou resultados adversos. Essa atitude fortalece o cirurgião, permitindo-lhe manter a calma e a clareza mental em situações críticas.
“O que está no meu poder é como reajo ao que acontece. O resto está fora do meu controle.” – Marco Aurélio
2. A Virtude da Perseverança em Meio às Adversidades
A cirurgia, especialmente nas doenças do aparelho digestivo, frequentemente envolve longos procedimentos, altos níveis de complexidade e a necessidade de ajustes rápidos. O estoicismo valoriza a perseverança diante de dificuldades, uma virtude essencial para o cirurgião que deve persistir no cuidado dos pacientes, mesmo em cenários complicados. A capacidade de continuar com foco e determinação, mesmo em circunstâncias adversas, é o que distingue o cirurgião estoico.
“A adversidade é uma oportunidade para a virtude.” – Marco Aurélio
3. Disciplina e Autocontrole no Centro Cirúrgico
O autocontrole é uma das virtudes centrais do estoicismo, e no campo cirúrgico, é vital que o cirurgião mantenha o controle emocional durante procedimentos complexos. O estoicismo nos ensina a não sermos controlados por emoções passageiras, como medo ou frustração, mas sim a agir com racionalidade. No centro cirúrgico, isso se traduz em decisões conscientes e calculadas, que priorizam o bem-estar do paciente, mantendo a objetividade diante de situações estressantes.
“Não é o que acontece, mas como você reage que importa.” – Marco Aurélio
4. Justiça e a Importância de Tratar Todos os Pacientes com Equidade
Para o cirurgião, a justiça, outro pilar estoico, é essencial. Todo paciente, independentemente de sua condição socioeconômica, deve receber o mesmo nível de cuidado e atenção. A prática cirúrgica ética requer que o cirurgião trate cada paciente com equidade, aplicando os princípios da medicina de maneira justa, sem preconceitos ou favoritismos. O cirurgião estoico vê em cada paciente uma oportunidade de exercer a sua profissão com justiça e integridade.
“A justiça consiste em fazer o que é correto, não o que é popular.” – Marco Aurélio
5. Coragem e Resiliência na Tomada de Decisões Difíceis
A cirurgia muitas vezes exige coragem para tomar decisões difíceis, especialmente em situações de risco à vida do paciente. A filosofia estoica valoriza a coragem como uma virtude indispensável. Para o cirurgião, isso significa enfrentar com firmeza e clareza os dilemas éticos e clínicos, mesmo quando há incertezas. A coragem estoica permite que o cirurgião aja com confiança e serenidade, tomando decisões informadas e moralmente corretas, mesmo em momentos críticos.
“A coragem é a dignidade sob pressão.” – Marco Aurélio
Conclusão
A prática cirúrgica é muito mais do que um conjunto de habilidades técnicas; é uma arte que exige um equilíbrio entre conhecimento, ética e resiliência emocional. Ao adotar os princípios estoicos, o cirurgião pode enfrentar os desafios diários com serenidade, perseverança e justiça, sempre em busca do bem maior para seus pacientes. O estoicismo oferece uma base filosófica robusta para lidar com as pressões da vida cirúrgica, fortalecendo o profissional em sua jornada por excelência técnica e moral.
“A felicidade de sua vida depende da qualidade de seus pensamentos.” – Marco Aurélio
Gostou ❔ Nos deixe um comentário ✍️, compartilhe em suas redes sociais e|ou mande sua dúvida pelo 💬 Chat On-line em nossa DM do Instagram.
#cirurgiageral #filosofiaestoica #éticaemcirurgia #estoicismonaetica #resiliencia
The Surgical Coach (P7)
Importance of OR Etiquette and Professionalism
The NOTTS emphasizes the significance of operating room (OR) etiquette and the evolution of surgical culture towards a more respectful and collaborative environment. Key points include:
- Changing Dynamics in the OR: The historical reputation of surgeons as being arrogant or demeaning, engaging in hazing practices, or displaying disruptive behavior is no longer acceptable. Modern surgeons are expected to create an atmosphere of mutual respect, trust, and communication.
- Cultural Shift towards Respect and Safety: A culture of safety and respect in the OR correlates with improved patient outcomes. It also enhances team communication, fosters professionalism, and contributes to a positive educational experience for all involved.
- Introduction to OR Etiquette: The concept of “OR etiquette” is introduced as a code of conduct among professionals that governs how they act and work together. This is distinct from manners, which are specific behaviors reflecting attitudes toward others.
- Components of OR Etiquette: The chapter covers various aspects of OR etiquette, including communication skills, leadership and followership, giving and receiving feedback, and available programs for improving team communication and culture.
- Team Members in the OR:
- Private Practice Setting: An attending surgeon, possibly with one or more assistants, which may include a second attending surgeon, certified surgical assistant (CSA), or physician assistant (PA).
- Academic Setting: Assistants may include medical students, residents, or fellows. Fellows are fully trained surgeons undergoing additional subspecialty training.
- Learning Environment: Progressive autonomy is a crucial concept, allowing learners to take on more responsibilities based on their competency level.
- Preoperative Discussion: Clear communication between the surgeon and the team members before the operation is essential. This includes discussing roles, responsibilities, and educational goals for the case.
- Patient-Centered Approach: Team members are responsible for reviewing the patient’s case in detail, understanding medical history, current disease status, medications, and diagnostic studies. A shared mental model of the operative and postoperative plan is crucial.
- Intraoperative Focus: During the operation, the patient becomes the central focus. Each team member is expected to contribute to the progress of the operation and assist others in doing the same.
- Postoperative Care Discussion: After the operation, discussions should cover postoperative care aspects, such as pain management, dietary restrictions, venous thromboembolism prophylaxis, and prescription medications.
The series posts (The Surgical Coach) aims to guide professionals in developing a positive OR culture through adherence to etiquette, emphasizing teamwork, respect, and effective communication for improved patient outcomes and a better working environment.
The Surgical Coach (P6)
Promoting a Positive OR Environment: Manners and Etiquette
Maintaining a respectful and collaborative atmosphere in the operating room (OR) is crucial for effective teamwork and patient safety. The author outlines key manners and etiquette that contribute to a positive OR environment:
- Politeness: Being courteous and considerate in interactions with colleagues fosters a harmonious atmosphere.
- Respect: Treating everyone in the OR with respect, regardless of their role or position, is essential for teamwork.
- Humility: Remaining humble helps create a collaborative environment where everyone’s input is valued.
- Learning Names: Taking the time to learn and use the names of all team members enhances personal connections.
- Offering Help: Anticipating needs and offering assistance without being asked demonstrates a proactive and cooperative attitude.
- Asking for Help: Being willing to seek assistance when needed promotes a culture of mutual support.
- Expressing Gratitude: Thanking colleagues for their contributions acknowledges their efforts and encourages teamwork.
- Patient-Centered Focus: Keeping the patient at the center of all actions emphasizes the ultimate goal of providing quality care.
Avoiding Disruptive Behavior:
- Rude, disruptive, or disrespectful behavior is not tolerated.
- Avoid yelling, making sarcastic comments, or engaging in inappropriate jokes.
- Refrain from gossiping or denigrating others.
- When playing music, be considerate of others’ preferences, and turn it off during critical times like the initial time-out.
Social Media Etiquette in the OR:
- Stay professional when using social media in the OR.
- Avoid checking Facebook or Instagram during surgery.
- Exercise caution when posting online, as anything posted can be captured and spread.
- Refrain from posting identifiable patient information.
Effective Communication and Surgical Pause:
- Ongoing effective communication among the surgical team is crucial.
- Emphasizes the importance of the surgical pause or “time-out” to establish a shared mental model.
- Recommends using a structured checklist, such as the World Health Organization Surgical Safety Checklist, during the surgical pause.
- Highlights the checklist’s positive impact on reducing mortality, complications, and hospital length of stay.
- Encourages active engagement of all team members during the checklist process.
Customizing the Checklist:
- The surgical safety checklist can be modified by hospitals or services to include relevant items specific to their patient population.
- Designated leaders should review and discuss each item, ensuring that all team members are introduced and empowered to speak up if they identify potential safety concerns.
- Customization may include a debriefing section at the end of the case to address additional items relevant to the team’s specific practices.
In summary, promoting positive manners and etiquette, avoiding disruptive behavior, and utilizing effective communication tools contribute to a culture of safety and collaboration in the OR. The surgical safety checklist serves as a valuable tool when implemented with commitment and engagement from all team members.
The Surgical Coach (P5)
The Surgery Success Pyramid: Insights from Coach Wooden
Drawing inspiration from the legendary basketball coach John Wooden and his “pyramid of success,” the author has adapted the concept to create the “surgery success pyramid.” This modified pyramid is tailored to the field of surgery, emphasizing key elements for professional and personal success.
Foundational (1st Tier) Elements:
- Industriousness: Hard work and diligence remain foundational to success in surgery.
- Friendship: Emphasizes the importance of teamwork, collaboration, and camaraderie within the surgical profession.
- Loyalty: Stresses the significance of loyalty to colleagues, patients, and the profession.
- Cooperation: Highlights the need for effective collaboration and cooperation among members of the surgical team.
- Enthusiasm: Encourages a positive and passionate approach to the practice of surgery.
2nd Tier Elements:
- Self-Control: The ability to maintain composure and discipline in challenging situations.
- Alertness: Staying vigilant and aware of the evolving surgical environment.
- Initiative: Taking proactive steps to address challenges and improve surgical practices.
- Intentness: Maintaining a focused and determined mindset toward achieving surgical goals.
While the foundational and second-tier elements retain Wooden’s original principles, modifications have been made to better reflect the nuances of the surgical profession.
Take-Home Points for Success in Surgery:
The author concludes with practical advice for success at different stages of a surgical career:
- Medical Student Success:
- Study or practice for an average of 4 hours per day.
- Write at least one paper for the literature per year.
- Engage in lab work and aim for a minimum of three papers per year.
- Read medical journals regularly.
- Strive for academic excellence, including achieving membership in one surgical association.
- Keep a journal or log of patient encounters and lessons learned.
- Prioritize physical fitness.
- Resident Success:
- Dedicate at least 2 hours a day to deliberate practice and study.
- Write one paper per clinical year and a minimum of three papers per year during lab experience.
- Be a positive deviant by identifying and improving inefficient processes.
- Keep a journal or log of valuable clinical insights.
- Maintain physical fitness and well-being.
- Fulfill all residency requirements promptly.
- Junior Faculty Success :
- Focus on mastering surgical practice.
- Seek mentorship and engage in a mentor-mentee relationship.
- Embrace new challenges in education, research, and administration.
- Plan for a full career by considering long-term well-being and financial planning.
- Prioritize life outside the hospital, spending time with family and friends.
- Contribute to the literature and engage in teaching.
- Value colleagues and foster a sense of community within the surgical field.
The author underscores the fulfillment derived from a life dedicated to surgery, emphasizing the value of hard work, continuous learning, and contributions to the field.
The Surgical Coach (P4)
Atul Gawande’s Insights: Navigating Medicine’s Core Requirements
Atul Gawande, a celebrated author known for his insightful perspectives on healthcare, especially in the surgical realm, has provided valuable insights that resonate with medical professionals. In his book “Better: A Surgeon’s Notes on Performance,” Gawande articulates three fundamental requirements for success in medicine:
- Diligence:
- Emphasizes the importance of meticulous attention to detail to prevent errors and overcome challenges.
- Do Right:
- Acknowledges that medicine is inherently a human profession, highlighting the ethical imperative to prioritize patient well-being.
- Ingenuity:
- Encourages a mindset of innovation, urging practitioners to think differently, embrace change, and learn from failures.
Gawande goes beyond defining these core requirements and offers five compelling suggestions on how individuals can make a positive impact within their professional culture:
- Ask an Unscripted Question:
- Advocates for spontaneous inquiries that can lead to unexpected discoveries and foster a culture of open communication.
- Don’t Complain:
- Advises against unproductive complaining, emphasizing that it neither solves problems nor contributes constructively to discussions. Encourages individuals to be prepared with alternative topics for discussion.
- Count Something:
- Promotes the practice of quantifying aspects of one’s work. Gawande suggests that counting something of personal interest leads to valuable insights and continuous learning.
- Write Something:
- Recognizes the transformative power of writing or typing. Encourages professionals to document experiences, insights, and reflections, enhancing both personal and collective learning.
- Change—Be an Early Adopter:
- Acknowledges the necessity of embracing change, especially in the rapidly advancing landscape of surgical technology. Urges individuals to be early adopters, staying abreast of innovations to enhance patient care.
Gawande’s guidance extends beyond the technical aspects of medicine, delving into the realms of communication, mindset, and professional development. These principles provide a roadmap for medical professionals to not only excel in their individual capacities but also positively influence the broader culture within which they operate.
The Surgical Coach (P3)
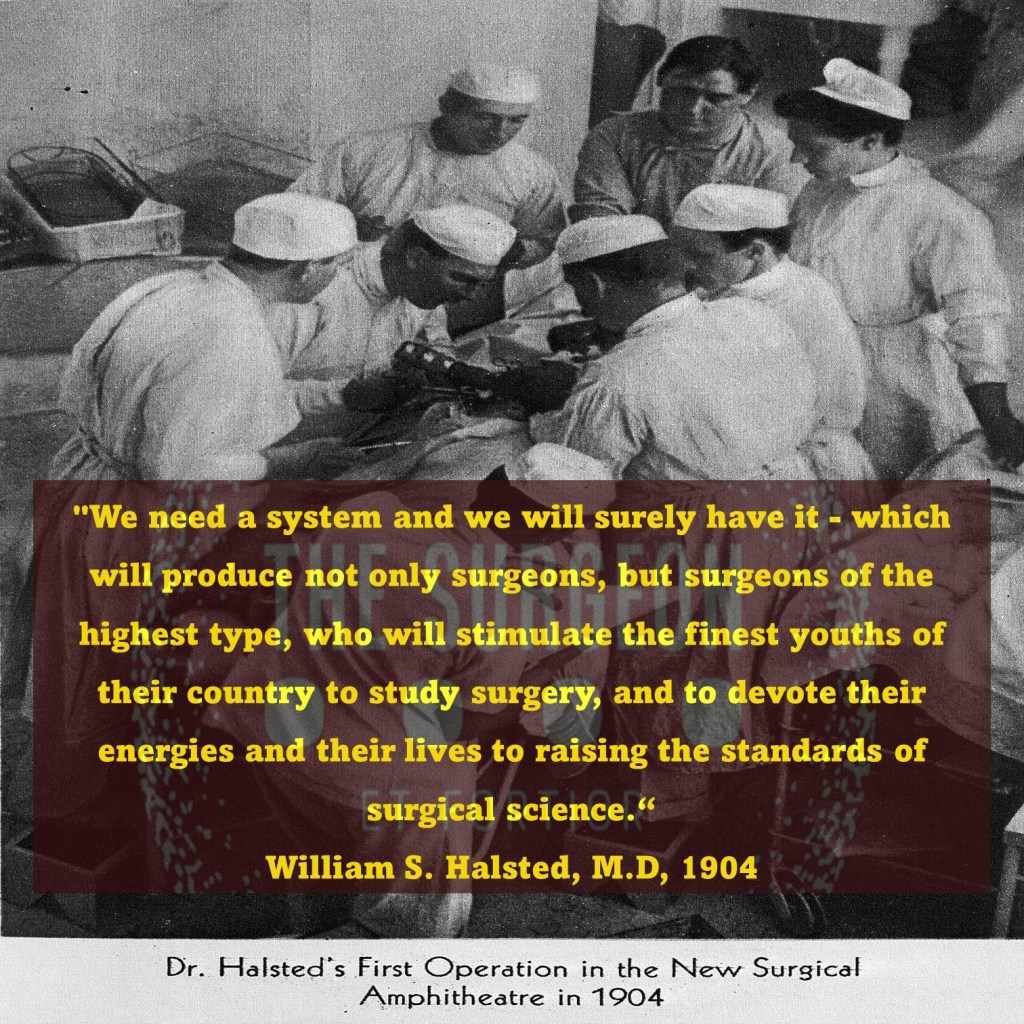
Legacy of Dr. William Stewart Halsted: Pioneer of Modern Surgery
In the annals of American surgery, the towering figure of Dr. William Stewart Halsted looms large, leaving an indelible mark on the field. Born in 1852 and educated at Andover and Yale, Halsted earned his medical degree from the College of Physicians and Surgeons in New York City in 1878. His illustrious career unfolded against the backdrop of transformative contributions to surgery, earning him the title of the “father of modern surgery.”
Innovations and Contributions 🌟💡
Halsted’s impact reverberated across various realms of surgery. He played a pivotal role in introducing cocaine’s use as a topical anesthetic, revolutionizing the management of pain during surgical procedures. His contributions to the “radical cure” of inguinal hernia, deployment of Listerian principles to reduce wound infections significantly, and groundbreaking surgeries for conditions like gallbladder disease, thyroid disease, periampullary cancer, aneurysm, and breast cancer underscore his multifaceted brilliance.
Halsted Residency Program 🏥👨⚕️
Central to his legacy is the renowned Halsted residency program, which yielded 17 chief residents within 33 years. Dr. Gerald Imber’s biography, “Genius on the Edge: The Bizarre Double Life of Dr. William Stewart Halsted,” encapsulates the complexity of Halsted’s character—rigid yet nurturing, compulsive yet negligent, and always devoted to advancing surgical science.
Halsted’s Reflections and Critique 📜🤔
In a reflective address at Yale in 1904, Halsted acknowledged the transformative strides made in surgery, with pain, hemorrhage, and infection no longer posing insurmountable challenges. However, he voiced concerns about the state of medical education in the United States, advocating for a system that produces surgeons of the highest caliber. His critique emphasized the need for reforms unburdened by tradition, offering ample opportunities for comprehensive training.
Legacy Through Teaching and Training 👩⚕️📚
Following Halsted’s passing in 1922, Dr. Rudolph Matas extolled his greatness as a clinician, scientist, and founder of a surgical school that stood unparalleled in scholarship and achievement. Matas highlighted Halsted’s unique ability to select and nurture a cadre of surgeons who would carry forth his teachings and principles.
The Goal of Training the Next Generation 🌱👩⚕️
Matas, in emphasizing Halsted’s enduring impact, touched upon a lofty aspiration—to train the next generation of surgeons for excellence. Indeed, an active surgeon’s noble pursuit involves imparting knowledge, skills, and a commitment to advancing surgical science to successors.
There Are No Time-Outs: Surgeon’s Lifelong Commitment ⏰💪
The training of a surgeon spans a lengthy, intricate, and challenging path, yet it is undeniably rewarding. Dr. Thirlby’s sentiments, expressed in his Top Ten list, echo the pride associated with surgical accomplishments. The narrative takes a turn toward addressing the often-unspoken topics of work-life balance and burnout. Dr. Thirlby reflects on the countless instances where a surgeon, even when “off duty,” is called upon to employ medical skills and surgical expertise, underscoring the ever-present nature of a surgeon’s commitment to patient care.
In the world of surgery, the white coat symbolizes an unwavering commitment. Driven by a sense of duty, surgeons find themselves intervening in various settings—restaurants, airplanes, theaters, sports fields—always ready to respond. The poignant illustration, “Once you put on the white coat, there are no substitutions, there are no time outs,” encapsulates the profound truth that defines a surgeon’s lifelong dedication to healing and serving others. 🩺👨⚕️🌐
The Surgical Coach (P2)
Mastery in Surgery: The 10,000-Hour Rule
In his acclaimed book “Outliers: The Story of Success,” Malcolm Gladwell delves into the essence of mastery, drawing attention to the 10,000-hour rule popularized by neurologist Daniel Levitin. This rule posits that a staggering 10,000 hours of dedicated practice are requisite for achieving mastery and excellence in any domain. Gladwell surveys diverse fields, from composers and basketball players to fiction writers and surgeons, finding the recurrent thread of the 10,000-hour benchmark.
The Discrepancy in Surgical Training ⏰🔍
However, in the context of surgical training, a stark contrast emerges. Graduating surgical chief residents are tasked with documenting approximately 850 cases, far from the 10,000-hour milestone. Even when considering an estimated 2 hours per case, the cumulative hours fall significantly short. Coach Carril’s emphasis on teamwork, meticulous attention, and the importance of the present moment aligns with the concept of deliberate practice. In those 850 cases, residents are encouraged to focus on refining techniques and embracing each opportunity for skill development.
Teamwork, Basics, and Deliberate Practice 🤝📚
Coach Carril’s principles echo the necessity for teamwork and concentration on fundamental aspects, resonating with Gladwell’s insights. Carril’s principle #18, emphasizing the significance of the present task, aligns with the idea of deliberate practice—immersing oneself fully in the current learning experience. Residents, akin to basketball players honing their skills, find value in focused and intentional practice to bridge the training gap.
Surgery: The Satisfying Triad of Autonomy, Complexity, and Connection 🌐💼💡
Gladwell further posits three key attributes that render work satisfying for individuals: autonomy, complexity, and a tangible connection between effort and reward. Surgery, by its very nature, encapsulates these elements. Autonomy reigns in decision-making and procedural skills, complexity manifests in the intricate facets of various surgeries, and the connection between effort and reward is evident at both the patient and practitioner levels.
The Surgeon’s Reward: A Patient’s Survival and Personal Compensation 🏥💰
At the heart of surgical satisfaction lies the profound connection between the surgeon’s effort and the patient’s well-being. Successfully navigating complex scenarios can be a gratifying reward, epitomizing the essence of surgery. Moreover, the broader efforts of a surgeon, measured in operations performed and patients attended to, correlate with personal compensation and professional recognition.
As surgical training evolves, the delicate interplay between practice, teamwork, and the intrinsic rewards of surgery remains a cornerstone. The journey to mastery may not strictly adhere to the 10,000-hour rule, but the principles of deliberate practice, teamwork, and the fulfilling nature of surgical work persist as guiding beacons in the realm of surgery. 🌟🔪
The Surgical Coach (P1)
Surgery: A Symphony of Skill and Teamwork
In the intricate realm of surgery, where years of rigorous training shape the hands and minds of general surgeons, a profound truth emerges—surgery is not a solitary endeavor. The narrative transcends beyond the operating room, highlighting the symphony of professionals within the healthcare ecosystem. As the surgeon navigates the complexities of patient care, a collaborative effort ensues, akin to the harmonious workings of a team.
Training as a Crucible for Fundamentals 🎓⚙️
Enduring the arduous journey of medical school and a demanding surgical residency, a surgeon’s arsenal is forged. Knowledge, technical prowess, and stamina become the pillars, fortifying the foundation upon which surgical practice rests. Yet, the linchpin is teamwork, a realization that dawns upon every practitioner as they step into the intricate dance of healthcare delivery.
The Surgical Maestro: Pete Carril’s Wisdom 🏀📘
Drawing inspiration from an unexpected quarter, Coach Pete Carril, the luminary basketball coach at Princeton University, becomes a beacon of wisdom. Beyond the basketball court, Carril’s teachings encapsulate universal principles applicable to life and, surprisingly, surgery. In the succinct volume, “The Smart Take from the Strong,” co-authored with Dan White and introduced by the venerable Bobby Knight, Carril imparts timeless wisdom.
25 Little Things: A Paragon for Surgery and Life 🌐📜
Coach Carril’s “25 little things to remember” echo with relevance not just in the realm of basketball but resonate in the corridors of surgery and life. Delving into a few, such as “every little thing counts,” “you want to be good at those things that happen a lot,” and “the way you think affects what you see and do,” the parallels with surgery become strikingly apparent. Carril’s philosophy becomes a guide for surgeons, emphasizing the importance of attention to detail, practice, and the profound interplay between thought and action.
Beyond the Hardwood: Surgery as a Team Sport 🤝🔬
In a synchrony reminiscent of a basketball team, the surgeon harmonizes with a chorus of healthcare professionals—nurses, anesthesiologists, support staff, administrators, and more. The cadence of success is dictated not just by individual skill but by the collective effort of the team. Vision, anticipation, and unwavering dedication converge, not only on the basketball court but also in the theater of surgery.
As Coach Carril remains a silent spectator in the hallowed halls of Princeton, witnessing a new generation striving for victory, surgeons too find inspiration in the collective pursuit of excellence. Teamwork, an indomitable spirit, and a commitment to personal and collective growth emerge as the hallmarks of success, both on the hardwood and in the operating room. 🏀🌟🔪
The Surgical Coach
Surgical Wisdom Unveiled: A Top Ten List and Commandments
Reflections on a Surgical Journey 🌟
Life’s journey is a mosaic woven with threads of guidance from parents, siblings, and mentors. This chapter transcends the mundane, embracing philosophy and personal testimony on sculpting a triumphant surgical career. Dr. Richard C. Thirlby, in the spirit of David Letterman, unfurls a top ten list that serves as a compass for aspiring surgeons.
Dr. Thirlby’s Top Ten Surgical Tenets 📜🌐
- Training is Fun (You’ll Never Forget It): A nod to lifelong learning, acknowledging the perpetual metamorphosis in surgical careers.
- Job Security: General surgeons, vital and in demand, find positions across diverse landscapes, from bustling urban centers to the serene rural expanses.
- The Pay is Not Bad: Comfortable compensation, soaring above societal averages, promises financial stability.
- Your Mother Will Be Proud of You: A familial pride resonates, extending beyond mothers to fathers, aunts, and a tapestry of family members.
- Surgeons Have Panache: Embracing the surgical personality and the unique culture that envelopes surgical realms.
- You Will Have Heroes; You Will Be a Hero: Surgeons, sculpted by influencers, reciprocate by becoming beacons of hope for grateful patients.
- There is Spirituality if You Want It: The inexplicable recoveries, the miraculous moments that defy statistical norms.
- You Will Change Patients’ Lives: A profound personal satisfaction derived from the tangible impact on patients’ destinies.
- Patients Will Change Your Life: Daily lessons from patients foster humility, nonjudgmentalism, and a continuous journey towards becoming a better human being.
- I Love to Cut: A poetic reflection of the joy derived from the meticulous artistry of surgical procedures, executed with precision for the greater good.
The Commandments of Surgical Living 🌌📜
Adding depth to the narrative, akin to timeless commandments, Dr. James D. Hardy contributes a list transcending millennia, etched in the New King James Version of the Holy Bible.
- Know Your Higher Power: An homage to the spiritual facet of life and the sanctity of the Sabbath day.
- Respect Your Roots: An acknowledgment of the significance of parents and the importance of familial bonds.
- Do No Harm: An ancient ethos resonates through the prohibition of actions such as murder, adultery, theft, lying, and coveting others’ belongings.
- Strive for Excellence: An unending pursuit of personal and professional growth, embodying efficiency, excellence, and the preservation of integrity.
- Prepare for Leadership: A call to groom leaders, emphasizing the importance of educational and professional growth.
- Nourish Professional Relationships: Recognizing the value of mentors, preserving the wisdom passed down through generations.
- Remember Your Roots: An echo from Dr. Hardy’s personal ten commandments, urging individuals to honor their origin and represent it with pride.
- Cherish Family: A gentle reminder to spend quality time with family, recognizing the profound impact of love on children.
- Spend Time Alone: Advocating for moments of solitude, fostering creative thinking and personal reflection.
- Find Joy in Your Work: A profound truth encapsulated in the sustenance derived from the daily pursuit of meaningful work one genuinely enjoys.
In this amalgamation of Dr. Thirlby’s top ten and Dr. Hardy’s commandments, a roadmap unfolds — a guide not just for a surgical career but for a fulfilling and purpose-driven life. 🌈🔍🔬
Gastrointestinal Anastomosis
Navigating the Gastrointestinal Anastomosis: A Surgical Odyssey
Unveiling the Historical Tapestry 🕰️
The creation of gastrointestinal anastomoses, an art in general surgery, has evolved over centuries. In delving into this surgical saga, fundamental principles stand tall, guiding the surgeon’s hands. This chapter unfolds the historical nuances, general tenets for successful anastomosis creation, and delves into pivotal technical considerations amidst current controversies.
The Dance of Healing and Anatomy 🩹🔍
Understanding the physiological waltz of gastrointestinal wound healing and the intricacies of intestinal wall anatomy sets the stage. An enterotomy’s inception triggers a symphony of vasoconstriction, vasodilation, and capillary changes, orchestrating the ballet of tissue healing. Granulation tissue emerges, heralding the proliferative phase, where collagen undergoes a dance of lysis and synthesis.
Layers of the Gastrointestinal Tapestry 🧵
The intestinal wall, a multilayered tapestry, unravels its secrets. The serosa, a connective tissue cloak veiled by mesothelial lining, demands precise apposition to thwart leakage risks. The submucosa, the stronghold of tensile strength, anchors the sutures knitting the anastomosis. Intestinal mucosa seals the deal, driven by epithelial cell migration and hyperplasia, crafting a watertight barrier.
Local Factors: Paving the Path to Healing ⚒️🩹
The local factors influencing this symphony include intrinsic blood supply and tension management. Adequate blood supply, a lifeline for tissue oxygenation, hinges on meticulous surgical technique. Tension, a delicate partner in this dance, demands finesse; too much jeopardizes perfusion, too little invites inflammatory infiltrates. The colon, in particular, demands a surgeon’s nuanced touch.
Systemic Harmony: The Ripples of Patient Factors 🔄🌊
Systemic factors contribute their ripples to this surgical pond. Hypotension, hypovolemia, and sepsis compose a dissonant note affecting blood flow and oxygen delivery. Patient-specific variables — malnutrition, immunosuppression, and medication use (hello, steroids and NSAIDs) — compose a subplot, influencing the narrative of wound healing.
As the surgeon steps into this intricate ballet of anastomosis creation, history, physiology, and patient-specific factors converge. Each suture, each decision, shapes the narrative of healing. The gastrointestinal odyssey continues, blending tradition with innovation, as surgeons embark on the timeless quest for successful anastomoses. 🌐🔍🩺
Pre Surgical Evaluation of BLEEDING
Unraveling Bleeding Risks: A Surgical Odyssey
In the realm of surgical care, meticulous assessment of bleeding risk is paramount. The age of onset of bleeding and the specific sites affected offer crucial clues, helping differentiate between inherited and acquired bleeding disorders. Inherited disorders, often manifesting in childhood, may lurk beneath the surface, surfacing during surgical trauma in adulthood.
Decoding the History 🕰️
Interrogating the patient’s history unveils key insights. Medication usage, both prescription and over-the-counter, unfurls potential contributors to bleeding events. Family history provides a roadmap for inheritance patterns, crucial in diagnosing disorders like hemophilia. The severity of past bleeding incidents serves as a yardstick, guiding expectations during surgical challenges. Comorbidities, especially liver and kidney dysfunction, loom large in magnifying bleeding risks.
The Physical Symphony 🩺🎶
While the physical exam plays a supportive role, it may hint at platelet disorders through findings like petechiae and ecchymoses. Platelet function issues or deficiencies may manifest similarly, emphasizing the importance of a comprehensive history. Single-site bleeding tends to be non-indicative of a bleeding disorder, while multisite bleeding raises red flags.
Laboratory Pilgrimage 🧪
A pilgrimage through laboratory tests offers a comprehensive snapshot of hemostatic competence. Assessing platelet count, complete blood count (CBC), platelet function, aPTT, PT, and fibrinogen levels becomes the map for surgical decisions.
Unmasking Causes of Excessive Surgical Bleeding 🚩
Most patients enter the operating room with normal hemostasis. However, certain surgeries, like liver transplants or trauma interventions, may trigger consumptive coagulopathy. Preexisting hemostatic defects, especially congenital bleeding disorders like hemophilia and von Willebrand disease, require keen suspicion.
Hunting the Culprit: Acquired Bleeding Disorders 🎯
Liver disease emerges as a common instigator of coagulation abnormalities, while anticoagulant therapies like Coumadin and heparin cast shadows on surgical hemostasis. Acquired thrombocytopenia, often linked to splenomegaly or medications, and platelet function disorders, especially induced by aspirin and clopidogrel, populate the landscape of surgical challenges.
Navigating Intraoperative Waters ⚓🔍
Intraoperative bleeding may cascade from shock, massive transfusions, or acute hemolytic reactions. Hemostatic agents, from gelatin sponge to topical thrombin, stand as stalwart navigators through these turbulent waters.
Postoperative Chessboard: A Risky Endgame ♟️🩹
Postoperative bleeding, often stemming from inadequate hemostasis, unveils additional players. Residual heparin, altered liver function, and acquired clotting factor deficiencies post-hepatectomy amplify the stakes. Fibrinolysis disorders may also cast shadows post-surgery.
Dancing with Disseminated Intravascular Coagulation (DIC) 🩸🎭
DIC, a theatrical presentation of intravascular coagulation gone awry, demands a spot on the stage. Prompt recognition and addressing precipitating factors are pivotal, with cryoprecipitate and platelet transfusions standing as protagonists.
Fibrinolytic Fantasia: When Clotting Goes Amiss 🌪️🩹
Primary and secondary fibrinolysis emerge as culprits in postsurgical bleeding, often linked to lytic therapy, severe liver failure, or DIC. Managing fibrinolytic storms necessitates tailored interventions.
Hypercoagulable Waltz in Surgical Limelight 💃🕺
A careful dance with thromboembolism risks follows, accentuating the importance of patient history in unraveling congenital and acquired hypercoagulable states. A familial narrative often unravels the genetic predispositions steering this intricate choreography.
In the surgical arena, every patient’s hemostatic tale unfolds uniquely. Through history, examination, and laboratory revelations, surgeons navigate the delicate balance between bleeding and clotting, ensuring a symphony of healing amidst the surgical odyssey. 🌐🔍🩺
Nutritional Surgical Care
Navigating the Nutritional Maze in Surgical Care 🌐🔍
Surgeons bear the responsibility of caring for patients whose nutritional status may be compromised, influencing their ability to heal optimally. The challenges encompass an array of issues, including anorexia, inanition, gluconeogenesis acceleration, hyperglycemia, insulin resistance, and electrolyte and hormonal imbalances. These factors intricately impact surgical responses and a patient’s healing capacity. Let’s delve into the complex world of digestive tract, esophageal, gastric, intestinal, and other surgeries, exploring how they interplay with nutritional considerations.
Digestive Tract Surgery 🍽️
The digestive tract, a bustling center of metabolic activity, plays a pivotal role in nutrient digestion, absorption, and metabolism. Surgical interventions involving the gastrointestinal (GI) tract can lead to malabsorption and maldigestion, causing nutritional deficiencies. Understanding the site of nutrient absorption aids in identifying potential postoperative deficiencies. Enhancing nutritional status before surgery becomes crucial for a smoother postoperative recovery.
Esophageal Surgery 🥄
Various conditions affecting the esophagus, from corrosive injuries to obstruction, necessitate surgical intervention. Procedures involve replacing the esophagus with the stomach or intestine, each carrying unique considerations. Nutritional support, including nasoenteric feeding tubes or parenteral nutrition (PN), may be necessary preoperatively for obstructed esophagi, with additional intraoperative measures for optimal postoperative outcomes.
Gastric Surgery 🥢
Gastric surgical procedures, while addressing specific issues, can potentially lead to malnutrition. Patients may experience dumping syndrome, requiring dietary modifications and cautious fluid intake. Anemia and metabolic bone diseases are common consequences, demanding periodic injections and calcium-vitamin D supplementation. Understanding postgastrectomy dietary modifications and careful fluid management becomes paramount.
Intestinal Surgery 🍴
Resection of excessive lengths of the intestine, especially in short bowel syndrome, can result in severe malabsorption and malnutrition. Long-term PN might be necessary to maintain nutritional balance. Pancreaticoduodenectomy, a complex surgery, requires postoperative monitoring for complications like delayed gastric emptying, diabetes mellitus, and malabsorption, influencing nutrient guidelines.
Ileostomy and Colostomy 🚽
Procedures like ileostomy or colostomy, creating artificial anuses, are employed for various intestinal issues. Patients with ostomies generally follow regular diets, with adjustments based on stoma output. High-output ostomies necessitate specific dietary precautions to manage fluid levels. Nutritional assessment’s crucial role in surgical outcomes emphasizes the growing interest in tailored preoperative nutritional support and the potential resurgence of parenteral nutrition.
Conclusion 🩺💡
Understanding the intricate dance between surgical interventions and nutritional considerations is paramount for surgeons and medical practitioners. As regulatory scrutiny intensifies, the role of nutrition in preventing complications and improving outcomes will likely take center stage, emphasizing the importance of personalized nutritional strategies in the surgical journey. 🌟💪
Tubes and Drains
Unlocking the World of Tubes and Drains in Medical Practice 🩹
Understanding the diverse array of tubes and drains is crucial for any medical practitioner, and it all begins with appreciating the French size system, where the outer diameter of a catheter is denoted. A quick calculation (French size multiplied by 0.33) reveals the catheter’s outer diameter in millimeters.
Gastrointestinal Tract Tubes 🍽️
Starting with nasogastric tubes designed to evacuate gastric contents, these are frequently employed in patients facing ileus or obstruction. Modern nasogastric tubes often incorporate a sump function, preventing suction locks and enhancing efficiency. Nonsump tubes, though less common, may be used for intermittent suction. Nasogastric tubes also serve in feeding, with soft, fine-bore tubes being preferred for this purpose. Nasoenteric tubes, intended for feeding, require careful attention to safety during instillation.
Nasobiliary tubes, often placed endoscopically, aid in biliary drainage in cases of obstruction or fistula. T-tubes within the common bile duct ensure closed gravity drainage. Gastrostomy tubes, placed surgically or via percutaneous endoscopic gastrostomy (PEG), find utility in drainage or feeding. Jejunostomy tubes, inserted surgically or endoscopically, are vital for long-term nutritional access.
Respiratory Tract Tubes 🫁
Chest tubes play a pivotal role in pleural cavity drainage, addressing issues like pneumothorax, hemothorax, or effusion. The three-bottle system facilitates constant suction, drainage, and prevention of air entry, crucial for maintaining a water seal.
Endotracheal tubes, cuffed for a secure tracheal seal, cater to short-term mechanical ventilation needs in adults. Tracheotomy tubes, directly inserted into the trachea through the neck, become essential for prolonged mechanical ventilation or when maintaining a patent airway is challenging.
Urinary Tract Tubes 🚰
Bladder catheters, commonly known as “Foley” catheters, serve to straight drain urine. Nephrostomy tubes, placed in the renal pelvis, drain urine above obstructions or delicate ureteral anastomoses. Percutaneously placed tubes, often pigtail catheters, assist in draining abscesses, typically guided by interventional radiologists.
Surgical Drains 🌡️
Closed suction drains, such as Jackson-Pratt and Hemovac, prove invaluable for evacuating fluid collections during surgery. Sump suction drains, like Davol drains, are larger and designed for continuous suction in scenarios with thick or particulate drainage. Passive tubes, exemplified by Penrose drains, offer a pathway for fluid without applied suction, serving as a two-way conduit for bacteria. Understanding these various tubes and drains is pivotal for medical practitioners navigating complex clinical scenarios. 💉💊
The Geriatric Patient
Navigating Surgical Challenges in an Aging Population: A Delicate Balance 🌐
The ongoing aging process within the American population brings forth a set of unique challenges that surgeons must adeptly navigate for decades to come. Elderly individuals, compared to their younger counterparts, often exhibit diminished physiological reserves. Their health is frequently influenced by medications that can alter normal physiological responses, such as β-blockers, or impact surgical outcomes, like warfarin or platelet aggregation–inhibiting agents. Additionally, baseline impairments, ranging from sensory issues to difficulties in ambulation or dementia, may complicate their ability to engage in everyday activities.
One perplexing dilemma faced by surgeons when caring for elderly patients revolves around the decision to pursue an aggressive intervention plan. Transparent communication between the patient and physician is paramount in determining the appropriate level of aggressiveness in the patient’s best interest. This conversation takes on heightened significance in the elderly population. Engaging in repeated discussions with patients and their families, starting before surgery and extending into the postoperative phase, is crucial. Generally, patients express a desire for aggressive medical care as long as there remains a reasonable chance for meaningful survival.
While these discussions may be uncomfortable, they are as integral to the patient’s care as any aspect of their medical history. It is imperative to recognize that surgical care is provided by individuals who genuinely care about the patient’s overall well-being. In certain situations, medical care may prioritize alleviating pain over prolonging life. Ideally, these conversations should occur in a serene and comfortable setting, free from distractions.
Moreover, it is essential to underscore that discussions about end-of-life matters are not legal proceedings. No forms need to be signed. These discussions are akin to any other conversation between a doctor and a patient regarding their care. The dialogue involves a careful consideration of the strengths and weaknesses of different approaches until a collaborative plan of action is determined. The only distinction lies in the profound nature of end-of-life discussions, offering patients the best opportunity to shape their destinies. Consequently, these discussions should be approached with the utmost reverence, acknowledging the gravity of the subject matter. 🤝💙
Estabelecendo Conexões Essenciais 💬
Técnicas de Entrevista na Medicina: Estabelecendo Conexões Essenciais 💬
A relação médico-paciente é uma parte vital do cuidado cirúrgico. O vínculo entre o cirurgião e o paciente deve ser construído, mantido e valorizado. Boas técnicas de entrevista são fundamentais para estabelecer essa relação. O alicerce para uma boa entrevista advém de uma preocupação genuína com as pessoas. Embora existam habilidades de entrevista que podem ser aprendidas, a qualidade da interação pode ser aprimorada. Estudantes de medicina devem reconhecer seu papel especial no cuidado do paciente, não se envergonhando de sua posição e compreendendo que são membros eficazes da equipe. Pacientes frequentemente veem os estudantes de medicina como acessíveis, compartilhando detalhes que poderiam ocultar de membros mais seniores da equipe. O papel do estudante é descobrir as queixas médicas principais do paciente, realizar uma história e exame físico focalizados e apresentar os achados à equipe. Uma entrevista eficaz requer a comunicação sobre quem você é e como se encaixa na equipe. 🏥
Desafios da Entrevista na Medicina: Adaptando-se a Diferentes Ambientes 🌐
Entrevistar bem pode ser desafiador devido à variedade de ambientes, como sala de cirurgia, unidade de terapia intensiva, consultório particular, leito hospitalar, sala de emergência e ambulatório. Cada ambiente apresenta desafios únicos à comunicação eficaz. Para construir boas relações médico-paciente, cirurgiões ajustam seus estilos a cada ambiente e à personalidade e necessidades de cada paciente. Algumas regras básicas são comuns a todas as entrevistas profissionais. A primeira regra é deixar claro ao paciente que, durante a história e o exame, nada além de uma emergência de vida ou morte terá maior importância do que a interação entre o cirurgião e o paciente naquele momento. Este é o primeiro e melhor momento para conectar-se com o paciente. É crucial que o paciente compreenda que um cirurgião cuidadoso, conhecedor e dedicado será seu parceiro na jornada pelo tratamento de doenças cirúrgicas. O cirurgião deve observar outras regras, incluindo dar atenção adequada à aparência pessoal para transmitir uma imagem profissional que inspire confiança, estabelecer contato visual, comunicar interesse, calor e compreensão, ouvir de forma não julgadora, aceitar o paciente como pessoa, ouvir a descrição do problema do paciente e ajudar o paciente a se sentir confortável na comunicação. 👩⚕️👨⚕️
Primeiros Minutos: Estabelecendo uma Base Sólida 🤝
Ao receber o paciente em um ambiente ambulatorial, os primeiros minutos são dedicados a cumprimentar o paciente pelo nome formal, apertar as mãos, se apresentar e explicar o papel do cirurgião. A atenção à privacidade do paciente, ajustando o estilo de conversação e o vocabulário às necessidades do paciente, descobrindo a atitude do paciente em relação à clínica, conhecendo a ocupação do paciente e entendendo o que o paciente sabe sobre sua condição são passos fundamentais. A seguir, ocorre a exploração do problema, movendo-se de perguntas abertas para perguntas fechadas. Técnicas importantes incluem o uso de transições, fazer perguntas específicas e claras e reformular o problema para verificação. É crucial determinar se o paciente tem alguma pergunta. No final da entrevista, o cirurgião explica quais serão os próximos passos e que realizará um exame no paciente. Por fim, verifica-se se o paciente está confortável. 🌟
Diferenças nos Ambientes de Atendimento: Adaptação e Compreensão 🏨
As técnicas utilizadas em ambientes ambulatoriais são igualmente adequadas para encontros em ambientes hospitalares e de pronto-socorro. Geralmente, mais tempo é dedicado ao paciente nas entrevistas iniciais e subsequentes do que em um ambiente ambulatorial. Na entrevista inicial, os pacientes podem estar com dor, preocupados com problemas financeiros e ansiosos com a falta de privacidade ou dietas desagradáveis. Eles também podem ter dificuldade para dormir, sentir medo do tratamento ou se sentir impotentes. É importante comunicar gentil e confiantemente o propósito da entrevista e quanto tempo levará. O paciente não apenas escuta, mas também observa o comportamento e a vestimenta do médico. O ambiente também afeta a entrevista. Por exemplo, um ambiente apertado, barulhento e lotado pode afetar a qualidade da comunicação. Pacientes podem ter sentimentos negativos devido a insensibilidades por parte do médico ou de outras pessoas. É fundamental evitar falar com o paciente na entrada do quarto, dar ou receber informações pessoais em um ambiente lotado, falar sobre um paciente em um elevador ou em outro espaço público, ou falar com um paciente sem fechar a cortina em uma enfermaria. 🌆
Conclusão: Construindo Relações de Confiança na Medicina 🌐
Em resumo, dominar as técnicas de entrevista na medicina é essencial para construir relações sólidas entre médico e paciente. Os cirurgiões habilmente ajustam suas abordagens a diferentes ambientes e personalidades dos pacientes, aplicando regras básicas universais. Os primeiros minutos são cruciais para estabelecer uma base sólida, enquanto a exploração cuidadosa do problema requer uma transição de perguntas abertas para fechadas. Adaptações ao ambiente e compreensão das preocupações do paciente são vitais para uma comunicação eficaz. Ao incorporar essas técnicas, os médicos podem garantir que a interação médico-paciente seja centrada no paciente, transmitindo confiança e dedicação à jornada conjunta pelo tratamento. 👨⚕️🤝👩⚕️
Navigating Your Clinical Experience in Surgery
Transitioning to the Role as a Junior Member of the Surgical Health Care Team: Navigating Your Clinical Experience in Surgery
Embarking on your surgical clerkship is an immersive clinical journey that extends beyond aspiring surgeons. This experience is a valuable opportunity to refine essential clinical skills applicable to any medical specialty. As you progress in your medical career, encounters with patients requiring surgical intervention will be inevitable. The insights gained during your surgery clerkship will empower you to identify surgical diseases, understand the need for surgical consultations, and develop empathy for the emotional, physiological, and logistical aspects patients and their families may face during operations or consultations.
Approaching Your Role: A Shift in Learning Dynamics
As a seasoned learner in medical school, your entry into the health care team during your 3rd year marks a profound transition. The focus is no longer solely on memorization; it now involves understanding patients’ complaints and diseases. Balancing voluminous information, time constraints, and determining the depth of knowledge required for patient care present unique challenges. Successful clinical performance is influenced by various factors:
- Preparatory Coursework and Experience: Constructing new knowledge relies on existing foundations. Deep knowledge, especially in anatomy, facilitates a seamless connection between new information and prior understanding.
- Quality of Study Methods: Active learning demands taking responsibility for your education. Maintaining a disciplined study plan aligned with your learning style is essential.
- Organizational Skills: Successful learners adeptly manage time and priorities to avoid last-minute cramming, reducing stress.
- Motivation and Emotion: Enthusiasm and positive feelings toward content, team, and environment significantly impact the clerkship experience and how you are perceived by patients and the team.
- Physical Health: The link between physical well-being and effective learning underscores the importance of attending to personal health needs.
- Distractibility and Concentration Skills: Active engagement in learning, whether through reading or listening, is crucial for processing and translating information into meaningful knowledge.
Maximizing Your Learning: Strategies for Success
1. Prepare, Practice, and Review:
- Preparation: Activate prior knowledge by pre-reading about upcoming topics, enhancing comprehension, and fostering long-term memory.
- Practice: Actively engage in learning, take notes, and generate questions. Studies show that self-generated notes enhance retention.
- Review: Ongoing review, coupled with self-assessment using test questions, patient management problems, and creating personal tests, reinforces information.
2. Organize Your Knowledge:
- Get the Big Picture: Familiarize yourself with learning objectives, chapter headings, and subheadings before reading. Listing questions beforehand guides focused reading.
- Review Charts and Diagrams: Key information in charts and diagrams aids study. Testing yourself on missing information enhances understanding.
- Emphasize Integration: Relate new information to patient encounters, lectures, or images. Create mind maps to organize information and identify patterns.
3. Know Expectations and Thyself:
- Clarify your role and responsibilities by reviewing syllabus materials and seeking guidance from experienced peers, residents, or faculty.
- Define personal learning goals and learning style, being proactive in your approach to studying.
4. Ask! Ask! Ask!:
- Be persistent and assertive in seeking clarification, feedback, or assistance.
- Utilize the wealth of expertise within the surgical team, including nurses, physician assistants, pharmacists, social workers, and technicians.
Maximizing Your Emotional Intelligence: Strategies for Well-Being
1. Focus Forward with a Positive Attitude:
- Make decisions with a positive end in mind, maintaining situational awareness in varied scenarios.
- Cultivate open-mindedness, positive energy, and enthusiasm to contribute constructively to patient care and the team.
2. Set Goals and Celebrate Successes:
- Define short- and long-range goals, including personal, financial, and relationship goals.
- Document achievements, reinforcing a sense of accomplishment and self-confidence.
3. Promote a Supportive Learning Environment:
- Take responsibility for mistakes, learn from them, and foster trust within the team.
- Avoid negativity by steering clear of individuals with persistent negative attitudes or behaviors.
In conclusion, approach your surgery clerkship with a proactive mindset. Maximize both your intellectual capabilities and emotional intelligence to derive the utmost benefit from this transformative experience. Keep in mind the wisdom of John Wooden, emphasizing the importance of being the best version of yourself. This principle not only ensures success in your surgery clerkship but resonates throughout your medical journey.
The Stoic Surgeon: Drawing Inspiration from Marcus Aurelius in Medical Practice
Introduction
The practice of medicine and surgery, while profoundly rewarding, can also be challenging and emotionally demanding. In these moments, many professionals seek guidance and inspiration to navigate the inherent difficulties in human healthcare. A rich source of timeless wisdom can be found in the words of the philosopher-emperor Marcus Aurelius, whose Stoic teachings resonate powerfully in the context of contemporary medicine. Let’s explore how Marcus Aurelius’s ideas can illuminate and fortify medical and surgical practice.
Development
- “What we control is what we calmly accept.” – In moments of uncertainty and pressure in the operating room, the serene acceptance of circumstances is crucial for maintaining composure and focus.
- “Do not expect the doctors to do everything for you.” – Marcus Aurelius reminds us of the importance of recognizing our own limitations. Collaboration between doctor and patient is essential for effective treatment.
- “Pain is inevitable. Suffering is optional.” – When dealing with patients in painful situations, it’s vital to remember that our role extends beyond physical treatment to emotional support and alleviating suffering.
- “Doing what needs to be done when it needs to be done, to the best of our ability, is already enough.” – In a profession as demanding as medicine, it’s vital to remember that every effort dedicated to patient care is valuable and meaningful.
- “What is morally right is more important than what is legally right.” – In some situations, it may be necessary to make decisions that go beyond protocol, aiming for the best interest of the patient.
- “To wait is harmful. Not to wait is necessary.” – Readiness and agility in making medical decisions can be crucial in emergency situations.
- “Time is a river, and facts are currents; we cannot escape, we cannot choose where we will go, nor when, nor how.” – This reflection reminds us of life’s impermanence and the importance of cherishing every moment in medical practice.
- “Man’s health is our treasure.” – Marcus Aurelius emphasizes the valuable responsibility doctors have in preserving and restoring individuals’ health.
- “Every day that dawns brings some evil, which we must accept, for no day will be without it.” – Recognizing that challenges are part of the medical journey allows professionals to face them with courage and determination.
- “Where is the good, if not in doing good to those in need?” – The practice of medicine is a living testament to compassion and altruism. Through it, doctors have the opportunity to demonstrate the true essence of human kindness.
Conclusion
Just as Marcus Aurelius faced the challenges of the Roman Empire with serenity and wisdom, the modern surgeon finds in his words a guide to practicing medicine with virtue and humanity. By uniting technical skill with Stoic philosophy, the surgeon becomes not only a master of their craft but also an example of Stoic activity for the entire medical community. May each operating room be a temple of virtue and care, where the legacy of Marcus Aurelius lives on through the hands of Stoic surgeons.
The Art of Healing: Wisdom from Opus Dei for Medical Professionals
1. “Work is a path to holiness.” – Just as in Opus Dei, where work is considered a means to grow closer to God, in the field of medicine, every interaction with a patient, every diagnosis, and every surgery is an opportunity to serve and make a positive impact.
2. “In your daily work, offer up small sacrifices for your patients.” – Much like Opus Dei encourages offering up small sacrifices for spiritual growth, in medicine, dedicating extra time, attention, or effort for a patient’s well-being can be a powerful form of compassion.
3. “Strive for excellence in your field; it is a reflection of your dedication to your patients.” – Opus Dei emphasizes the pursuit of excellence in one’s profession as a form of service to God. Similarly, in medicine, continuous learning and improvement directly benefit the quality of care provided to patients.
4. “Treat each patient with dignity, respect, and kindness.” – This fundamental principle aligns with Opus Dei’s emphasis on valuing every individual. In medicine, showing compassion and empathy is as important as clinical expertise.
5. “Pray for guidance in making difficult decisions.” – Just as Opus Dei encourages seeking spiritual guidance in challenging situations, in medicine, turning to one’s faith for moral and ethical dilemmas can provide clarity and a sense of purpose.
6. “Foster a culture of trust and collaboration among colleagues.” – Opus Dei emphasizes unity and mutual support among its members. Similarly, in the medical field, teamwork and open communication are vital for providing the best possible care for patients.
7. “Never underestimate the power of a kind word or gesture.” – Small acts of kindness, like those encouraged in Opus Dei, can have a profound impact on a patient’s experience and recovery in the medical setting.
8. “Cultivate a spirit of gratitude for the opportunity to serve others.” – Recognizing the privilege of being able to heal and alleviate suffering is a perspective shared by Opus Dei and medical professionals alike.
9. “Strive for balance between professional and personal life.” – Opus Dei emphasizes the importance of a balanced life. In medicine, maintaining a healthy work-life balance is crucial for sustaining a long and fulfilling career.
10. “Embrace the challenges of medicine as opportunities for growth and service.” – Opus Dei encourages embracing life’s challenges as a means of spiritual growth. Likewise, in medicine, facing the complexities and difficulties of healthcare with dedication and compassion can lead to profound personal and professional development.
Incorporating these principles from Opus Dei into the practice of medicine can not only enhance the quality of care provided but also contribute to a more compassionate and fulfilling healthcare experience for both practitioners and patients alike.
Liderança Inspiradora de Lord Nelson: Lições para Cirurgiões Contemporâneos
A história nos presenteou com inúmeros líderes notáveis, cujas habilidades e características têm inspirado gerações ao longo dos séculos. Um desses ícones é Lord Nelson, o lendário almirante britânico do século XVIII, conhecido por sua coragem e maestria tática nas batalhas navais. Surpreendentemente, as características de liderança de Lord Nelson têm aplicações valiosas mesmo na prática contemporânea da cirurgia. Neste artigo, exploraremos algumas dessas qualidades e como nós cirurgiões podemos aplicá-las para alcançar o sucesso em nossas batalhas cirúrgicas.
“Eu sou inabalável em minha determinação, como nunca estive em minha vida, desde que coloquei o pé no convés de um navio.”
1. Determinação Inabalável: Lord Nelson era conhecido por sua determinação inabalável em alcançar seus objetivos. Ele enfrentou inúmeras adversidades e desafios durante suas batalhas navais, mas nunca desistiu diante das dificuldades. Os cirurgiões contemporâneos podemos aprender com essa qualidade, mantendo-se resilientes diante de obstáculos, buscando soluções mesmo nas situações mais desafiadoras e garantindo o melhor atendimento possível para nossos pacientes. Durante a Batalha do Nilo, em 1798, Nelson enfrentou condições adversas quando a frota britânica ficou encalhada em bancos de areia. Enfrentando uma situação aparentemente desesperadora, ele permaneceu determinado a superar os obstáculos para alcançar a vitória. Com habilidades táticas brilhantes, Nelson conseguiu finalmente manobrar sua frota para fora dos bancos de areia e alcançar uma vitória decisiva sobre a frota francesa.
“Eu sempre fui um covarde em tudo, exceto nesta profissão.”
2. Coragem sob Pressão: Durante a Batalha de Copenhague, em 1801, Nelson foi ordenado a se retirar pelo comandante em chefe, mas ele ignorou a ordem e ergueu o telescópio em seu olho cego para afirmar que não conseguia ver o sinal. Ele então liderou seu esquadrão em um ataque corajoso, superando uma poderosa defesa dinamarquesa. Sua determinação e coragem sob pressão foram fundamentais para a vitória britânica. Em meio ao caos e perigo das batalhas navais, Lord Nelson demonstrou coragem excepcional. Seu exemplo inspirador pode nos lembrar da importância de permanecermos calmos e focados, mesmo durante procedimentos complexos ou emergências médicas. A coragem para tomar decisões rápidas e precisas pode fazer a diferença entre a vida e a morte em uma sala de cirurgia.
“A vontade não pode ser chamada de coragem, mas dever, o resultado da força da mente; e qualquer um que possua esse poder, quando chega a hora de agir, encontrará a coragem que necessita.”
3. Liderança Carismática: Lord Nelson conquistou o respeito e a admiração de sua tripulação com sua liderança carismática. Durante a Batalha do Nilo, quando o perigo era iminente e a tripulação estava nervosa, Nelson subiu ao convés e enfrentou corajosamente o inimigo, encorajando seus marinheiros a seguirem seu exemplo. Sua presença inspiradora foi fundamental para manter o moral elevado e motivar sua equipe a lutar com determinação. Lord Nelson era conhecido por sua liderança carismática e inspiradora. Ele conquistou o respeito e a lealdade de sua tripulação com sua empatia e capacidade de se conectar emocionalmente com seus marinheiros. Os cirurgiões contemporâneos também podem se beneficiar ao desenvolver uma liderança que inspire confiança e motivação em suas equipes médicas, promovendo um ambiente colaborativo e eficiente.
“Eu planejo que cada homem atue de acordo com o que vê melhor, mas qualquer homem que venha entre as duas frotas, não pode ser errado, portanto, não pode ser chamado de insubordinação, mas uma obediência em que cada oficial julga por si mesmo o que é melhor a ser feito.”
4. Capacidade de Adaptação: Durante a Batalha de Trafalgar, a estratégia inicial de Nelson era enfrentar a frota inimiga de maneira mais tradicional. No entanto, quando percebeu que a formação inimiga era mais forte do que o esperado, ele rapidamente adaptou sua tática e implementou a “manobra de Nelson”, cortando a linha inimiga e concentrando seu poder de fogo para alcançar a vitória. Durante suas batalhas, Lord Nelson enfrentou situações imprevistas e mudanças de planos. Sua capacidade de adaptação e flexibilidade permitiu-lhe ajustar suas estratégias conforme necessário. Na cirurgia contemporânea, os profissionais também devem ser ágeis e adaptáveis, prontos para responder a mudanças repentinas durante procedimentos cirúrgicos complexos ou emergências médicas.
“Seja qual for a estação em que você estiver, carregue consigo o pensamento de que todos os olhos estão voltados para você. Comande a si mesmo sempre que for o exemplo de todos os outros.”
5. Comunicação Efetiva: Lord Nelson era conhecido por sua habilidade de comunicação clara e direta com sua equipe. Antes da Batalha do Nilo, ele escreveu uma carta aos marinheiros enfatizando a importância da vitória e oferecendo palavras de encorajamento. Sua mensagem sincera e motivadora demonstrava sua preocupação com o bem-estar de sua tripulação e ajudou a criar um senso de propósito comum entre seus homens. A comunicação efetiva era uma das principais características de liderança de Lord Nelson. Ele sabia como transmitir suas ordens com clareza e também valorizava o feedback de sua equipe. Cirurgiões contemporâneos podem seguir esse exemplo, enfatizando a comunicação transparente com seus colegas e pacientes para garantir que todos estejam alinhados quanto aos procedimentos e tratamentos.
Em suma, a história de Lord Nelson nos ensina que as características de liderança transcendem as épocas e têm aplicação valiosa em diversas áreas, incluindo a medicina. Ao incorporar a determinação, coragem, carisma, adaptação e comunicação efetiva de Lord Nelson, podemos nos inspirar e tornar líderes excepcionais em nossas práticas médicas, promovendo um atendimento de qualidade e impactando positivamente a vida dos pacientes. A frase ‘A Inglaterra espera que cada um faça sua parte’ tornou-se um lema inspirador e atemporal, capturando a essência da liderança de Lord Nelson na Batalha de Trafalgar. Essas palavras ecoam através dos séculos, lembrando-nos da importância da responsabilidade individual e do trabalho em equipe para alcançar o sucesso em qualquer empreendimento. Assim como os marinheiros da frota britânica foram impulsionados por esse chamado à ação, também podemos aplicar essa mensagem em nossas próprias vidas e carreiras. Como cirurgiões, somos lembrados da nossa obrigação de desempenhar cada procedimento com diligência e dedicação, e ao mesmo tempo, liderar nossas equipes com empatia e coragem. A mensagem de Lord Nelson nos inspira a superar desafios, enfrentar pressões e trabalhar juntos para alcançar os melhores resultados possíveis em nossas práticas médicas. Ao seguir esse exemplo atemporal de liderança podemos oferecer o melhor atendimento possível aos nossos pacientes e à sociedade.
Ortodoxia Cirúrgica
Embora “Ortodoxia” seja uma obra filosófica e teológica escrita por G.K. Chesterton, suas ideias podem ter algumas aplicações interessantes e reflexivas no cotidiano da cirurgia. Claro que a relação direta pode não ser evidente, mas certos princípios filosóficos podem fornecer perspectivas valiosas para os cirurgiões. Aqui estão algumas maneiras pelas quais as ideias de “Ortodoxia” podem ser aplicadas no contexto cirúrgico:
- Valorizar o pensamento paradoxal: A cirurgia é uma disciplina complexa e muitas vezes ambígua, onde os médicos devem tomar decisões cruciais em situações desafiadoras. Valorizar o pensamento paradoxal pode ajudar os cirurgiões a considerar opções diversas e até opostas antes de tomar decisões importantes.
- Reconhecimento da complexidade humana: Chesterton destaca a importância de compreender a natureza complexa da realidade. No contexto cirúrgico, isso se traduz em tratar cada paciente como um indivíduo único, com suas próprias circunstâncias médicas, emocionais e sociais. Isso pode ajudar os cirurgiões a abordar cada caso com uma mente aberta e livre de preconceitos.
- Equilíbrio entre tradição e inovação: Assim como Chesterton valoriza a tradição cultural, os cirurgiões podem se beneficiar de uma abordagem equilibrada entre as técnicas tradicionais e as inovações médicas. Combinar o conhecimento estabelecido com as mais recentes pesquisas e tecnologias pode levar a melhores resultados para os pacientes.
- Enfrentar a incerteza: A cirurgia pode ser imprevisível, e os resultados nem sempre são garantidos. A ortodoxia de Chesterton nos encoraja a aceitar a incerteza e a enfrentar os desafios com coragem e confiança. Essa mentalidade pode nos ajudar a enfrentar situações complicadas e se adaptar a cenários imprevistos.
- Importância da ética e moralidade: Chesterton enfatiza a importância da moralidade e da virtude. Na cirurgia, esses princípios são essenciais para garantir a melhor qualidade de atendimento ao paciente, respeitando sempre a dignidade e os direitos humanos.
- Valorizar a imaginação: A imaginação é uma parte essencial do trabalho cirúrgico, permitindo aos médicos visualizar procedimentos, simular situações e pensar em soluções criativas. A capacidade de imaginar possibilidades pode ajudar os cirurgiões a planejar cuidadosamente cada intervenção.
Embora “Ortodoxia” não tenha sido escrito com o objetivo específico de se aplicar à cirurgia, as ideias e princípios contidos na obra podem inspirar uma reflexão mais profunda e nos guiar de forma mais consciente, sensível e equilibrada.
As virtudes cardinais cirúrgicas
A prática cirúrgica é uma forma de arte que exige habilidade técnica e precisão, mas vai além disso. Os cirurgiões não apenas dominam as técnicas e procedimentos, mas também são desafiados a aplicar virtudes cardinais em cada etapa do ato operatório. A diérese, exérese, hemostasia e síntese, as quatro fases cruciais da cirurgia, podem ser vistas como um reflexo das virtudes cardinais: prudência, justiça, fortaleza e temperança. Vamos explorar como essas virtudes se manifestam na rotina de um cirurgião comprometido com o bem-estar dos pacientes.
Diérese (A Prudência como Guia) : A primeira etapa da cirurgia, a diérese, é o momento em que o cirurgião realiza uma incisão precisa para acessar o local a ser tratado. A prudência, virtude da sabedoria prática, entra em cena através do domínio da anatomia. O cirurgião deve avaliar cuidadosamente cada caso, analisar os riscos e tomar decisões fundamentadas. A prudência orienta a escolha das melhores abordagens cirúrgicas, levando em consideração a saúde geral do paciente, suas necessidades individuais e o objetivo final da intervenção.
Exérese (A Justiça na Busca pelo Equilíbrio): Na fase de exérese, o cirurgião remove tecidos ou estruturas comprometidas pela doença. Aqui, a justiça desempenha um papel essencial. O cirurgião deve agir com equidade, buscando remover apenas o que é necessário, sem excessos ou negligências. A justiça implica em tratar cada paciente com equidade, respeito e imparcialidade, levando em consideração os melhores interesses do indivíduo e buscando o bem comum. É um compromisso em garantir que o procedimento cirúrgico seja realizado com integridade e sempre em benefício do paciente.
Hemostasia (A Fortaleza para Enfrentar Desafios) : Durante a fase de hemostasia, o cirurgião aplica técnicas para controlar o sangramento e garantir um campo cirúrgico claro. Nesse momento, a fortaleza se faz presente. A cirurgia pode apresentar situações imprevistas, complicações ou momentos de grande pressão. A fortaleza permite ao cirurgião manter-se firme, agir com coragem diante de adversidades e tomar decisões rápidas, mas sábias, para proteger a vida e o bem-estar do paciente. A fortaleza é a virtude que impulsiona o cirurgião a enfrentar desafios com firmeza e superar obstáculos através de uma alma inabalável, mantendo durante todo o procedimento uma determinação com o melhor prognóstico do paciente.
Síntese (A Temperança na Busca do Equilíbrio Final) : A última etapa, a síntese, envolve a restauração da integridade do tecido por meio de suturas ou outros meios. Nesse momento, a temperança se revela. A temperança é a virtude que permite ao cirurgião exercer controle e moderação, evitando excessos e buscando a harmonia. A escolha adequada do material de sutura, a técnica precisa e o cuidado meticuloso são fundamentais. A temperança assegura que a finalização do ato operatório seja feita com prudência, justiça e fortaleza, considerando o bem-estar a longo prazo do paciente.
Logo, podemos concluir que a prática da cirurgia transcende a habilidade técnica e exige o cultivo das virtudes cardinais. A prudência, a justiça, a fortaleza e a temperança tornam-se guias éticos para o cirurgião comprometido com o cuidado ao paciente. A diérese, exérese, hemostasia e síntese, cada uma refletindo uma virtude cardinal, são etapas cruciais em busca da excelência médica. Quando o cirurgião incorpora essas virtudes em sua rotina, ele se torna não apenas um técnico habilidoso, mas um verdadeiro médico que busca o bem-estar e a cura integral do paciente. A arte da cirurgia, assim, se revela não apenas como uma expressão de destreza manual, mas como uma expressão do cuidado compassivo e virtuoso que o médico oferece ao paciente.
Sobre o FUTURO
Aos cinco anos, o que você queria ser quando crescesse?
Médico.
Tudo começou quando eu tinha por volta de 4 – 5 anos e após um acidente domiciliar, precisei passar por uma cirurgia na mão. A forma como aquele profissional que nos atendeu acalmou a angústia dos meus pais e tratou com habilidade o ferimento me marcou profundamente. Apesar de não ter ideia do que isso significaria na minha jornada futura, aquele sentimento de ação e resolução se tornou uma paixão que me acompanha até hoje.

Specific Competence of Surgical Leadership
Surgeons are uniquely prepared to assume leadership roles because of their position in the operating room (OR). Whether they aspire to the title or not, each and every surgeon is a leader, at least within their surgical team. Their clinical responsibilities offer a rich variety of interpretations that prepare them for a broader role in health care leadership. They deal directly with patients and their families, both in and out of the hospital setting, seeing a perspective that traditional health care administrative leaders rarely experience. They work alongside other direct providers of health care, in varied settings, at night, on weekends, as well as during the typical workday. They understand supply-chain management as something more than lines on a spreadsheet.
The Challenges for a Surgical Leader
Surgeons prefer to lead, not to be led. Surgical training has traditionally emphasized independence, self-reliance, and a well-defined hierarchy as is required in the OR. However, this approach does not work well outside the OR doors. With colleagues, nurses, staff, and patients, they must develop a collaborative approach. Surgeons are entrusted with the responsibility of being the ultimate decision maker in the OR. While great qualities in a surgeon in the OR, it hinders their interactions with others. They have near-absolute authority in the OR, but struggle when switching to a persuasive style while in committees and participating in administrative activities. Most surgeons do not realize they are intimidating to their patients and staff. With patients, a surgeon needs to be empathetic and a good listener. A surgeon needs to slow the pace of the discussion so that the patient can understand and accept the information they are receiving. As perfectionists, surgeons demand a high level of performance of themselves. This sets them up for exhaustion and burnout, becoming actively disengaged, going through the motions, but empty on the inside. Given the many challenges surgeons face, it is difficult for them to understand the leadership role, given its complex demands.
Specific Competencies
Authority
Although teams and all team members provide health care should be allowed input, the team leader makes decisions. The leader must accept the responsibility of making decisions in the presence of all situations. They will have to deal with conflicting opinions and advice from their team, yet they must accept that they will be held accountable for the performance of their team. The surgeon–leader cannot take credit for successes while blaming failures on the team. Good teamwork and excellent communication do not relieve the leader of this responsibility.
Leadership Style
A surgeon often has a position of authority based on their titles or status in an organization that allows them to direct the actions of others. Leadership by this sort of mandate is termed “transactional leadership” and can be successful in accomplishing specific tasks. For example, a surgeon with transactional leadership skills can successfully lead a surgical team through an operation by requesting information and issuing directives. However, a leader will never win the hearts of the team in that manner. The team will not be committed and follow through unless they are empowered and feel they are truly heard. A transformational leader is one who inspires each team member to excel and to take action that supports the entire group. If the leader is successful in creating a genuine atmosphere of cooperation, less time will be spent giving orders and dealing with undercurrents of negativity. This atmosphere can be encouraged by taking the time to listen and understand the history behind its discussion. Blame should be avoided. This will allow the leader to understand the way an individual thinks and the group processes information to facilitate the introduction of change. While leadership style does not guarantee results, the leader’s style sets the stage for a great performance. At the same time, they should be genuine and transparent. This invites the team members to participate, creating an emotional connection. Leaders try to foster an environment where options are sought that meet everyone’s desires.
Conflict Management
Conflict is pervasive, even in healthy, well-run organizations and is not inherently bad. Whether conflict binds an organization together or divides it into factions depends on whether it is constructive or destructive. A good leader needs to know that there are four essential truths about conflict. It is inevitable, it involves costs and risks, the strategies we develop to deal with the conflict can be more damaging than the conflict itself, and conflict can be permanent if not addressed. The leader must recognize the type of conflict that exists and deal with the conflict appropriately. Constructive discussion and debate can result in better decision making by forcing the leader to consider other ideas and perspectives. This dialog is especially helpful when the leader respects the knowledge and opinions of team members with education, experience, and perspective different from the leader’s. Honesty, respect, transparency, communication, and flexibility are all elements that a leader can use to foster cohesion while promoting individual opinion. The leader can create an environment that allows creative thinking, mutual problem solving, and negotiation. These are the hallmarks of a productive conflict. Conflict is viewed as an opportunity, instead of something to be avoided.
Communication Skills
Communication is the primary tool of a successful leader. On important topics, it is incumbent on the leader to be articulate, clear, and compelling. Their influence, power, and credibility come from their ability to communicate. Research has identified the primary skills of an effective communicator. They are set out in the LARSQ model: Listening, Awareness of Emotions, Reframing, Summarizing, and Questions. These are not set in a particular order, but rather should move among each other freely. In a significant or critical conversation, it is important for a leader to listen on multiple levels. The message, body language, and tone of voice all convey meaning. You cannot interrupt or over-talk the other side. They need an opportunity to get their entire message out. Two techniques that enhance listening include pausing and the echo statement. Pausing before speaking allows the other conversant time to process what they have said to make sure the statement is complete and accurate. Echo statements reflect that you have heard what has been said and focuses on a particular aspect needing clarification. Good listening skills assure that the leader can get feedback that is necessary for success.
Vision, Strategy, Tactics, and Goals
One of the major tasks of a leader is to provide a compelling vision, an overarching idea. Vision gives people a sense of belonging. It provides them with a professional identity, attracts commitment, and produces an emotional investment. A leader implements vision by developing strategy that focuses on specific outcomes that move the organization in the direction of the vision. Strategy begins with sorting through the available choices and prioritizing resources. Through clarification, it is possible to set direction. Deficits will become apparent and a leader will want to find new solutions to compensate for those shortfalls. For example, the vision of a hospital is to become a world class health care delivery system. Strategies might include expanding facilities, improving patient satisfaction, giving the highest quality of care, shortening length of hospital stay with minimal readmissions, decreased mortality, and a reduction in the overall costs of health care. Tactics are specific behaviors that support the strategy with the aim to achieve success. Tactics for improving patient satisfaction may include reduced waiting time, spending more time with patients, taking time to communicate in a manner that the patient understands, responding faster to patient calls, etc. These tactics will then allow a leader to develop quantitative goals. Patient satisfaction can be measured. The surgical leader can then construct goals around each tactic, such as increasing satisfaction in specific areas. This information allows a surgical leader to identify barriers and they can take steps to remedy problem areas. This analysis helps a leader find the weakest links in their strategies as they continue toward achieving the vision.
Change Management
The world of health care is in continuous change. The intense rate of political, technical, and administrative change may outpace an individual’s and institution’s ability to adapt. Twenty-first century health care leaders face contradictory demands. They must navigate between competing forces. Leaders must traverse a track record of success with the ability to admit error. They also must maintain visionary ideas with pragmatic results. Individual accountability should be encouraged, while at the same time facilitating teamwork. Most leaders do not understand the change process. There are practical and psychological aspects to change. From an institutional perspective, we know that when 5% of the group begins to change, it affects the entire group. When 20% of a group embraces change, the change is unstoppable.
Succession Planning and Continuous Learning
An often-overlooked area of leadership is planning for human capital movement. As health care professionals retire, take leaves of absences, and move locations, turmoil can erupt in the vacuum. Leaders should regularly be engaging in activities to foster a seamless passing of institutional knowledge to the next generation. They also should seek to maintain continuity to the organization. Ways to accomplish this include senior leaders actively exposing younger colleagues to critical decisions, problem solving, increased authority, and change management. Leaders should identify promising future leaders, give early feedback for areas of improvement, and direct them toward available upward career tracks. Mentoring and coaching help prepare the younger colleagues for the challenges the institution is facing. Teaching success at all levels of leadership helps create sustainable high performance.
Visão Crítica de Segurança (Colecistectomia)
A colecistectomia laparoscópica (CL) é o padrão-ouro para tratamento de cálculos biliares. No entanto, o risco de lesão do ducto biliar (BDI) continua a ser preocupação significativa, uma vez que CL ainda tem taxa de BDI maior do que a via laparotômica, apesar de muitos esforços propostos para aumentar sua segurança.
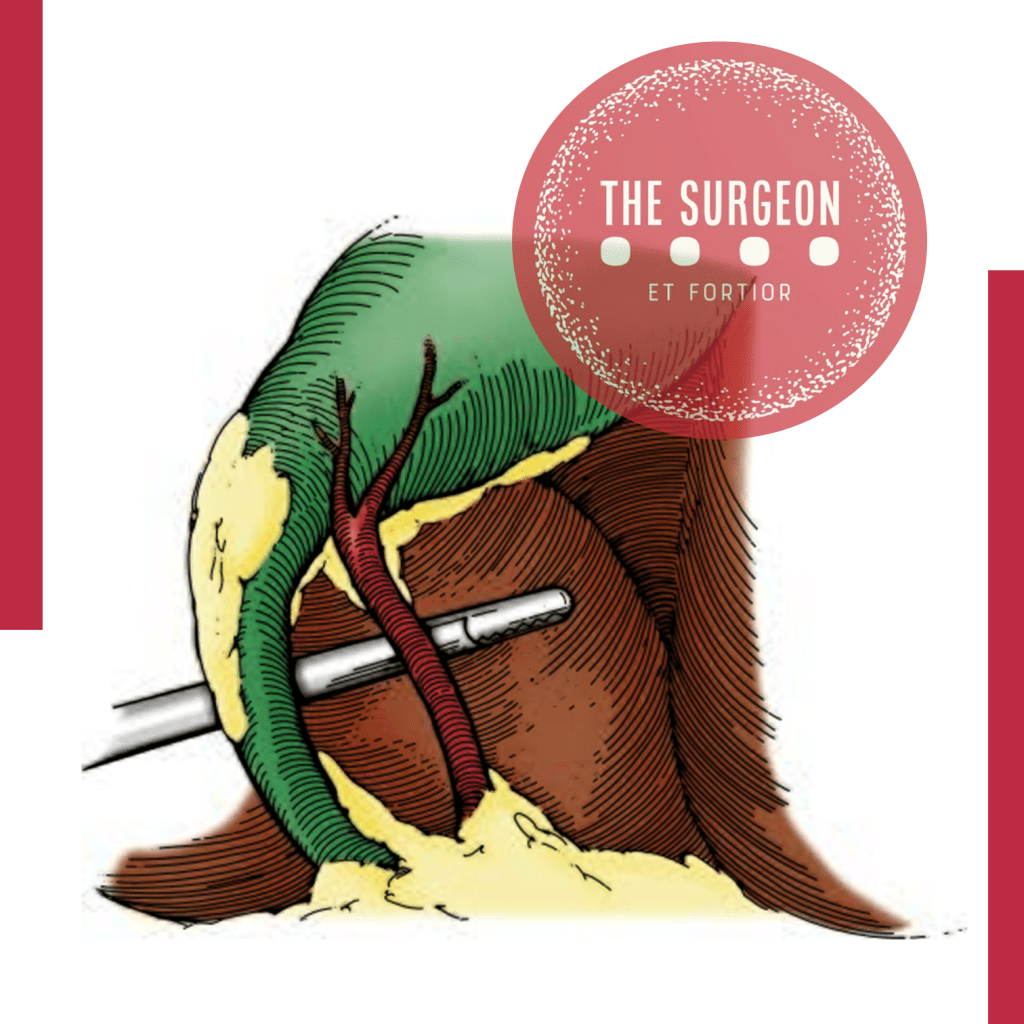
A Visão Crítica da Segurança (CVS) proposta por Strasberg é a técnica para a identificação dos elementos críticos do triângulo de Calot durante a CL. Esta técnica foi adotada em vários programas de ensino e com a proposta de reduzir o risco de BDI e o uso da adequado da CVS está associado a menores taxas de BDI. O objetivo deste #Webinar é abordar a Anatomia Cirúrgica Fundamental para a realização de uma Colecistectomia Laparoscópica.
Subtotal cholecystectomy for difficult acute cholecystitis
Laparoscopic cholecystectomy is considered the gold standard for treatment of benign gallbladder diseases. Cholecystectomy using this method can be completed in 90% of elective cholecystectomies and 70% of emergency cholecystectomies. Acute cholecystitis, especially if difficult, can change the above paradigm, resulting in open conversion or change of technique. The conditions that define a difficult cholecystectomy are as follows: necessity of conversion from laparoscopic to open surgery; duration of procedure greater than 180 min; blood loss greater than 300 ml; and urgent need for involvement of a more experienced surgeon. One of the “rescue” procedures to complete the surgery safely (both for the surgeons and patients) is subtotal cholecystectomy (STC). Open and laparoscopic subtotal cholecystectomy have been reported. For many surgeons, this is considered a bail out technique, and the timing of decision making is crucial to avoid catastrophic complications. Te capability to perform STC in laparoscopy is increasingly requested during difficult laparoscopic cholecystectomy. Difficult LC has a risk of BDI from 3 to 5 times higher in laparoscopy than open surgery. In case of operative difficulties of young surgeons mostly trained in laparoscopy the help of senior surgeons is strongly recommended. The purpose of the present study is to clarify how laparoscopic subtotal cholecystectomy may be used to complete a difficult cholecystectomy for acute cholecystitis without serious complications.
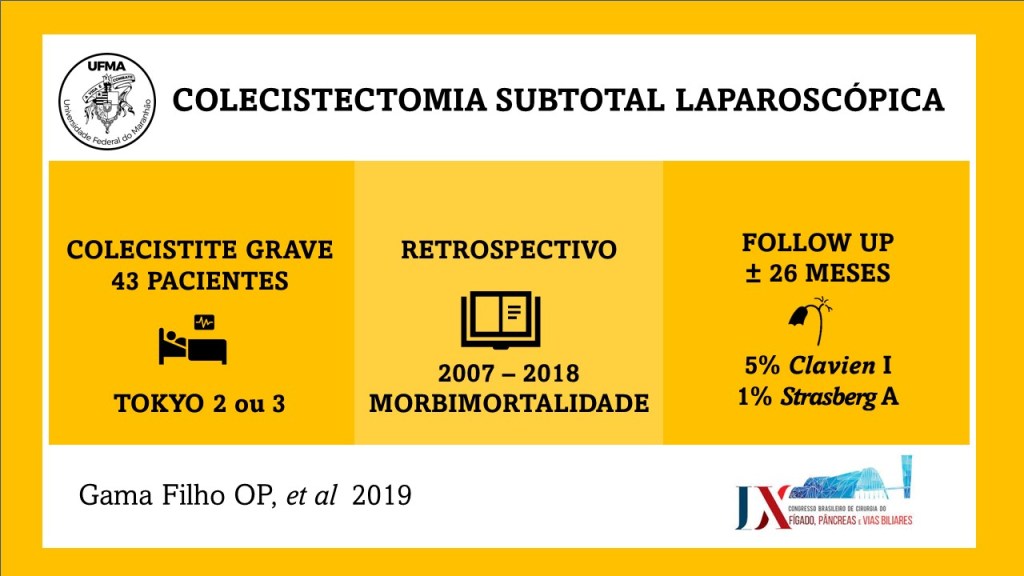
Biliary leakage represents the most frequent complication of incomplete resection of the gallbladder wall in cases of difficult acute cholecystectomy treated with subtotal cholecystectomy. This complication is rarely fatal but requires correct treatment. If bile leakage does not stop spontaneously seven days postoperatively, the possible treatments are endoscopic biliary sphincterotomy, endoscopic plastic stent, and a fully covered self-expanding metal stent. When performing closure of the gallbladder stump, suturing the anterior residual of both anterior and posterior wall represents the best method to have fewer complications. Complications, if not lethal, decrease the patient’s quality of life. Intraoperatively, it is of utmost importance to carefully expose the gallbladder stump to avoid left-in-place stones, wash the entire cavity and drain the abdomen. Bile duct injuries can be a significant complication in this type of surgery. Prevention of the lesions with conversion from laparoscopic to open, or the opinion of older surgeon in case of difficulties is strongly recommended. Mortality is a very rare complication. The limitations of our study are given by the heterogeneity of the techniques used for LSC and the lack of a long-term follow-up analyzing the related complications.
Liver Disease and Perioperative Risk
The liver is the biggest intestinal organ and plays a central role in the homeostasis of different physiological systems including nutrition and drug metabolism, the synthesis of plasma proteins and haemostatic factors, as well as the elimination of different endogenous and exogenous substances. Although the liver contributes with only 3% to total body weight, given its major role in homeostasis and high energy consumption, it receives 25% of total cardiac output (CO). Two vessels contribute to the perfusion of the liver. The majority (70%) of the hepatic perfusion is provided by the portal vein, which contributes 50% of the organ’s oxygen demand. The other 50% is provided by the hepatic artery, which makes up around 30% of total liver perfusion. Hepatic arterial blood flow is mainly dependent on the organ’s metabolic demands and controlled via autoregulatory mechanisms, whereas blood supply through the portal vein depends on the perfusion throughout the whole gastrointestinal tract and the spleen. This unique, dual perfusion system provides constant perfusion rates and oxygen supply, which is crucial for adequate liver function. These high oxygen demands are reflected in a hepatic vein saturation of almost 30%.
The liver is also unique in its ability of regeneration, which allows the performance of major surgery including, amongst others, extended resections of liver tumours, living donations and so on. Many patients have normal liver function parameters when they present for liver surgery, especially when the reason for resection is metastasis or a benign liver tumour. The most common causes of liver resections are the hepatocellular carcinoma (HCC) and the cholangiocellular carcinoma (CCC). Hepatocellular carcinoma (HCC) often develops in patients with underlying liver cirrhosis; many of these patients show signs of chronic liver dysfunction (CLD).
As explained previously, the liver plays a central role in a great deal of physiological systems. Therefore, in case of chronic liver dysfunction (CLD) or liver failure, several effects on other organ systems have to be expected. Consequently liver resections and bile duct surgery as having a high risk for perioperative cardiac events, with an estimated 30-day cardiac event rate (cardiac death and myocardial infarction) of more than 5%. Patients undergoing liver surgery pose a significant challenge to treating physicians in the perioperative period. Due to the improvement of surgical techniques, the “liver patient” is becoming more and more complex, confronting surgeons, anaesthetists and intensive care personnel with difficult intra- and postoperative courses, and considerable multiorgan disorders. The cornerstones of an optimal management are careful selection of the patients, appropriate monitoring and protection of the liver and other vital organs.
“Not Only SURGEONS…”
SURGERY, A NOBLE PROFESSION
Surgery is, indeed, one of the noblest of professions. Here is how Dictionary defines the word noble: 1) possessing outstanding qualities such as eminence, dignity; 2) having power of transmitting by inheritance; 3) indicating superiority or commanding excellence of mind, character, or high ideals or morals. These three attributes befit the profession of surgery. Over centuries, the surgical profession has set the standards of ethical and humane practice. Surgeons have made magnificent contributions in education, clinical care, and science. Their landmark accomplishments in surgical science and innovations in operative technique have revolutionized surgical care, saved countless lives, and significantly improved longevity and the quality of human life. Generations of surgeons have developed their craft and passed it on to succeeding generations, as they have to me and to each one of you, to take into the future.
Beyond its scientific and technical contributions, surgery is uniquely fulfilling as a profession. It has disciplined itself over the centuries and dedicated its practice to the best welfare of all human beings. In return, it has been accorded the respect of society, of other professions, and of policy makers. Its conservative stance has served it well and has been the reason for its constancy and consistency. At the beginning of the 21st century, however, profound changes are taking place at all levels and at a dizzying pace, providing both challenges and opportunities to the surgical profession. These changes are occurring on a global level, on the national level, in science and technology, in healthcare, and in surgical education and practice.
To retain its leadership position in innovation and its attractiveness as a career choice for students, surgery must evolve with the times. It is my belief that surgery needs to introduce changes to create new priorities in clinical practice, education, and research; to increase the morale and prestige of surgeons; and to preserve general surgery as a profession. I am reminded of a Chinese aphorism that says, “You cannot prevent the birds of unhappiness from flying over your head, but you can prevent them from building a nest in your hair.”
ADVANCES IN SCIENCE
The coalescence of major advances in science and technology made the end of the 20th century unique in human history. Notable among the achievements are the development of microchips and miniaturization, which fueled the explosion in information technology. The structure of the human genome is nearly completely elucidated, ushering in the genomic era in which genetic information will be used to predict, on an individual basis, susceptibility to disease and responsiveness to drug therapy. The field of nanotechnology allows scientists to work at a resolution of less than one nanometer, the size of the atom. By comparison, the DNA molecule is 2.5 nanometers.
In the last 50 years, biomedical research became increasingly reductionist, turning physiologists and anatomists into molecular biologists. As a result, two basic science fields—integrative physiology and gross anatomy—now have a lower standing in medical education and surgical science than they once did. Surgery and surgical departments can and possibly should claim these fields, but the window of opportunity is narrow. Research is now moving back from discipline-based reductionist science to multidisciplinary science of complexity, in which biomedical scientists work side by side with engineers, mathematicians, and bioinformatists. The ability of high-speed computers to quickly process tens of millions of pieces of data now allows for data-driven rather than hypothesis-based research. This collaboration among different disciplines has already been successful.
TRANSFORMATION OF HEALTHCARE SYSTEM
During the past 75 years, we have seen the entire healthcare system undergo a profound transformation. In the 1930s and for a considerable period thereafter, medical practice was fee-for-service, the doctor–patient relationship was strong, and the physician perceived himself or herself as being responsible nearly exclusively to his or her individual patients. The texture of medical practice started to change when the federal government became involved in the provision of healthcare in 1965. The committee on “Crossing the Quality Chasm” identified six key attributes of the 21st-century healthcare system. It must be:
- Safe, avoiding injuries to patients;
- Effective, providing services based on scientific knowledge;
- Patient-oriented, respectful of and responsive to individual patients’ needs, values, and preferences;
- Timely, reducing waits, eliminating harmful delays for both care receiver and caregiver;
- Efficient, avoiding wasted equipment, supplies, ideas, and energy;
- Equitable, providing equal care across genders, ethnicities, geographic locations, and socioeconomic strata;
No one knows at present what this 21st-century healthcare system will look like. While care in the old system was reactive, in the new system it will be proactive. The “find it, fix it” approach of the old system will be replaced by a “predict it, prevent it, and if you cannot prevent it, fix it” approach. Sporadic intervention, provided only when patients present with illness, will give way to a system in which physicians and other healthcare providers plan 1-, 5-, and 10-year care programs for each patient. Care will be more interactive, with patients taking a more important role in their own care. The technology-oriented system will become a system that provides graded intervention. Delivery systems will not be fractionated but integrated. Even more importantly, care will not be based simply on experience and clinical impression but on evidence of proven outcome measures. If the old system was cost-insensitive, the new system will be cost-sensitive.
SURGICAL PRACTICE
There are many reasons for the declining interest in general surgery, some of which parallel reasons for the drop in medical school applicants in general. One problem specific to surgery is that medical students are given less and less exposure to surgery, due to the shortening of required surgical rotations. Most important, however, is their perception that the life of the surgical resident is stressful, the work hours too long, and the time for personal and family needs inadequate. The workload of the surgical resident over the years has increased significantly both in amount and intensity, without concomitant increase in the number of residents and at a time when hospitals have significantly reduced the support personnel on the surgical ward and in the operating rooms. Students graduating with debts close to $100,000 simply find the years of training in surgery too long, followed by uncertain practice income after graduation.
From several recent studies, lifestyle is the critical and most pressing issue in surgical residency. Some studies have also shown that the best students tend to select specialties that provide controllable lifestyles, such as radiology, dermatology, and ophthalmology. We have a problem not only in the declining number of students applying for surgical training but also in the declining quality of those who do apply. In a preliminary survey of 153 responding general surgery programs, we found that attrition (i.e., categorical residents leaving the training programs) occurred at a rate of 13% to 19% in the last 5 years. In 2001, 46% of those leaving general surgery training programs cited lifestyle as the major reason.
Unless these trends are reversed, general surgery as a specialty is threatened, and a future shortage of general surgeons is inevitable. I know that the Council of the American Surgical Association is most concerned about the crisis in general surgery. We must do a better job of communicating to students and residents that the practice of surgery is as rewarding as ever and full of opportunities in this new era. Innovations in minimal access and computer-assisted surgery and simulation technology provide exciting new possibilities in surgical training. We must also look very carefully at the demands of surgical residency and improve the life of residents without compromising their surgical experience. Unless we deal with work hours and quality of life issues, we are likely to see continuing decline in the interest of medical students in surgical training.
CONCLUSIONS
In conclusion, the noble profession of surgery must rise to meet numerous challenges as the world in which it operates continues to undergo profound change. These challenges represent opportunities for the profession to develop an international perspective and a global outreach and to address the growing needs of an aging population undergoing major demographic and workforce shifts. The leadership of American surgery has a unique role to play in the formulation of a new healthcare system for the 21st century. This task will require commitment to quality of care and patient safety, and it will depend on harnessing the trust and support of the American public. Advances in science and technology—particularly in minimal access surgery, robotics, and simulation technology—provide unprecedented opportunity for surgeons to continue to make landmark contributions that will improve surgical care and the human condition. I believe it is also crucially important that we train surgeon-scientists who will keep surgery at the cutting edge in the genomic and bioinformatics era. Ours is a noble profession imbued with eminence, dignity, high ideals, and ethical values. It has a rich and proud heritage… and I quote, “The highest intellects, like the tops of mountains, are the first to catch and reflect the dawn.”
Source: Lecture from Haile T. Debas, MD (UCSF School of Medicine, San Francisco, California) Presented at the 122nd Annual Meeting of the American Surgical Association, April 25, 2002, The Homestead, Hot Springs, Virginia.
Surgical Management of PANCREATIC CANCER
INTRODUCTION
Pancreatic ductal adenocarcinoma (PDAC) carries one of the poorest overall prognosis of all human malignancies. The 5-year survival in patients with PDAC, for all stages, remains as low as 6–7%. The low survival rate is attributed to several factors, of which the two most important are aggressive tumor biology and late stage at which most patients are diagnosed. Only 10–20% of patients are eligible for resection at presentation, 30–40% are unresectable/locally advanced, and 50–60% are metastatic. Pancreatic cancer without distant metastasis can be divided into three categories: resectable, borderline resectable, and locally advanced. In absence of metastatic disease, the most important factor for improving survival and possibly offer cure is to achieve a margin-negative resection. Even after potential curative resection, most patients develop recurrences eventually, and 5-year survival of completely resected patients is only up to 25%. The aggressive tumor biology and its inherent resistance to chemotherapy and radiotherapy contributes to early recurrence and metastasis.
SURGICAL ADVANCES
Pancreatic cancer surgery has evolved over the past few decades and remains the cornerstone of treatment of resectable and borderline resectable tumors. Advances in modern imaging give precise information on disease extension and vascular involvement that aids in surgical planning in order to achieve a margin-negative resection.
SURGICAL TECHNIQUES
Surgical techniques for pancreatic cancer include pancreaticoduodenectomy, distal pancreatectomy with splenectomy, and total pancreatectomy. Standard lymphadenectomy for pancreatoduodenectomy should include removal of lymph node stations 5, 6, 8a, 12b1, 12b2, 12c, 13a, 13b, 14a, 14b, 17a, and 17b. Involvement of superior mesenteric vein (SMV)/portal vein(PV) was previously considered as a contraindication for resection. However, curative resection along with SMV/PV with vascular reconstruction has now become a standard practice in specialized high-volume centers. To improve margin-negative resections, specially in borderline resectable tumors with proximity to vascular structures, SMA first approach was proposed as a new modification of standard pancreatico-duodenectomy. In a systematic review, SMA first approach was shown to be associated with better perioperative outcomes, such as blood loss, transfusion requirements, pancreatic fistula, delayed gastric emptying, and reduced local and metastatic recurrence rates. In case of arterial involvement, there is no good evidence at present to justify arterial resections for right-sided pancreatic tumors. However, the modified Appleby procedure, which includes en bloc removal of celiac axis with or without arterial reconstruction, when used in appropriately selected patients, offers margin negative resection with survival benefit for locally advanced pancreatic body and tail tumors and should be performed in high-volume centers. Most evidence does not support advantage of more extended resections such as removal of the para-aortic lymph nodes and nerve plexus and multivisceral resections routinely. Such extended resections are associated with compromised quality of life because of associated higher perioperative morbidity and intractable diarrhea. However, in highly selected patients, with preserved performance status and stable or nonprogressive disease on neoadjuvant treatment, such extended resections can provide survival advantage over palliative treatments. Radical surgery in the presence of oligometastatic disease has also been reported to prolong survival in highly selected patients.
Surgical Management of CHOLANGIOCARCINOMA
Cholangiocarcinoma is an uncommon cancer that occurs within the intrahepatic and extrahepatic portions of the bile duct system. In North America, the incidence of extrahepatic cholangiocarcinoma is 0.5–2 per 100,000 and 0.95 per 100,000 for intrahepatic cholangiocarcinoma. Up to 50% of patients will be lymph node (LN) positive at presentation, 5% are multifocal tumors, and 10–20% will have peritoneal involvement at presentation. Risk factors for cholangiocarcinoma are primary sclerosing cholangitis (PSC) with a lifetime risk 10–40%, parasitic infection, previous sphincteroplasty, congenital anomalies of the biliary tree (choledochal cyst, Caroli’s disease, anomalous pancreaticobiliary duct junction), and chronic biliary inflammatory disease (hepatitis B/C, liver cirrhosis, recurrent pyogenic cholangitis). The most common presentation is painless jaundice and weight loss in the setting of extrahepatic duct involvement. In Western countries, 80% are extrahepatic (20% distal and 60% hilar) and 20% are intrahepatic.
SPECIAL NOTES
Click here and share on TWITTER
• Ca 19–9 can be elevated in up to 85% of patients with cholangiocarcinoma, but is not specific; elevation can also occur in the setting of obstructive jaundice without malignancy. If it remains elevated after biliary decompression, it could indicate the presence of malignancy. Elevated pre- and postoperative Ca 19–9 predict poor survival.
• For perihilar tumors, decisions regarding which side of the liver to resect depend on right- or left-sided dominance, volume of future liver remnant, and the extent of vascular and ductal involvement.
• Some centers report that 30–50% of tumors will be deemed unresectable at the time of surgery, despite accurate preoperative imaging.
• Quality Indicators: Pathologic Analysis—R0 margin, regional lymphadenectomy includes three or more LN.
SURGICAL MANAGEMENT
Intrahepatic cholangiocarcinoma: Surgical resection is the only potential cure with removal of involved liver segments. There is emerging evidence that recommends a routine hilar LN and dissection for its prognostic value, M1 disease includes involvement of celiac,periaortic or caval LN.
Distal bile duct (below the cystic duct): Surgical resection is the only potential cure. Pancreaticoduodenectomy including en bloc resection of extrahepatic bile duct and gallbladder. Regional nodes include: Hilar (CBD, common hepatic, portal, cystic), Posterior and anterior pancreaticoduodenal Nodes along SMV, Nodes along right and lateral wall of SMA.
Hilar (above the cystic duct): En bloc resection of extrahepatic bile duct and gallbladder, including right and left hepatectomy, or extended right/left hepatectomy, Caudate lobe should be removed. Regional nodes include: Hilar (CBD, hepatic,portal, cystic), Pericholedochal nodes in hepatoduodenal ligament.
PhD THESIS (Ozimo Gama, MD)
COMPARATIVE STUDY BETWEEN THE SLEEVE GASTRECTOMY AND GASTRIC PLICATION IN OBESE RATS
INTRODUCTION: Obesity results from a prolonged imbalance between energy intake and energy expenditure. Studies with experimental models of bariatric surgery provided a fundamental contribution to the understanding of morphological and functional changes in obesity and after bariatric surgery. The restrictive bariatric surgery techniques currently used are gastric banding, sleeve gastrectomy and the gastric plication. The latter is considered an experimental technique and has therefore not yet enough studies that shed light on the postoperative rates of weight loss, surgical complications, resolution of comorbidities and the mechanisms responsible for weight loss. The aim of this study was to conduct a comparative study in rats with cafeteria diet-induced, between gastric plication and sleeve gastrectomy in variation late postoperative in body weight ,plasma biochemistry and gross and microscopic alterations gastric effects obesity.
MATERIAL AND METHOD: 28 male Wistar rats were randomized into three groups after induction period of obesity by cafeteria diet and underwent sleeve gastrectomy (GV group), gastric plication (GP group) and sham operation (control group). The animals were assessed daily postoperatively and the variables were recorded: (initial seven days, 14 and 21 days) body weight and presence of complications until day 21 postoperatively, when they were euthanized and evaluated: biochemistry (glucose, insulin, HDL, total cholesterol, triglycerides, AST, ALT and serum ghrelin), degree of intra-abdominal adhesions, resistance testing will air insufflation in the stomach and microscopic evaluation of the gastric mucosa.

RESULTS: In relation to body weight variation of animals GV group (initial weight: 318 ± 7.89 g / Final weight: 213 ± 9.03g) was significantly decreased (p<0.05) at 21 post-surgery day compared to the GP group (initial weight: 314.11 ± 20.79 g / final weight: 239.16 ± 14.71 g) and control (initial weight: 315.16±17.54g / final weight: 317.91±16.06 g). The animals in the GV group had a significant decrease (p<0.001) in blood glucose, insulin, transaminases, serum HDL and ghrelin compared to animals in GP and control. Was also significantly lower the burst pressure of the stomach in the GV group, the insufflation test the atmospheric air in relation to the GP and control groups. The GP and GV groups showed even different histological grade of inflammation
(subacute inflammation) and control group (chronic inflammation).
CONCLUSIONS: The sleeve gastrectomy is more effective than gastric plication weight loss, metabolic control and reduction of serum ghrelin in obesity rats, and presents the same rates of postoperative complications (adhesions, deaths and grade inflammation).
KEYWORDS: 1. Obesity; 2. Bariatric Surgery; 3.Wistar rats.
Preoperative Biliary Drainage
The most common presenting sign for patients with malignancy of the periampullary region is obstructive jaundice. While a significant proportion of these patients will be asymptomatic, the deleterious systemic consequences of uncontrolled hyperbilirubinemia may still occur. Furthermore, symptoms such as pruritus can be debilitating and have a significant impact on the quality of life. Thus, some have advocated preoperative drainage of the biliary system in patients with resectable periampullary malignancies, given widespread availability of endoscopic retrograde cholangiopancreatography and its perceived safety profile. On the other hand, the purported benefits of routine preoperative drainage in this patient population (namely, resolution of symptoms in symptomatic patients while awaiting surgery, restoration of the enterohepatic cycle, and a potential decrease in postoperative morbidity) have proven to be largely theoretical, and now there are high-quality phase III data that demonstrate the deleterious effects of routine stenting. A seminal study originating from the Netherlands in 2010 evaluated this issue in the only modern randomized controlled trial to date evaluating preoperative endoscopic biliary decompression for these patients. In their multicenter study, they randomized 202 patients with newly diagnosed pancreatic head cancer and bilirubin levels between 2.3 and 14.6 mg/dL to preoperative biliary drainage for 4–6 weeks vs. immediate surgery which was to be performed within a week of enrollment. The primary endpoint was the development of serious complications within 120 days after randomization. Serious complications were defined as complications related to the drainage procedure or the surgical intervention that required additional medical, endoscopic, or surgical management, and that resulted in prolongation of the hospital stay, readmission to the hospital, or death. The reported overall rate of serious complications in this study favored the immediate surgery group (39 vs. 74%; RR 0.54–95% [CI], 0.41–0.71; P < 0.001), complications related to surgery were equivalent (37 vs. 47%; P = 0.14), and there was no difference in mortality rates or length of hospital stay. The observed drainage-related complications included a 15% rate of stent occlusion, 30% need for exchange, and 26% incidence of cholangitis.
“Based on these results, the authors concluded that the morbidity associated with the drainage procedure itself had an additive effect on the postoperative morbidity of patients undergoing pancreatic head resection for cancer and recommended against its routine use in this population.“
A Cochrane systematic review of all available randomized studies (including the abovementioned study by van der Gaag et al.) evaluating preoperative biliary drainage was published in 2012. In this study, Fang et al. assessed the impact of this intervention on survival, serious morbidity (defined as Clavien-Dindo grade 3 or 4), and quality of life. Furthermore, they sought to assess differences in total length of hospital stay and cost. They identified six randomized trials of which four used percutaneous transhepatic biliary drainage and the remaining two used endoscopic sphincterotomy and stenting. The pooled analysis of 520 patients (of which 51% underwent preoperative biliary drainage) showed no difference in mortality, but importantly, it showed a significantly higher incidence of serious morbidity in the preoperative drainage group with a rate ratio (RaR) of 1.66 (95% CI 1.28–2.16;P = 0.002). There was no difference in length of hospital stay and not enough data reported for analysis of cost or quality of life.
“Based on the available level 1 data, the authors concluded that there was no evidence to support or refute routine preoperative biliary drainage in patients with obstructive jaundice.“
However, this review also underscored the fact that preoperative biliary drainage may be associated with an increased rate of adverse events and thus questioned the safety of this practice. This Cochrane review included old studies that evaluated patients undergoing percutaneous drainage, a technique used less frequently today for periampullary malignancies. Furthermore, several of these trials included patients with hilar and other types of biliary obstruction. However, the concept of preoperative decompression, as well as its purported benefits and observed results, may be reasonably extrapolated to patients with periampullary lesions.
Critical View Of Safety
“The concept of the critical view was described in 1992 but the term CVS was introduced in 1995 in an analytical review of the emerging problem of biliary injury in laparoscopic cholecystectomy. CVS was conceived not as a way to do laparoscopic cholecystectomy but as a way to avoid biliary injury. To achieve this, what was needed was a secure method of identifying the two tubular structures that are divided in a cholecystectomy, i.e., the cystic duct and the cystic artery. CVS is an adoption of a technique of secure identification in open cholecystectomy in which both cystic structures are putatively identified after which the gallbladder is taken off the cystic plate so that it is hanging free and just attached by the two cystic structures. In laparoscopic surgery complete separation of the body of the gallbladder from the cystic plate makes clipping of the cystic structures difficult so for laparoscopy the requirement was that only the lower part of the gallbladder (about one-third) had to be separated from the cystic plate. The other two requirements are that the hepatocystic triangle is cleared of fat and fibrous tissue and that there are two and only two structures attached to the gallbladder and the latter requirements were the same as in the open technique. Not until all three elements of CVS are attained may the cystic structures be clipped and divided. Intraoperatively CVS should be confirmed in a “time-out” in which the 3 elements of CVS are demonstrated. Note again that CVS is not a method of dissection but a method of target identification akin to concepts used in safe hunting procedures. Several years after the CVS was introduced there did not seem to be a lessening of biliary injuries.
Operative notes of biliary injuries were collected and studied in an attempt to determine if CVS was failing to prevent injury. We found that the method of target identification that was failing was not CVS but the infundibular technique in which the cystic duct is identified by exposing the funnel shape where the infundibulum of the gallbladder joins the cystic duct. This seemed to occur most frequently under conditions of severe acute or chronic inflammation. Inflammatory fusion and contraction may cause juxtaposition or adherence of the common hepatic duct to the side of the gallbladder. When the infundibular technique of identification is used under these conditions a compelling visual deception that the common bile duct is the cystic duct may occur. CVS is much less susceptible to this deception because more exposure is needed to achieve CVS, and either the CVS is attained, by which time the anatomic situation is clarified, or operative conditions prevent attainment of CVS and one of several important “bail-out” strategies is used thus avoiding bile duct injury.
CVS must be considered as part of an overall schema of a culture of safety in cholecystectomy. When CVS cannot be attained there are several bailout strategies such a cholecystostomy or in the case of very severe inflammation discontinuation of the procedure and referral to a tertiary center for care. The most satisfactory bailout procedure is subtotal cholecystectomy of which there are two kinds. Subtotal fenestrating cholecystectomy removes the free wall of the gallbladder and ablates the mucosa but does not close the gallbladder remnant. Subtotal reconstituting cholecystectomy closes the gallbladder making a new smaller gallbladder. Such a gallbladder remnant is undesirable since it may become the site of new gallstone formation and recurrent symptoms . Both types may be done laparoscopically.”
Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 1995;180:101-25.
Mirizzi’s Syndrome
INTRODUCTION
First described by Pablo Mirizzi in 1948 as “functional hepatic syndrome”, Mirizzi’s syndrome was initially thought to be the result of a “physiologic sphincter” of the hepatic duct. It is now understood to be a result of mechanical obstruction of the common hepatic duct secondary to an impacted stone in the gallbladder neck, Hartmann’s pouch, or the cystic duct. The syndrome is very uncommon in Western populations with a reported prevalence of 0.05%-5.7% in large modern series of patients undergoing biliary surgery. With chronic stone impaction, inflammation and recurrent cholangitis can develop with subsequent erosion into the common bile duct (CBD) and resultant biliobiliary fistula between the gallbladder and CBD.
CLASSIFICATION
The syndrome encompasses a spectrum of disease. Broadly speaking, Mirizzi’s syndrome can be grouped into two major categories: (1) external compression of the CBD without a fistula (Type 1), and (2) erosion into the CBD causing a cholecystobiliary fistula (Type II-IV). Csendes classification is currently being used to reflect the above classification. Retrospective studies have identified an association between Mirizzi’s syndrome and gallbladder cancer, with an incidence as high as 28%, relative to an incidence of 1-2% in patients with uncomplicated gallstone disease. As with other malignant processes of the biliary tract, biliary stasis and chronic inflammation have been suggested to play a role. In general, it is difficult to distinguish benign Mirizzi’s syndrome from a neoplastic process preoperatively, although older patient age, significantly elevated Ca 19-9, and imaging features suggestive of invasion into the liver or a mass filling the gallbladder should raise suspicion for malignancy.

CLINICAL FINDS
The most common presenting symptoms are right upper quadrant pain, jaundice, nausea/vomiting, and fever. This spectrum of findings overlaps with several other pathologic processes of the hepatobiliary tract, making preoperative diagnosis difficult. Additionally, the clinical picture may be complicated by the concurrent presence of acute cholecystitis, pancreatitis, or even gallstone ileus. Mirizzi’s syndrome should be suspected in any patient presenting with right upper quadrant pain and abnormal liver enzymes (particularly elevated bilirubin and alkaline phosphatase) or imaging suggestive of an impacted stone. Three findings on imaging together suggest a diagnosis of Mirizzi’s: 1) dilation of the biliary system above the level of the gallbladder neck, 2) the presence of a stone impacted in the gallbladder neck, and 3) an abrupt change to a normal width of the common duct below the level of the stone. Such findings should prompt further imaging to better define the biliary tree, either indirectly though magnetic resonance cholangiopancreatography (MRCP), or directly through endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic cholangiography (PTC). No imaging modality is entirely sensitive for Mirizzi’s syndrome and the key is to maintain a high index of suspicion.
MANAGEMENT
Management of Mirizzi’s syndrome depends on the degree of fistula. In Type I disease, laparoscopic cholecystectomy is usually achievable, either total (classic) or subtotal, depending on the specific intraoperative findings. If the view of safety can be attained with the critical structures isolated, a classic cholecystectomy may be performed. If the view of safety cannot be achieved due to inflammation or adhesions, the gallbladder is taken down retrograde and opened near the cystic duct orifice. All stones are removed, including any impacted stones, and the cystic duct orifice is examined for the presence of bile to determine whether it is patent. If the cystic duct is patent, it should be ligated (if possible), or the remnant gallbladder should be sutured closed over it (choledochoplasty). An external closed suction drain may be left in the gallbladder fossa and removed the following day if drainage is non-bilious. More commonly, the cystic duct is obliterated, and a subtotal cholecystectomy with removal of all stones is sufficient.
Management of Mirizzi’s syndrome in the presence of a biliobiliary fistula is more complex. If the fistula involves <1/3 of the CBD circumference (Type II), options include primary repair using absorbable suture, closure over a T-tube, or choledochoplasty using the remnant gallbladder. The last approach is preferable to maintain the diameter of the CBD and minimize the risk of subsequent stricture but requires that sufficient gallbladder remnant be available to allow closure. In the presence of a more extensive fistula (Type III or IV), bilioenteric anastomosis is usually the best option.
Transplantation for nonalcoholic steatohepatitis

INTRODUCTION
The global obesity epidemic has dramatically increased the prevalence of NAFLD and made it the leading cause of chronic liver disease in Western nations. NAFLD is considered the hepatic manifestation of the metabolic syndrome and shares a strong association with type 2 diabetes mellitus, obstructive sleep apnea (OSA), and cardiovascular disease. Although cardiovascular disease is the leading cause of death in patients with NAFLD, the subset of patients who meet histopathologic criteria for NASH are those at greatest risk of liver-related morbidity and mortality. Ludwig and colleagues coined the term NASH in 1980 to describe a cohort of middle-aged patients with elevated serum liver enzyme levels who had evidence of alcohol-associated hepatitis on biopsy specimens in the absence of alcohol consumption. Subsequent study led to the proposed “2-hit” hypothesis in which a sequential progression from isolated fatty liver (IFL) to NASH involved the initial “hit” of hepatic steatosis followed by a second “hit” of oxidative stress resulting in liver injury. It was subsequently recognized that patients who have steatohepatitis on a liver biopsy specimen are at greatest risk for progression to cirrhosis compared with those who have IFL. Correspondingly, our understanding of the pathogenesis of NAFLD has evolved from the 2-hit hypothesis. NASH is expected to become the most common cause of cirrhosis and the leading indication for LT in the USA in the 2020s. As a major public health concern, an understanding of its epidemiology and pathogenesis is paramount to facilitate our ability to effectively diagnose and treat patients with NAFLD and NASH.
EPIDEMIOLOGY
NAFLD is an increasingly frequent cause of cirrhosis and HCC. In fact, a report published in 2018 listed NAFLD as the second leading non-neoplastic indication for LT in adults in the USA, following alcohol-associated liver disease. Obesity (BMI ≥30 kg/m2) and type 2 diabetes mellitus are commonly encountered in patients with NAFLD; these 2 diseases have been recognized as risk factors for HCC, irrespective of the presence or etiology of cirrhosis. Although BMI is not necessarily a reliable indicator of adiposity in patients with end-stage liver disease, particularly in those with fluid retention and ascites, it is commonly used by many LT centers during the patient selection process. Morbid obesity (BMI ≥40 kg/m2 without significant obesity-related comorbidities or BMI ≥35 kg/m2 associated with obesity-related comorbidities) is commonly regarded as a relative contraindication to LT; however, data from the Organ Procurement and Transplantation Network demonstrate that 16.5% and 5% of patients who underwent LT in 2016 had a BMI greater than or equal to 35 kg/m2 and greater than or equal to 40 kg/m2, respectively.
NAFLD and Liver Transplantation
Analysis of data from the UNOS registry has suggested that the risk of primary graft nonfunction is increased and short- and long-term survival is poorer in morbidly obese liver transplant recipients with various causes of end-stage liver disease. However, when analyzed as an entire cohort and not stratified by BMI, patients with NAFLD have patient and graft survival rates that are comparable to those for other indications for LT. Many of the key precipitants of NAFLD (obesity, hyperlipidemia, and insulin resistance) are exacerbated by immunosuppression. Recurrence of NAFLD after LT causes graft injury, although graft loss does not typically occur. De novo NAFLD after LT has also been described. In the absence of specific therapy for NAFLD, therapeutic efforts after LT should center on weight control, optimal diabetic management, and use of a lipid-lowering agent, if indicated. Intensive noninvasive weight loss interventions pre-LT appear to be successful (reduction of BMI to <35 kg/m2) in a large proportion of patients (84%) enrolled in carefully monitored multidisciplinary protocols; however, 60% of patients regained weight to a BMI ≥35 kg/m2 post-LT. Although bariatric surgery is feasible in selected patients with NAFLD, this intervention is typically reserved for patients with early stages of liver disease and, as is the case for many other abdominal surgical procedures, is contraindicated in those with decompensated cirrhosis because of high morbidity and mortality. A strategy of combining LT with sleeve gastrectomy during the same operation has only been evaluated in small prospective series. The mean surgical time was not significantly different between LT and combined LT/sleeve gastrectomy, and the mean BMI reduction with the combined surgical approach was 20 kg/m2. Metabolic complications, such as post-transplant diabetes mellitus, as well as steatosis of the graft noted by US were significantly less frequent in patients undergoing LT/sleeve gastrectomy compared with patients who lost weight noninvasively pre-LT. The safety and efficacy of this combined surgical approach and other combinations of less invasive weight loss interventions, such as endoscopic techniques, pre-LT must be confirmed by large prospective studies before they can be recommended. Bariatric interventions are still an option post-LT; however, the procedure should be performed by an experienced surgeon, and the role of less invasive endoscopic techniques postLT is still under investigation.
Sleeve Gastrectomy vs NAFLD
Bariatric surgery leads to substantial weight loss that results in improved metabolic parameters and hepatic histology in patients with NAFLD, according to numerous large retrospective and prospective cohort studies. In one study of 109 patients with NASH who underwent follow-up liver biopsy one year after bariatric surgery, 85% of patients had resolution of NASH, and 33% had improvement in fibrosis. Initial concerns that fibrosis would worsen with rapid weight loss were unfounded, as demonstrated in a meta-analysis in which fibrosis improved by 11.9% from baseline after bariatric surgery. Although bariatric surgery is not recommended as a treatment for NASH, the abundant positive data in its favor suggest that surgical weight loss is a viable option for patients with comorbid conditions that would warrant the surgery for other reasons. Patients with NASH cirrhosis are at potentially higher risk for surgical complications, although some centers have demonstrated encouraging results with sleeve gastrectomy in patients with Child-Pugh class A cirrhosis.
BASICS OF SURGICAL TECHNIQUE

This e-book was designed to assist in learning related to experimental surgical technique, during the training of health professionals. Concisely and objectively, it presents the basic principles for professional practice in surgery and in basic techniques of the most relevant surgical procedures. It is directed to the training of general practitioners, through the technical base, illustrated in procedures described step by step, with reference to the routines of the discipline of Surgical Technique, at the Federal University of Maranhão. It is not a work aimed at surgical clinic nor does it presuppose a descriptive detail that definitively supplies the necessary information for the execution of procedures in patients. This book is specially dedicated to undergraduate students, to serve as a guide during the Experimental Surgical Technique. It was designed and structured in order to facilitate theoretical study and encourage practical learning. Assisting your training, we seek professionals better prepared for health care.
Good Studies.
Laparoscopic Liver Resection
INTRODUCTION
Laparoscopic hepatic resection is an emerging option in the field of hepatic surgery. With almost 3000 laparoscopic hepatic resections reported in the literature for benign and malignant tumors, with a combined mortality of 0.3% and morbidity of 10.5%, there will be an increasing demand for minimally invasive liver surgery. Multiple series have been published on laparoscopic liver resections; however, no randomized controlled trial has been reported that compares laparoscopic with open liver resection. Large series, meta-analyses, and reviews have thus far attested to the feasibility and safety of minimally invasive hepatic surgery for benign and malignant lesions.
THECNICAL ASPECTS
The conversion rate from a laparoscopic approach to an open procedure was 4.1%. The most common type of laparoscopic liver resection performed is a wedge resection or segmentectomy (45%), followed by left lateral sectionectomy (20%). Major anatomic hepatectomies are still less frequently performed: right hepatectomy (9%) and left hepatectomy (7%). Cumulative morbidity and mortality was 10.5% and 0.3%.
BENEFITS OF LAPAROSCOPIC APPROACH
More importantly, almost all the studies comparing laparoscopic with open liver resection consistently showed a significant earlier discharge to home after laparoscopic liver resection. Lengths of stay were variable based on the country of origin of the studies but were consistently shorter for laparoscopic liver resection. Three studies published in the United States presented a length of stay of 1.9 to 4.0 days after laparoscopic liver resection. Studies from Europe showed an average length of stay of 3.5 to 10 days whereas those from Asia reported an average of length of stay of 4 to 20 days after laparoscopic liver resection.
COST ANALYSIS
Vanounou and colleagues used deviation-based cost modeling to compare the costs of laparoscopic with open left lateral sectionectomy at the University of Pittsburgh Medical Center. They compared 29 laparoscopic with 40 open cases and showed that patients who underwent the laparoscopic approach faired more favorably with a shorter length of stay (3 vs 5 days, P<.0001), significantly less postoperative morbidity (P 5 .001), and a weighted-average median cost savings of $1527 to $2939 per patient compared with patients who underwent open left lateral sectionectomy.
SURGICAL MARGINS
Initial concerns about the adequacy of surgical margins and possible tumor seeding prevented the widespread adoption of laparoscopic resection approaches for liver cancers. In comparison studies, there were no differences in margin-free resections between laparoscopic and open liver resection. In addition, no incidence of port-site recurrence or tumor seeding has been reported. With more than 3000 cases of minimally invasive hepatic resection reported in the literature (and no documentation of any significant port-site or peritoneal seeding), the authors conclude that this concern should not prevent surgeons from accepting a laparoscopic approach.
SURVIVAL OUTCOMES
There were no significant differences in overall survival in the 13 studies that compared laparoscopic liver resection with open liver resection for cancer. For example, Cai and colleagues showed that the 1-, 3-, and 5-year survival rates after laparoscopic resection of HCC were 95.4%, 67.5%, and 56.2% versus 100%, 73.8%, and 53.8% for open resection. For resection of colorectal cancer liver metastasis, Ito and colleagues showed a 3-year survival of 72% after laparoscopic liver resection and 56% after open liver resection whereas Castaing and colleagues51 showed a 5-year survival of 64% after laparoscopic liver resection versus 56% after open liver resection.
CONCLUSION
Compared with open liver resections, laparoscopic liver resections are associated with less blood loss, less pain medication requirement, and shorter length of hospital stay. A randomized controlled clinical trial is the best method to compare laparoscopic with open liver resection; however, such a trial may be difficult to conduct because patients are unlikely to subject themselves to an open procedure when a minimally invasive approach has been shown feasible and safe in experienced hands. In addition, many patients would have to be accrued to detect a difference in complications that occur infrequently. Short of a large randomized clinical trial, meta-analysis and matched comparisons provide the next best option to compare laparoscopic with open liver resection. For laparoscopic resection of HCC or colorectal cancer metastases, there has been no difference in 5-year overall survival compared with open hepatic resection. In addition, from a financial standpoint, the minimally invasive approach to liver resection may be associated with higher operating room costs; however, the total hospital costs were offset or improved due to the associated shorter length of hospital stay with the minimally invasive approach.
Medically-Necessary, Time Sensitive: (MeNTS) Score
Operating During The COVID-19 Coronavirus Pandemic
“At the University of Chicago, members of the Department of Surgery decided to investigate this issue more precisely. As stay-at-home restrictions in some states are easing, and as non-emergency medical care is being reconsidered, how does one possibly triage the thousands upon thousands of patients whose surgeries were postponed? Instead of the term “elective,” the University of Chicago’s Department of Surgery chose the phrase “Medically-Necessary, Time Sensitive” (MeNTS). This concept can be utilized to better assess the acuity and safety when determining which patients can get to the operating room in as high benefit/low risk manner as possible. And unlike in any recent time in history, risks to healthcare staff as well as risks to the patient from healthcare staff, are now thrown into the equation. The work was published in the April issue of the Journal of the American College of Surgeons.
On March 17, 2020, the American College of Surgeons recommended that all “elective” surgeries be canceled indefinitely. These guidelines were published, stating that only patients with “high acuity” surgical issues, which would include aggressive cancers and severely symptomatic disease, should proceed. Based on the Elective Surgery Acuity Scale (ESAS), most hospitals were strongly encouraged to cancel any surgery that was not high acuity, including slow-growing cancers, orthopedic and spine surgeries, airway surgeries, and any other surgeries for non-cancerous tumors. Heart surgeries for stable cardiac issues were also put on hold. Patients and surgeons waited. Some patients did, indeed undergo non-Covid-19-related surgeries. But most did not. Redeployment is gradually turning to re-entry.
The re-entry process for non-urgent (yet necessary) surgeries is a complicated one. Decisions and timing, based on a given hospital’s number and severity of Covid-19 patients, combined with a given city or state’s current and projected number of Covid-19 cases, how sick those patients will be, and whether or not a second surge may come, involves a fair amount of guesswork. As we have all seen, data manipulation has become a daily sparring match in many arenas. The authors of the study created an objective surgical risk scoring system, in order to help hospitals across this country, as well as others across the world, better identify appropriate timing regarding which surgeries can go ahead sooner rather than later, and why. They factored several variables into their equation, to account for the multiple potential barriers to care, including health and safety of hospital personnel. They created scoring systems based on three factors: Procedure, Disease and Patient Issues.
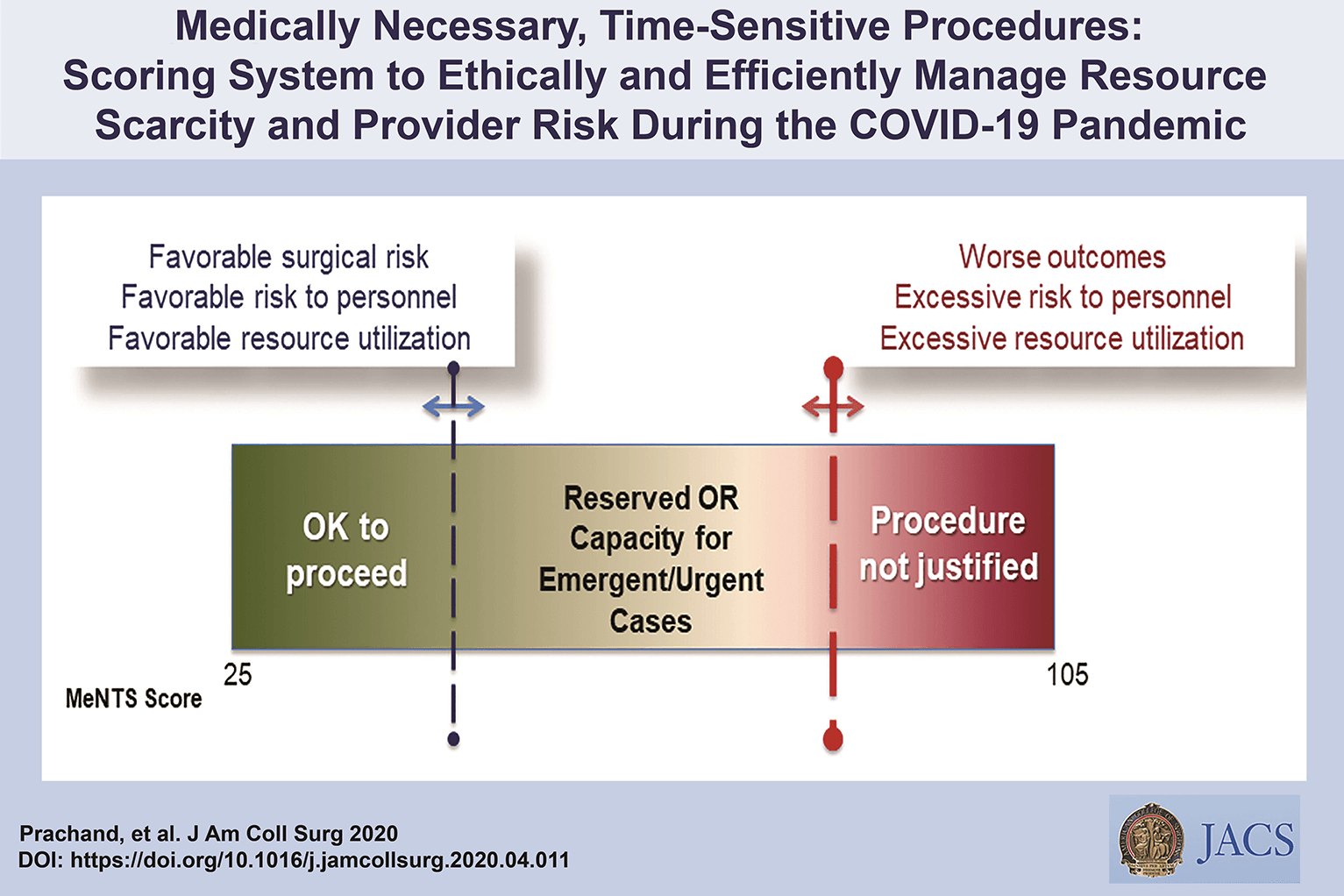
CALCULATE MeNTS SCORE HERE
The authors of the study created an objective surgical risk scoring system, in order to help hospitals across this country, as well as others across the world, better identify appropriate timing regarding which surgeries can go ahead sooner rather than later, and why. They factored several variables into their equation, to account for the multiple potential barriers to care, including health and safety of hospital personnel. Each patient would receive an overall conglomerate score, based on all of these factors, with the lower risks giving them more favorable scores to proceed with surgery soon, and the higher risks giving patients a higher score, or higher risk regarding proceeding with surgery, meaning it may be safest, for now, to wait.
Dr. Jeffrey Matthews, senior author of the paper, and Department Chair at the University of Chicago, stated that this model is reproducible across hospital systems, in urban, rural, and academic settings. And in the event of potential unpredictable surges of Covid-19 cases, the scoring system “helps prioritize cases not only from the procedure/disease standpoint but also from the pandemic standpoint with respect to available hospital resources such as PPE, blood, ICU beds, and [regular hospital] beds.”
The scoring system is extremely new, and the coming weeks will reveal how patients, surgeons and hospitals are faring as patients without life-and-death emergencies and/or Covid-19 complications gradually begin filling the operating rooms and hospital beds. In addition, and perhaps just as important, the study authors note that creating systems whereby healthcare resources, safety, and impact on outcomes need to be considered more carefully for each patient intervention, the larger impact of each intervention on public health will be better understood: not only for today’s pandemic, but also in future, as yet unknown, global events.”
Source: Nina Shapiro, 2020
Discover our surgical video channel and lectures associated with the surgeon blog.
Share and Join: https://linktr.ee/TheSurgeon
Covid-19 and Digestive Surgery
The current world Covid-19 pandemic has been the most discussed topic in the media and scientific journals. Fear, uncertainty, and lack of knowledge about the disease may be the significant factors that justify such reality. It has been known that the disease presents with a rapidly spreading, it is significantly more severe among the elderly, and it has a substantial global socioeconomic impact. Besides the challenges associated with the unknown, there are other factors, such as the deluge of information. In this regard, the high number of scientific publications, encompassing in vitro, case studies, observational and randomized clinical studies, and even systematic reviews add up to the uncertainty. Such a situation is even worse when considering that most healthcare professionals lack adequate knowledge to critically appraise the scientific method, something that has been previously addressed by some authors. Therefore, it is of utmost importance that expert societies supported by data provided by the World Health Organization and the National Health Department take the lead in spreading trustworthy and reliable information.
Discover our surgical video channel and lectures associated with the surgeon blog.
Share and Join: https://linktr.ee/TheSurgeon
#Medicine #Surgery #GeneralSurgery #DigestiveSurgery
#TheSurgeon #OzimoGama
Tratamento Cirúrgico do Abscesso Hepático Piogênico
Introdução
O abscesso hepático piogênico (AHP) é uma condição infecciosa grave caracterizada por uma coleção encapsulada de material purulento no fígado. Frequentemente, essa condição é resultante de infecções bacterianas, originárias do trato biliar ou de fontes intra-abdominais, como diverticulite. O manejo do AHP requer uma abordagem multidisciplinar, combinando diagnóstico rápido, antibioticoterapia e, em muitos casos, intervenção cirúrgica. No Brasil, a mortalidade associada a essa condição pode variar de 10% a 20%, sendo particularmente elevada em pacientes com comorbidades, como diabetes e cirrose. A presente revisão discute as abordagens cirúrgicas no tratamento do AHP, com ênfase nos critérios de intervenção, técnicas cirúrgicas e melhores práticas para o cirurgião do aparelho digestivo.
Diagnóstico e Classificação
O diagnóstico precoce do AHP é essencial para determinar a abordagem terapêutica mais adequada. Exames de imagem, como ultrassonografia (USG) e tomografia computadorizada (TC), são as ferramentas primárias para identificar a extensão da lesão e guiar a tomada de decisões. A classificação dos abscessos hepáticos baseia-se em seu tamanho e características morfológicas:
- Abscessos pequenos (menores que 3 cm) podem, muitas vezes, ser tratados com antibioticoterapia isolada.
- Abscessos maiores (geralmente >5 cm) e multiloculados exigem drenagem percutânea ou intervenção cirúrgica.
A etiologia do AHP no Brasil é predominantemente associada a bactérias como Escherichia coli e Klebsiella pneumoniae, e pacientes imunocomprometidos, como diabéticos, estão em maior risco de desenvolver complicações graves.
Abordagem Terapêutica
O tratamento do AHP é multimodal e deve ser adaptado à gravidade do caso, com o uso combinado de antibióticos, drenagem percutânea e intervenção cirúrgica, quando necessário. As diretrizes atuais propõem um algoritmo terapêutico baseado no tamanho e nas características dos abscessos.
1. Antibioticoterapia
A antibioticoterapia empírica deve ser iniciada imediatamente após o diagnóstico, visando cobertura para bactérias gram-negativas e anaeróbias. Ciprofloxacina ou cefixima combinadas com metronidazol são frequentemente utilizadas no manejo de abscessos hepáticos não complicados. A escolha do antibiótico deve ser ajustada conforme os resultados das culturas de sangue e de amostras do abscesso, garantindo uma abordagem personalizada.
2. Drenagem Percutânea
A drenagem percutânea, guiada por USG ou TC, é o tratamento de escolha para abscessos maiores que 3 cm e uniloculares (Tipo II). Esse método minimamente invasivo apresenta uma alta taxa de sucesso, próxima a 90%, sendo eficaz na maioria dos casos. No entanto, falhas podem ocorrer em abscessos multiloculados ou com conteúdo viscoso ou necrótico, situações em que a drenagem percutânea se torna inadequada, necessitando de intervenção cirúrgica.
3. Intervenção Cirúrgica
A cirurgia está indicada em abscessos multiloculados grandes (>3 cm, Tipo III), em abscessos que não respondem à drenagem percutânea ou na presença de complicações, como ruptura do abscesso. A cirurgia pode envolver drenagem minimamente invasiva ou ressecção hepática, dependendo da complexidade do abscesso e da experiência do cirurgião. Abscessos maiores que 10 cm apresentam maior risco de complicações, e nesses casos, a drenagem cirúrgica pode ser preferível. A laparotomia é recomendada em situações de peritonite ou quando o abscesso é de difícil acesso para drenagem percutânea.
4. Laparoscopia
A laparoscopia é uma alternativa minimamente invasiva à cirurgia aberta, indicada em abscessos uniloculares de tamanho moderado. Essa técnica oferece vantagens significativas, como menor tempo de internação e recuperação mais rápida, além de menor risco de complicações pós-operatórias.
Aplicação na Cirurgia Digestiva
O papel do cirurgião do aparelho digestivo é central no manejo dos abscessos hepáticos, especialmente em casos que requerem intervenção cirúrgica. A drenagem percutânea deve ser considerada a primeira linha de tratamento sempre que viável, mas o cirurgião deve estar preparado para realizar intervenções mais invasivas quando necessário. A laparoscopia tem demonstrado resultados promissores, reduzindo o tempo de internação e o risco de complicações. No Brasil, as infecções intra-abdominais complicadas são uma das principais causas de internação em emergências cirúrgicas, e o manejo adequado desses casos depende de uma sólida formação técnico-cirúrgica.
Algoritmo de Tratamento
Com base nas evidências disponíveis, um algoritmo de tratamento para o AHP pode ser delineado da seguinte forma:
- Abscessos pequenos (<3 cm, Tipo I): Tratamento com antibióticos isolados.
- Abscessos grandes uniloculares (>3 cm, Tipo II): Drenagem percutânea associada a antibioticoterapia.
- Abscessos grandes multiloculados (>3 cm, Tipo III): Intervenção cirúrgica.
Pontos-Chave
- Diagnóstico Precoce: O uso da TC com contraste é fundamental para o diagnóstico preciso do tamanho e da localização dos abscessos hepáticos, orientando a decisão terapêutica.
- Intervenção Cirúrgica: Abscessos multiloculados ou maiores que 5 cm frequentemente requerem intervenção cirúrgica, especialmente quando a drenagem percutânea falha.
- Abordagem Minimamente Invasiva: A laparoscopia oferece uma alternativa eficaz à cirurgia aberta, proporcionando uma recuperação mais rápida e com menor morbidade.
- Manejo Integral pelo Cirurgião Digestivo: O conhecimento técnico-cirúrgico é essencial para o manejo de abscessos hepáticos complexos, garantindo uma abordagem eficaz e personalizada.
Conclusão
O manejo do abscesso hepático piogênico exige uma abordagem multidisciplinar, sendo o cirurgião digestivo uma peça-chave no tratamento de casos complexos. A decisão entre drenagem percutânea e intervenção cirúrgica deve considerar múltiplos fatores, como o tamanho do abscesso, a resposta ao tratamento conservador e as condições clínicas do paciente. Como afirmou o Prof. Henri Bismuth: “Le traitement chirurgical n’est pas seulement une question de technique, mais de jugement. Le moment de l’intervention est aussi important que l’intervention elle-même.” Assim, o domínio técnico e a tomada de decisões precisas são fundamentais para o sucesso terapêutico no tratamento do AHP.
Gostou ❔Nos deixe um comentário ✍️, compartilhe em suas redes sociais e|ou mande sua dúvida pelo 💬 Chat On-line em nossa DM do Instagram.
#AbscessoHepatico #CirurgiaDigestiva #TratamentoAbscesso #DrenagemPercutanea #AparelhoDigestivo
Anatomia Cirúrgica Pancreática
A anatomia cirúrgica do pâncreas é um dos tópicos mais fascinantes e desafiadores da cirurgia do aparelho digestivo. Conhecer detalhadamente a estrutura e a topografia do pâncreas é crucial para a realização de procedimentos cirúrgicos seguros e eficazes. Neste artigo, vamos explorar os aspectos mais importantes da anatomia pancreática, abordando pontos-chave para estudantes de medicina e residentes de cirurgia do aparelho digestivo.
Estrutura Anatômica do Pâncreas
O pâncreas é uma glândula retroperitoneal situada transversalmente no abdome, na altura das vértebras L1-L2, abrangendo os principais vasos sanguíneos e a coluna vertebral. Ele é composto por cinco partes principais: cabeça, colo, corpo, cauda e processo uncinado.
- Cabeça: Localizada à direita da linha média, cercada pelo duodeno. A cabeça do pâncreas possui uma extensão inferior chamada processo uncinado, que está intimamente relacionada com a veia mesentérica superior e a artéria mesentérica superior.
- Colo: Uma parte estreita entre a cabeça e o corpo, situada anteriormente à veia porta, definida pela localização anatômica anterior à formação da veia porta, geralmente pela confluência das veias mesentérica superior e esplênica.
- Corpo: Estende-se para a esquerda, posterior ao estômago, com a superfície anterior coberta pelo peritônio, formando parte da parede posterior do saco menor.
- Cauda: Parte terminal que se estende até o hilo esplênico, confinada entre as camadas do ligamento esplenorrenal juntamente com a artéria esplênica e a origem da veia esplênica.
- Processo Uncinado: Considerado uma parte distinta do pâncreas devido à sua origem embriológica diferente, estendendo-se posteriormente aos vasos mesentéricos superiores.
Peso e Dimensões Normais
Em um adulto saudável, o pâncreas tem um peso médio de aproximadamente 80 a 120 gramas. As dimensões normais do pâncreas variam, mas geralmente medem cerca de 15 a 20 cm de comprimento, 4 a 5 cm de largura na cabeça, e 1,5 a 2,5 cm de espessura.
Vascularização do Pâncreas
A vascularização do pâncreas é complexa e vital para a compreensão cirúrgica. As principais artérias que irrigam o pâncreas são:
- Artéria Pancreatoduodenal Superior: Ramo da artéria gastroduodenal que irriga a cabeça do pâncreas.
- Artéria Pancreatoduodenal Inferior: Ramo da artéria mesentérica superior que também fornece sangue à cabeça do pâncreas.
- Ramos Pancreáticos da Artéria Esplênica: Irrigam o corpo e a cauda do pâncreas.
As veias pancreáticas drenam para a veia esplênica, veia mesentérica superior e, eventualmente, para a veia porta.
Ductos Pancreáticos
O pâncreas possui dois principais ductos: o ducto pancreático principal (ducto de Wirsung) e o ducto pancreático acessório (ducto de Santorini).
- Ducto Pancreático Principal (Ducto de Wirsung): Começa na cauda do pâncreas e percorre o corpo até a cabeça, onde geralmente se junta ao ducto biliar comum na ampola de Vater, regulada pelo esfíncter de Oddi. O diâmetro normal do ducto pancreático principal varia de 1 mm na cauda até 3 mm na cabeça.
- Ducto Pancreático Acessório (Ducto de Santorini): Corre superior e paralelo ao ducto de Wirsung, drenando parte da cabeça do pâncreas na papila duodenal menor.
O esfíncter de Oddi é uma estrutura única de fibras musculares lisas que regula o fluxo das secreções biliares e pancreáticas para o duodeno e impede o refluxo do conteúdo intestinal para o sistema ductal pancreatobiliar.
Considerações Cirúrgicas
Entender a anatomia pancreática é essencial para evitar complicações durante procedimentos cirúrgicos. Algumas das considerações importantes incluem:
- Ressecção Pancreática: Procedimentos como a pancreatoduodenectomia (procedimento de Whipple) requerem um conhecimento detalhado das relações anatômicas para garantir a remoção eficaz do tumor com a menor morbidade possível.
- Drenagem Biliar: A proximidade do pâncreas com o ducto biliar comum exige precisão ao evitar danos durante as cirurgias.
- Anastomoses Pancreáticas: A criação de anastomoses seguras entre o pâncreas e o intestino é crítica para prevenir complicações pós-operatórias, como fístulas pancreáticas.
Variações Anatômicas
As variações anatômicas do pâncreas e dos ductos pancreáticos são comuns e podem impactar significativamente a abordagem cirúrgica. Uma compreensão detalhada dessas variações é essencial para a personalização do plano cirúrgico. Por exemplo, o pâncreas anular é uma condição em que o tecido pancreático forma um anel ao redor do duodeno, podendo causar estenose duodenal.
Conclusão
A anatomia cirúrgica pancreática é um campo complexo e detalhado que exige estudo e prática contínuos. Compreender as nuances dessa anatomia é fundamental para qualquer cirurgião do aparelho digestivo. Como disse o renomado anatomista Andreas Vesalius: “A anatomia é a fundação de todas as ciências médicas.”
Gostou? Nos deixe um comentário ✍️, ou mande sua dúvida pelo 💬 Chat On-line em nossa DM do Instagram.
Hashtags
#AnatomiaPancreática #CirurgiaDigestiva #EstudantesDeMedicina #ResidentesDeCirurgia #Pancreas

Nutritional Management of Acute Pancreatitis
Acute pancreatitis is a common intra-abdominal inflammatory condition of varied aetiology. The disease is mild in the vast majority of patients and has a favourable outcome. The acute severe form of the disease on the other hand is a lethal form with a high mortality and morbidity. A number of strategies have provided clinical benefit in severe acute pancreatitis (SAP). Of these, nutritional management is by far the most effective. SAP is associated with persistent end-organ failure, commonly respiratory, circulatory and renal. Treatment is targeted to support these organs. As of now there is no definitive therapy for acute pancreatitis. Patients are managed with fluids, analgesics, antibiotics and nutritional supplements besides adequately treating local complications such as pseudocyst and walled-off pancreatic necrosis by suitable interventional methods, be it endoscopic or percutaneous. The focus here is nutritional support in the management of SAP.
Which Form of Nutrition: Parenteral or Enteral?
This depends largely on the functional integrity of the stomach and small intestine. Patients of SAP often have poor gastric emptying and paralytic ileus, which is made worse with the use of narcotics. Moreover, local complications of pancreatitis (peripancreatic fluid collections) can have a pressure effect on the stomach and/or duodenum. As a result oral feeds may not be possible in these patients. Patients on ventilator support also cannot be given oral feeds.
Enteral feeding through the nasogastric or nasojejunal tubes is often not tolerated by patients because of discomfort. In addition, these tubes often get displaced or withdrawn. Reinsertion of the tubes, under endoscopic or radiological guidance, is cumbersome in such patients. All these factors favour parenteral feeding. The distinct advantage of enteral nutrition is that it prevents mucosal atrophy and transmigration of bacteria (an important causeof sepsis in SAP). Also, enteral feeding augments intestinal motility and is cheaper than parenteral preparations. Enteral nutrition improves motility in patients with paralytic ileus. The relative merits of these forms of nutritional therapy have been evaluated in a systematic review. Eight published randomized trials including a total of 348 patients were included. Enteral feeding was given through a nasojejunal tube and parenteral nutrition through a catheter placed in a central vein. Enteral nutrition was shown to reduce mortality, multi-organ failure, systemic infection and surgical intervention in comparison with parenteral nutrition. The length of hospital stay too was shown to be reduced. In view of these, enteral nutrition appears to be a better option while managing patients of SAP and has been recommended by the American College of Gastroenterology, American Gastroenterological Association and International Association of Pancreatology.
When should enteral feeding be started?
Patients with mild acute pancreatitis can usually be started on oral feeds in 2–3 days. Those with moderately severe acute pancreatitis can be started on oral feeding only after a variable period and hence should receive enteral nutritional support. Early enteral feeding has been shown to avoid end-organ failure in a large series of patients (1200).
Enteral feeding started within 48 h of onset of illness was associated with organ failure in 21% of patients as opposed to 81% when enteral feeding was started after 48 h. This benefit of early enteral feeding has also been shown in a recent meta-analysis. However, there was no benefit in mortality with early enteral feeding. In yet another randomized controlled trial, early enteral feeding (within 24 h) was compared with on-demand enteral feeding after 72 h.
The primary endpoint of this study was major infection or death. The study did not detect any significant difference in the primary endpoint in either group (early or on-demand feeding). However, it did show that patients receiving on-demand nutrition tolerated oral feeds without using a tube.
- Nasogastric or Nasojejunal
Should the feed be administered in the stomach through a nasogastric (NG) tube or in the jejunum through a nasojejunal (NJ) tube? Gastric feeding is thought to increase pain and aggravate pancreatitis due to food-induced pancreatic stimulation. In view of this, NJ feeding is practised. However, placement of a NJ tube is cumbersome and needs a skilled endoscopist or radiologist. It causes more inconvenience to patients. A nasogastric (NG) tube is thus an alternative. A number of studies have been published comparing NG and NJ feeding. The results of these studies can be summarized as follows: There was no difference in mortality. Feeds were equally tolerated in the two groups and NG feeding is simple. NG feed was not shown to increase pain and is thus as good as NJ feeding. A meta-analysis subsequently published showed no difference in mortality, hospital stay and infection rate between the two groups. Both forms of feeding were equally well tolerated. NJ feeding thus is not advised in the management of most patients with SAP. However, it still has a place when the patient has a high risk of aspiration. Also, patients on a ventilator and those not tolerating NG feed should be fed through NJ tube. The other issue concerning enteral feeding in SAP is the composition of the feed.
- Type of Formulation
Various commercially available formulations include (1) polymeric formulations comprising complex lipids, carbohydrates and proteins and (2) elemental formulations comprising simple amino acids, carbohydrates and free fatty acids. Other formulations used are glutamine-rich feeds and feeds with probiotics, fibres, etc. Immuno-nutrition using arginine, glutamine and polyunsaturated fatty acids has been evaluated in multiple studies and compared with standard feeding. A metaanalysis showed some benefit in mortality but not for prevention of infection, end-organ failure or inflammatory response. This benefit was not seen with the use of probiotics or fibre-based feeds. A systematic review did not show any benefit of immuno-nutrition or probiotics. It also showed that polymeric formulations are as well tolerated as oligomeric ones (elemental).