Non Operative Management of SPLENIC TRAUMA

The spleen, an important component of the reticuloendothelial system in normal adults, is a highly vascular solid organ that arises as a mass of differentiated mesenchymal tissue during early embryonic development. The normal adult spleen weighs between 75 and 100 g and receives an average blood flow of 300 mL/min. It functions as the primary filter of the reticuloendothelial system by sequestering and removing antigens, bacteria, and senescent or damaged cellular elements from the circulation. In addition, the spleen has an important role in humoral immunity because it produces immunoglobulin M and opsonins for the complement activation system.
The increased availability of high-resolution CT scan and advances in arterial angiography and embolization techniques have contributed to the success of nonoperative management of splenic injuries.
The hemodynamically stable patient with blunt splenic trauma can be adequately managed with bed rest, serial abdominal exams, and hemoglobin and hematocrit monitoring. This approach, in combination with occasional angiography, especially for grade III and IV injuries, confers a splenic salvage rate of up to 95%.
In the setting of expectant management, indications for angiography have been delineated by several studies and include the following CT scan features: contrast extravasation, the presence of a pseudoaneurysm, significant hemoperitoneum, high-grade injury, and evidence of a vascular injury. The goal of angiography is to localize bleeding and embolize the source with coils or a gelatin foam product. Embolization can occur either at the main splenic artery just distal to the dorsal pancreatic portion of the vessel—known as proximal embolization—or selectively at the distal branch of the injured vessel. The goal behind the former technique is to decrease the perfusion pressure to the spleen to encourage hemostasis. The disadvantage to this technique is global splenic ischemia, and many have questioned the spleen’s immunocompetence following proximal embolization.
Malhotra et al. examined the effects of angioembolization on splenic function by examining serum levels of a particular T-cell line. T-cell proportions between patients who had undergone splenic embolization with asplenic patients and healthy controls were similar suggesting some degree of splenic immunocompetency was maintained. A Norwegian study comparing blood samples from patients who had undergone angioembolization with healthy controls demonstrated that the study samples had similar levels of pneumococcal immunoglobulins and no Howell-Jolly bodies, suggesting normal splenic function. Although these preliminary studies remain encouraging, there is no definitive evidence that splenic immunocompetency is fully maintained following angio-embolization.
There is no question that advancements in interventional techniques have contributed to the successful nonoperative management of splenic injuries. This has certainly changed the strategy, but it has not completely replaced operative intervention. The challenge now remains predicting those patients who will ultimately require splenectomy.
Many groups have studied potential predictors of nonoperative failure. Earlier studies found that a higher injury grade, increased transfusion requirement, and hypotension on initial presentation consistently predicted failure of nonoperative management. More recent literature reflects the use of advanced imaging techniques for predicting which patients will ultimately require splenectomy. Haan looked at the overall outcomes of patients admitted with blunt splenic trauma and reported several radiographic findings that were prevalent among patients requiring splenectomy after angioembolization:
- contrast extravasation,
- pseudoaneurysm,
- significant hemoperitoneum,
- and arteriovenous fistula.
Among these characteristics, an arteriovenous fistula had the highest rate of nonoperative failure at 40%. Nonradiographic features associated with significant risk of nonoperative failure include age greater than 40, injury severity score of 25 or greater, or presence of large-volume hemoperitoneum.
Aside from radiographic findings, some groups have also examined the mechanism of injury and its association with nonoperative failure. Plurad et al. conducted a retrospective review over a 15-year period and found that patients who were victims of blunt assault were more likely to fail nonoperative management: 36% of these patients required splenectomy versus 11.5% of patients from all other mechanisms combined. These findings suggest that regardless of overall injury severity, individuals who sustain a direct transfer of injury to the left torso are more likely to require splenectomy.
Currently, the accepted standard of care for most splenic trauma is expectant management with close observation. Operative intervention is reserved for the hemodynamically labile patient who shows signs of active hemorrhage and who does not respond appropriately to fluid resuscitation. Although these clinical scenarios seem straightforward, it is often the condition of the patient who falls in between the two ends of the spectrum that can be the most challenging to manage. In the setting of advanced imaging techniques and interventional radiology, the trauma surgeon has more diagnostic information and more treatment options for the patient with splenic trauma.
IPMN Surgical Management

INTRODUCTION
IPMNs were first recognized in 1982 by Ohashi, but the term IPMN was not officially used until 1993. IPMNs are defined in the WHO Classification of Tumors of the Digestive System as an intraductal, grossly visible epithelial neoplasm of mucin-producing cells. Using imaging and histology, IPMNs can be classified into three types based on duct involvement:
1. Main-duct IPMN (approximately 25% of IPMNs): Segmental or diffuse dilation of the main pancreatic duct (>5 mm) in the absence of other causes of ductal obstruction.
2. Branch-duct IPMN (approximately 57% of IPMNs): Pancreatic cysts (>5 mm) that communicate with the main pancreatic duct.
3. Mixed type IPMN (approximately 18% of IPMNs): Meets criteria for both main and branch duct.
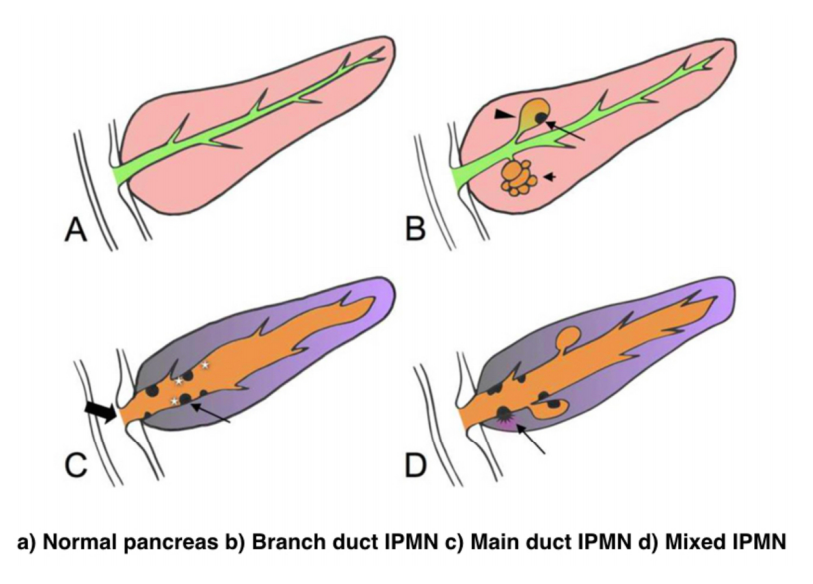
Due to the asymptomatic nature of the disease, the overall incidence of IPMNs is difficult to define but is thought to account for approximately 3% to 5% of all pancreatic tumors. Most IPMNs are discovered as incidental lesions from the workup of an unrelated process by imaging or endoscopy. IPMNs are slightly more prevalent in males than in females, with a peak incidence of 60 to 70 years of age. Branch-duct IPMNs tend to occur in a slightly younger population and are less associated with malignancy compared with main-duct or mixed variants.
Because a majority of IPMNs are discovered incidentally, most are asymptomatic. When symptoms do occur, they tend to be nonspecific and include unexplained weight loss, anorexia, abdominal pain, and back pain. Jaundice can occur with mucin obstructing the ampulla or with an underlying invasive carcinoma. The obstruction of the pancreatic duct can also lead to pancreatitis. IPMNs may represent genomic instability of the entire pancreas. This concept, known as a “field defect,” has been described as a theoretical risk of developing a recurrent IPMN or pancreatic adenocarcinoma at a site remote from the original IPMN. The three different types of IPMNs, main duct, branch duct, and mixed duct, dictate different treatment algorithms.
MAIN DUCT IPMNs
Main-duct IPMNs should be resected in all patients unless the risks of existing comorbidities outweigh the benefits of resection. The goal of operative management of IPMNs is to remove all adenomatous or potentially malignant epithelium to minimize recurrence in the pancreas remnant. There are two theories on the pathophysiologic basis of IPMNs. The first groups IPMNs into a similar category as an adenocarcinoma, a localized process involving only a particular segment of the pancreas. The thought is that removal of the IPMN is the only treatment necessary. In contrast, some believe IPMNs to represent a field defect of the pancreas. All of the ductal epithelium remains at risk of malignant degeneration despite removal of the cyst. Ideally, a total pancreatectomy would eliminate all risk, but this is a radical procedure that is associated with metabolic derangements and exocrine insufficiency. Total pancreatectomy should be limited to the most fit patients, with a thorough preoperative assessment and proper risk stratification prior to undertaking this surgery.
There is less uncertainty with treatment of main-duct IPMNs. The high incidence of underlying malignancy associated with the IPMNs warrants surgical resection. IPMNs localized to the body and tail (approximately 33%) can undergo a distal pancreatectomy with splenectomy. At the time of surgery, a frozen section of the proximal margin should be interpreted by a pathologist to rule out high-grade dysplasia. A prospective study identified a concordance rate of 94% between frozen section and final pathologic examination. If the margin is positive (high-grade dysplasia, invasion) additional margins may be resected from the pancreas until no evidence of disease is present. However, most surgeons will proceed to a total pancreatectomy after two subsequent margins demonstrate malignant changes. This more extensive procedure should be discussed with the patient prior to surgery, and the patient should be properly consented regarding the risks of a total pancreatectomy.
IPMNs localized to the head or uncinate process of the pancreas should undergo a pancreaticoduodenectomy. A frozen section of the distal margin should be analyzed by pathology for evidence of disease. As mentioned before, after two additional margins reveal malignant changes, a total pancreatectomy is usually indicated (approximately 5%). The absence of abnormal changes in frozen sections does not equate to negative disease throughout the pancreas remnant. Rather, skip lesions involving the remainder of the pancreas can exist and thus patients ultimately still require imaging surveillance after successful resection. A prophylactic total pancreatectomy is rarely performed because the subsequent pancreatic endocrine (diabetes mellitus) and exocrine deficits (malnutrition) carry an increased morbidity.
BRANCH DUCT IPMNs
Localized branch-duct IPMN can be treated with a formal anatomic pancreatectomy, pancreaticoduodenectomy, or distal pancreatectomy, depending on the location of the lesion. However, guidelines were established that allow for nonoperative management with certain branch- type IPMN characteristics.
These include asymptomatic patients with a cyst size less than 3 cm and lack of mural nodules. The data to support this demonstrate a very low incidence of malignancy (approximately 2%) in this patient group. Which nearly matches the anticipated mortality of undergoing a formal anatomic resection. In approximately 20% to 30% of patients with branch- duct IPMNs, there is evidence of multifocality. The additional IPMNs can be visualized on high-resolution CT or MRI imaging. Ideally, patients with multifocal branch-duct IPMNs should undergo a total pancreatectomy. However, as previously mentioned, the increased morbidity and lifestyle alterations associated with a total pancreatectomy allows for a more conservative approach. This would include removing the most suspicious or dominant of the lesions in an anatomic resection and follow-up imaging surveillance of the remaining pancreas remnant. If subsequent imaging demonstrates malignant charac- teristics, a completion pancreatectomy is usually indicated.
RECURRENCE RATES
Recurrence rates with IPMNs are variable. An anatomic resection of a branch-duct IPMN with negative margins has been shown to be curative. The recurrence of a main- duct IPMN in the remnant gland is anywhere from 0% to 10% if the margins are negative and there is no evidence of invasion. Most case series cite a 5-year survival rate of at least 70% after resection of noninvasive IPMNs. In contrast, evidence of invasive disease, despite negative margins, decreases 5-year survival to 30% to 50%. The recurrence rate in either the pancreatic remnant or distant sites approaches 50% to 90% in these patients. Histopathologic subtype of the IPMN is correlated with survival. The aggressive tubular subtype has a 5-year survival ranging from 37% to 55% following surgical resection, whereas the colloid subtype has 5-year survival ranging from 61% to 87% post resection. Factors associated with decreased survival include tubular subtype, lymph node metastases, vascular invasion, and positive margins. IPMNs with evidence of invasion should be treated similar to pancreatic adenocarcinomas. Studies show that IPMNs tend to have better survival than pancreatic adenocarcinoma. This survival benefit may be secondary to the less aggressive tumor biology or the earlier diagnosis of IPMNs.
SURVEILLANCE
All patients who have a resected IPMN should undergo imaging surveillance. There is continual survival benefit with further resection if an IPMN does recur. International Consensus Guidelines published in 2017 offer recom- mendations for the frequency and modality of imaging surveillance after resection. Routine serum measurement of CEA and CA 19-9 has a limited role for detection of an IPMN recurrence. Of note, a new pancreatic lesion discovered on imaging after resection could represent a postoperative pseudocyst, a recurrence of the IPMN from inadequate resection, a new IPMN, or an unrelated new neoplastic process. IPMNs may also be associated with extrapancreatic neoplasms (stomach, colon, rectum, lung, breast) and pancreatic ductal adenocarcinoma. It is unclear if this represents a true genetic syndrome. However, patients with IPMNs should have a discussion about the implications of their disease with their physician and are encouraged to undergo colonoscopy to exclude a synchronous neoplastic process.
The incidence of PANCREATIC CYSTIC LESIONS will continue to increase as imaging technology improves. EUS, cytology, and molecular panels have made differentiating the type of PCN less problematic. The importance of an accurate preoperative diagnosis ensures that operative management is selectively offered to those with high-risk lesions. Management beyond surgery, including adjuvant therapy and surveillance, continue to be active areas of research.
Perioperative Medicine

Surgery and anesthesia profoundly alter the normal physiologic and metabolic states. Estimating the patient’s ability to respond to these stresses in the postoperative period is the task of the preoperative evaluation. Perioperative complications are often the result of failure, in the preoperative period, to identify underlying medical conditions, maximize the patient’s preoperative health, or accurately assess perioperative risk. Sophisticated laboratory studies and specialized testing are no substitute for a thoughtful and careful history and physical examination. Sophisticated technology has merit primarily in confirming clinical suspicion.
Classroom: Perioperative Medicine
Hepatocellular Carcinoma: Resection Versus Transplantation

Hepatocellular carcinoma is the second most common cause of cancer mortality worldwide and its incidence is rising in North America, with an estimated 35,000 cases in the U.S. in 2014. The best chance for cure is surgical resection in the form of either segmental removal or whole organ transplantation although recent survival data on radiofrequency ablation approximates surgical resection and could be placed under the new moniker of “thermal resection”. The debate between surgical resection and transplantation focuses on patients with “within Milan criteria” tumors, single tumors, and well compensated cirrhosis who can safely undergo either procedure. Although transplantation historically has had better survival outcomes, early diagnosis, reversal of liver disease, and innovations in patient selection and neo-adjuvant therapies have led to similar 5-year survival. Transplantation clearly has less risk of tumor recurrence but exposes recipients to long term immunosuppression and its side effects. Liver transplantation is also limited by the severe global limit on the supply of organ donors whereas resection is readily available. The current data does not favor one treatment over the other for patients with minimal or no portal hypertension and normal synthetic function. Instead, the decision to resect or transplant for HCC relies on multiple factors including tumor characteristics, biology, geography, co-morbidities, location, organ availability, social support and practice preference.
Resection Versus Transplantation
The debate between resection and transplantation revolves around patients who have well compensated cirrhosis with Milan criteria resectable tumors. Patients within these criteria represent a very small proportion of those who initially present with HCC. This is especially true in western countries where hepatitis C is the most common cause of liver failure and HCC is a result of the progressive and in most cases advanced cirrhosis.
Given the need for a large number of patients to show statistical significance, it would be difficult to perform a high-quality prospective randomized controlled trial comparing resection and transplantation. In fact the literature revealed that no randomized controlled trials addressing this issue exist. Instead, outcomes of surgical treatment for HCC stem from retrospective analyses that have inherent detection, selection and attrition biases.
Given the numerous articles available on this subject, several meta-analyses have been published to delineate the role of transplantation and resection for treatment of HCC. However, there is reason to be wary of these meta-analyses because they pool data from heterogeneous populations with variable selection criteria and treatment protocols. One such meta-analysis by Dhir et al. focused their choice of articles to strict criteria which excluded studies with non-cirrhotic patients, fibrolamellar HCC and hepato-cholangiocarcinomas but included those with HCC within Milan criteria and computation of 5-year survival; between 1990 and 2011 they identified ten articles that fit within these criteria, of which six were ITT analyses, six included only well-compensated cirrhotics (Child-Pugh Class A without liver dysfunction) and three were ITT analyses of well-compensated cirrhotics.
Analysis of the six ITT studies that included all cirrhotics (n = 1118) (Child-Pugh Class A through C) showed no significant difference in survival at 5 years (OR = 0.600, 95 % CI 0.291– 1.237 l; p=0.166) but ITT analysis of only well-compensated cirrhotics (Child- Pugh Class A) revealed that patients undergoing transplant had a significantly higher 5-year survival as compared to those with resection (OR=0.521, 95 % CI 0.298–0.911; p=0.022).
A more recent ITT retrospective analysis from Spain assessed long-term survival and tumor recurrence following resection or transplant for tumors <5 cm in 217 cirrhotics (Child-Pugh Class A, B and C) over the span of 16 years. Recurrence at 5 years was significantly higher in the resection group (71.6 % vs. 16 % p<0.001) but survival at 4 years was similar (60 % vs. 62 %) which is likely explained by the evolving role of adjuvant therapies to treat post-resection recurrence.
Conclusions
- Patients with anatomically resectable single tumors and no cirrhosis or Child-Pugh Class A cirrhosis with normal bilirubin, HVPG (<10 mmHg), albumin and INR can be offered resection (evidence quality moderate; strong recommendation).
- Patients with Milan criteria tumors in the setting of Child- Pugh Class A with low platelets and either low albumin or high bilirubin or Child-Pugh Class B and C cirrhosis, especially those with more than one tumor, should be offered liver transplantation over resection (evidence quality moderate; strong recommendation).
- Those with Milan criteria tumors and Child-Pugh Class A cirrhosis without liver dysfunction should be considered for transplantation over resection (evidence quality low; weak recommendation).
- No recommendation can be made in regard to transplanting tumors beyond Milan criteria (evidence quality low) except to follow regional review board criteria.
- Pre-transplant therapies such as embolic or thermal ablation are safe and by expert opinion considered to be effective in decreasing transplant waitlist dropout and bridging patients to transplant (evidence quality low, weak recommendation). These interventions should be considered for those waiting longer than 6 months (evi- dence quality low, moderate recommendation).
- Living donor liver transplantation is a safe and effective option for treatment of HCC that are within and exceed Milan criteria (evidence quality moderate, weak recommendation).
The century of THE SURGEONS
Surgery is a profession defined by its authority to cure by means of bodily invasion. The brutality and risks of opening a living person’s body have long been apparent, the benefits only slowly and haltingly worked out. Nonetheless, over the past two centuries, surgery has become radically more effective, and its violence substantially reduced — changes that have proved central to the development of mankind’s abilities to heal the sick.
Consider, for instance, amputation of the leg.
The procedure had long been recognized as lifesaving, in particular for compound fractures and other wounds prone to sepsis, and at the same time horrific. Before the discovery of anesthesia, orderlies pinned the patient down while an assistant exerted pressure on the femoral artery or applied a tourniquet on the upper thigh.
Surgeons using the circular method proceeded through the limb in layers, taking a long curved knife in a circle through the skin first, then, a few inches higher up, through the muscle, and finally, with the assistant retracting the muscle to expose the bone a few inches higher still, taking an amputation saw smoothly through the bone so as not to leave splintered protrusions. Surgeons using the flap method, popularized by the British surgeon Robert Liston, stabbed through the skin and muscle close to the bone and cut swiftly through at an oblique angle on one side so as to leave a flap covering the stump.
The limits of patients’ tolerance for pain forced surgeons to choose slashing speed over precision. With either the flap method or the circular method, amputation could be accomplished in less than a minute, though the subsequent ligation of the severed blood vessels and suturing of the muscle and skin over the stump sometimes required 20 or 30 minutes when performed by less experienced surgeons.
No matter how swiftly the amputation was performed, however, the suffering that patients experienced was terrible. Few were able to put it into words. Among those who did was Professor George Wilson. In 1843, he underwent a Syme amputation — ankle disarticulation — performed by the great surgeon James Syme himself. Four years later, when opponents of anesthetic agents attempted to dismiss them as “needless luxuries,” Wilson felt obliged to pen a description of his experience:
“The horror of great darkness, and the sense of desertion by God and man, bordering close on despair, which swept through my mind and overwhelmed my heart, I can never forget, however gladly I would do so. During the operation, in spite of the pain it occasioned, my senses were preternaturally acute, as I have been told they generally are in patients in such circumstances. I still recall with unwelcome vividness the spreading out of the instruments: the twisting of the tourniquet: the first incision: the fingering of the sawed bone: the sponge pressed on the flap: the tying of the blood-vessels: the stitching of the skin: the bloody dismembered limb lying on the floor.”
It would take a little while for surgeons to discover that the use of anesthesia allowed them time to be meticulous. Despite the advantages of anesthesia, Liston, like many other surgeons, proceeded in his usual lightning-quick and bloody way. Spectators in the operating-theater gallery would still get out their pocket watches to time him. The butler’s operation, for instance, took an astonishing 25 seconds from incision to wound closure. (Liston operated so fast that he once accidentally amputated an assistant’s fingers along with a patient’s leg, according to Hollingham. The patient and the assistant both died of sepsis, and a spectator reportedly died of shock, resulting in the only known procedure with a 300% mortality.)
How to Choose a Mesh in Hernia Repair

Since the introduction of polypropylene (PP) mesh for hernia repair, surgeons continue to discuss the use of mesh in a variety of settings for one of the most common operations performed by general surgeons—hernia repair. This discussion has involved raw materials, cost, and outcomes and for many years referred to only a few products, as manufacturing was limited. Nowadays, with multiple permanent, absorbable, biologic, and hybrid products on the market, the choice of mesh for a hernia repair can be daunting. Increasing clinical complexity further emphasizes the need for individualizing care, but more frequently, hospital supply chain personnel institute product procurement procedures for cost control, limiting mesh choice for surgeons. This can force surgeons into a “one-size-fits-all” practice regarding mesh choice, which may not be ideal for some patients. Conversely, current literature lacks definitive evidence supporting the use of one mesh over another, a fact that has not escaped the radar screen of the hospital supply chain and mesh industry, both of which attempt to limit vendor and mesh choice for financial gain. It is unlikely that this type of “proof” will ever come to fruition. This leaves us with choosing a mesh based on an algorithm that is centered on the patient and the patient’s unique clinical scenario.
Article: Mesh in Hernia Repair
The Surgical Personality

Surgical stereotypes are remnants of the days of pre-anaesthesia surgery and include impulsivity, narcissism, authoritativeness, decisiveness, and thinking hierarchically. Medical students hold these stereotypes of surgeons early in their medical training. As Pearl Katz says in the The Scalpel’s Edge: ‘Each generation perpetuates the culture and passes it on by recruiting surgical residents who appear to resemble them and training these residents to emulate their thinking and behaviour.’ The culture of surgery has evolved, and certain behaviours are rightly no longer seen as acceptable, Non-technical skills such as leadership and communication have become incorporated into surgical training. Wen Shen, Associate Professor of Clinical Surgery at University of California San Francisco, argues that this has gone too far: ‘Putting likeability before surgical outcomes is like judging a restaurant by the waiters and ignoring the food,’ I would argue that operative and communication skills are indivisible, An aggressive surgeon is a threat to patient safety if colleagues are frightened to speak up for fear of a colleague shouting or, worse, throwing instruments. Conversely, a flattened hierarchy promotes patient safety.
Read More
Article: The Surgical Personality
The “GOOD” Surgeon
Surgery is an extremely enjoyable, intellectually demanding and satisfying career, and many more people apply to become surgeons each year than there are available places.
Those who are successful have to be ready not just to learn a great deal, but have the right kind of personality for the job.
Is a surgical career right for you?
Read the link…
THE GOOD SURGEON

Modern Concepts of Pancreatic Surgery
 Operations on the gallbladder and bile ducts are among the surgical procedures most commonly performed by general surgeons. In most hospitals, cholecystectomy is the most frequently performed operation within the abdomen. Pancreatic surgery is less frequent , but because of the close relation between the biliary system and the pancreas, knowledge of pancreatic problems is equally essential to the surgeon. Acute and chronic pancreatitis and cancer of the pancreas are often encountered by surgeons, with apparently increasing frequency; their treatment remains difficult and perplexing. This review demonstrates the modern aspects of pancreatic surgery. Good study.
Operations on the gallbladder and bile ducts are among the surgical procedures most commonly performed by general surgeons. In most hospitals, cholecystectomy is the most frequently performed operation within the abdomen. Pancreatic surgery is less frequent , but because of the close relation between the biliary system and the pancreas, knowledge of pancreatic problems is equally essential to the surgeon. Acute and chronic pancreatitis and cancer of the pancreas are often encountered by surgeons, with apparently increasing frequency; their treatment remains difficult and perplexing. This review demonstrates the modern aspects of pancreatic surgery. Good study.
AULA: PRÍNCIPIOS MODERNOS DA CIRURGIA PANCREÁTICA
Palestras e Vídeoaulas

Vejam nos links a seguir algumas de nossas palestras disponíveis para download no Canal do SlideShare e Videoaulas presentes no You Tube.
Postoperative Delirium

Postoperative delirium is recognized as the most common surgical complication in older adults,occurring in 5% to 50% of older patients after an operation. With more than one-third of all inpatient operations in the United States being performed on patients 65 years or older, it is imperative that clinicians caring for surgical patients understand optimal delirium care. Delirium is a serious complication for older adults because an episode of delirium can initiate a cascade of deleterious clinical events, including other major postoperative complications, prolonged hospitalization, loss of functional independence, reduced cognitive function, and death. The annual cost of delirium in the United States is estimated to be $150 billion. Delirium is particularly compelling as a quality improvement target, because it is preventable in up to 40% of patients; therefore, it is an ideal candidate for preventive interventions targeted to improve the outcomes of older adults in the perioperative setting. Delirium diagnosis and treatment are essential components of optimal surgical care of older adults, yet the topic of delirium is under-represented in surgical teaching.
Postoperative Delirium in Older Adults
Surgical treatment of ACUTE PANCREATITIS
Acute pancreatitis is more of a range of diseases than it is a single pathologic entity. Its clinical manifestations range from mild, perhaps even subclinical, symptoms to a life-threatening or life-ending process. The classification of acute pancreatitis and its forms are discussed in fuller detail by Sarr and colleagues elsewhere in this issue. For the purposes of this discussion, the focus is on the operative interventions for acute pancreatitis and its attendant disorders. The most important thing to consider when contemplating operative management for acute pancreatitis is that we do not operate as much for the acute inflammatory process as for the complications that may arise from inflammation of the pancreas. In brieSurgical treatment of acute pancreatitisf, the complications are related to: necrosis of the parenchyma, infection of the pancreas or surrounding tissue, failure of pancreatic juice to safely find its way to the lumen of the alimentary tract, erosion into vascular or other structures, and a persistent systemic inflammatory state. The operations may be divided into three major categories: those designed to ameliorate the emergent problems associated with the ongoing inflammatory state, those designed to ameliorate chronic sequelae of an inflammatory event, and those designed to prevent a subsequent episode of acute pancreatitis. This article provides a review of the above.
SURGICAL TREATMENT OF ACUTE PANCREATITIS
O TEMPLO DO CIRURGIÃO.
Templo (do latim templum, “local sagrado”) é uma estrutura arquitetônica dedicada ao serviço religioso. O termo também pode ser usado em sentido figurado. Neste sentido, é o reflexo do mundo divino, a habitação de Deus sobre a terra, o lugar da Presença Real. É o resumo do macrocosmo e também a imagem do microcosmo: ‘o corpo é o templo do Espírito Santo’ (I, Coríntios, 6, 19).
Dos locais especiais, O corpo humano (morada da alma), a Cavidade Peritoneal e o Bloco Cirúrgico, se bem analisados, são muito semelhantes e merecem atitudes e comportamentos respeitáveis. O Templo, em todos os credos, induz à meditação, absoluto silêncio tentando ouvir o Ser Supremo. A cavidade peritoneal | abdominal , espaço imaculado da homeostase, quando injuriada, reage gritando em dor, implorando uma precoce e efetiva ação terapêutica.
O Bloco Cirúrgico, abrigo momentâneo do indivíduo solitário, que mudo e quase morto de medo, recorre à prece implorando a troca do acidente, da complicação, da recorrência, da seqüela, da mutilação, da iatrogenia e do risco de óbito pela agressiva e controlada intervenção que lhe restaure a saúde, patrimônio magno de todo ser vivo.
O Bloco Cirúrgico clama por respeito ao paciente cirúrgico, antes mesmo de ser tomado por local banal, misturando condutas vulgares, atitudes menores, desvio de comportamento e propósitos secundários. Trabalhar no Bloco Cirúrgico significa buscar a perfeição técnica, revivendo os ensinamentos de William Stewart Halsted , precursor da arte de operar, dissecando para facilitar, pinçando e ligando um vaso sangüíneo, removendo tecido macerado, evitando corpos estranhos e reduzindo espaço vazio, numa síntese feita com a ansiedade e vontade da primeira e a necessidade e experiência da última.
Mas, se a cirurgia e o cirurgião vêm sofrendo grande evolução, técnica a primeira e científica o segundo, desde o início do século, a imagem que todo doente faz persiste numa simbiose entre mitos e verdades. A cirurgia significa enfrentar ambiente desconhecido chamado “sala de cirurgia” onde a fobia ganha espaço rumo ao infinito. O medo ainda prepondera em muitos.
A confiança neste momento além de um reconhecimento é um troféu que o cirurgião recebe dos pacientes e seus familiares. Tanto a CONFIANÇA quanto a SEGURANÇA têm que ser preservadas a qualquer custo. Não podem correr o risco de serem corroídas por palavras e atitudes de qualquer membro da equipe cirúrgica. Não foi tarefa fácil transformar, para a população, o ato cirúrgico numa atividade científica, indispensável, útil e por demais segura. Da conquista da cirurgia, como excelente arma terapêutica para a manutenção de um alto padrão de qualidade técnica, resta a responsabilidade dos cirurgiões, os herdeiros do suor e sangue, que se iniciou com o trabalho desenvolvido por Billroth, Lister, Halsted, Moyniham, Kocher e uma legião de figuras humanas dignas do maior respeito, admiração e gratidão universal.
No ato operatório os pacientes SÃO TODOS SEMELHANTES EM SUAS DIFERENÇAS, desde a afecção, ao prognóstico, ao caráter da cirurgia e especialmente sua relação com o ato operatório. Logo, o cirurgião tem por dever de ofício entrar no bloco cirúrgico com esperança e não deve sair com dúvida. Nosso trabalho é de equipe, cada um contribui com uma parcela, maior ou menor, para a concretização do todo, do ato cirúrgico por completo, com muita dedicação, profissionalismo e sabedoria. Toda tarefa, da limpeza do chão ao ato de operar, num crescendo, se faz em função de cada um e em benefício da maioria, o mais perfeito possível e de uma só vez, quase sempre sem oportunidade de repetição e previsão de término.
O trabalho do CIRURGIÃO é feito com carinho, muita dignidade, humildade e executado em função da alegria do resultado obtido aliado a dimensão ética do dever cumprido que transcende a sua existência. A vida do cirurgião se materializa no ato operatório e o bloco cirúrgico, palco do nosso trabalho não tolera e jamais permite atitudes menores, inferiores, ambas prejudiciais a todos os pacientes e a cada cirurgião. Como ambiente de trabalho de uma equipe diversificada, precisamos manter, a todo custo, o controle de qualidade, eficiência, eficácia e efetividade técnina associados aos mais altos valores ético, pois lidamos com o que há de mais precioso da criação divina na Terra: O SER HUMANO.
“Tem presença de Deus, como já a tens. Ontem estive com um doente, um doente a quem quero com todo o meu coração de Pai, e compreendo o grande trabalho sacerdotal que os médicos levam a cabo. Mas não se ponham orgulhosos, porque todas as almas são sacerdotais. Devem pôr em prática esse sacerdócio! Ao lavares as mãos, ao vestires a bata, ao calçares as luvas, pensa em Deus, e pensa nesse sacerdócio real de que fala São Pedro, e então não se te meterá a rotina: farás bem aos corpos e às almas” São Josemaria Escriva
Bariatric Complications

Over the past decade, following the publication of several long-term outcome studies that showed a significant improvement in cardiovascular risk and mortality after bariatric surgery, the number of bariatric procedures being carried out annually in the UK has grown exponentially. Surgery remains the only way to produce significant, sustainable weight loss and resolution of comorbidities. Nevertheless, relatively few surgeons have developed an interest in this field. Most bariatric surgery is now performed in centres staffed by surgeons with a bariatric interest, usually as part of a multidisciplinary team.
The commonest weight loss procedures performed around the world at present are the gastric band, the gastric bypass and the sleeve gastrectomy. In very obese patients, an alternative operation is the duodenal switch, while the new ileal transposition procedure represents one of the few purely metabolic operations designed specifically for the treatment of type II diabetes. Older operations such as vertical banded gastroplasty and jejuno-ileal bypass are now obsolete, although patients who have undergone such procedures in the distant past may still present to hospital with complications. The main endoscopic option at present is insertion of a gastric balloon, with newer procedures like the endoscopic duodenojejunal barrier and gastric plication on the horizon. Implantable neuroregulatory devices (gastric ‘pacemakers’) represent a new direction for surgical weight control by harnessing neural feedback signals to help control eating.
It should be within the capability of any abdominal surgeon to manage the general complications of bariatric surgery, which include pulmonary atelectasis/pneumonia, intra-abdominal bleeding, anastomotic or staple-line leak with or without abscess formation, deep vein thrombosis (DVT)/pulmonary embolus and superficial wound infections. Patients may be expected to present with malaise, pallor, features of sepsis or obvious wound problems. However, clinical features may be difficult to recognise owing to body habitus. Abdominal distension, tenderness and guarding may be impossible to determine clinically due to the patient’s obesity. Pallor is non-specific. Fever and leucocytosis may be absent. Wound collections may be very deep. These complications in a bariatric patient should be actively sought with appropriate investigations. In particular, it is vital for life-threatening complications such as bleeding, sepsis and bowel obstruction to be recognised promptly and treated appropriately. A persistent tachycardia may be the only sign heralding significant complications and should always be taken seriously. It is useful to classify complications as ‘early’, ‘medium’ and ‘late’ because, from the receiving clinician’s point of view, the differential diagnosis will differ accordingly.
Complications of bariatric surgery presenting to the GENERAL SURGEON
A “PROFISSÃO” CIRÚRGICA
 “A arte de curar vem do coração e da mente mais do que das mãos.” – Hipócrates
“A arte de curar vem do coração e da mente mais do que das mãos.” – Hipócrates
Na complexa tapeçaria da sociedade moderna, as profissões desempenham papéis fundamentais na organização dos serviços necessários ao bem-estar coletivo. Definida pelo American College of Surgeons, uma profissão é um campo onde a maestria de um corpo complexo de conhecimento e habilidades é essencial. É uma vocação em que o conhecimento científico ou a prática de uma arte, fundamentada nesse conhecimento, é empregada em benefício dos outros. O compromisso com a competência, a integridade e a moralidade forma a base de um contrato social entre a profissão e a sociedade, que concede à profissão um monopólio sobre o uso de seu conhecimento, considerável autonomia na prática e o privilégio da auto-regulação. Em troca, a profissão deve prestar contas a quem serve e à sociedade como um todo.
Os Elementos Essenciais da Profissão
No cerne de toda profissão estão quatro elementos fundamentais:
- Monopólio do Conhecimento Especializado: Profissionais detêm o direito exclusivo de utilizar conhecimentos e habilidades especializados, o que lhes confere uma posição única na sociedade.
- Autonomia e Auto-Regulação: Em troca deste monopólio, profissionais desfrutam de uma relativa autonomia na prática e são responsáveis pela sua própria regulação.
- Serviço Altruísta: A profissão deve servir tanto indivíduos quanto a sociedade de forma altruísta, colocando o bem-estar do paciente acima de outros interesses.
- Responsabilidade pela Manutenção e Expansão do Conhecimento: Profissionais são responsáveis por atualizar e expandir continuamente seu conhecimento e habilidades.
O Que é Profissionalismo?
Profissionalismo descreve as qualidades cognitivas, morais e colegiais de um profissional. É o conjunto de razões pelas quais um pai se orgulha de dizer que seu filho é um médico e cirurgião. Profissionalismo é mais do que apenas conhecimento técnico; é uma combinação de ética, respeito e dedicação ao ofício e ao paciente.
Por Que Precisamos de um Código de Conduta Profissional?
A confiança é o alicerce da prática cirúrgica. O Código de Conduta Profissional esclarece a relação entre a profissão cirúrgica e a sociedade que serve, frequentemente referido como contrato social. Para os pacientes, o código cristaliza o compromisso da comunidade cirúrgica em relação aos indivíduos e suas comunidades. A confiança é construída, tijolo por tijolo.
O Código de Conduta Profissional
O Código de Conduta Profissional aplica os princípios gerais do profissionalismo à prática cirúrgica e serve como a fundação sobre a qual os privilégios profissionais e a confiança dos pacientes e do público são conquistados. Durante o cuidado pré-operatório, intraoperatório e pós-operatório, os cirurgiões têm a responsabilidade de:
- Advogar Eficazmente pelos interesses dos pacientes.
- Divulgar Opções Terapêuticas incluindo seus riscos e benefícios.
- Divulgar e Resolver Conflitos de Interesse que possam influenciar as decisões de cuidado.
- Ser Sensível e Respeitoso com os pacientes, compreendendo sua vulnerabilidade durante o período perioperatório.
- Divulgar Completamente Eventos Adversos e Erros Médicos.
- Reconhecer Necessidades Psicológicas, Sociais, Culturais e Espirituais dos pacientes.
- Incorporar Cuidados Especiais para Pacientes Terminais.
- Reconhecer e Apoiar as Necessidades das Famílias dos Pacientes.
- Respeitar o Conhecimento, Dignidade e Perspectiva de outros profissionais de saúde.
A Necessidade do Código de Profissionalismo para Cirurgiões
Procedimentos cirúrgicos são experiências extremas que impactam os pacientes fisiológica, psicológica e socialmente. Quando os pacientes se submetem a uma experiência cirúrgica, devem confiar que o cirurgião colocará seu bem-estar acima de todas as outras considerações. O código escrito ajuda a reforçar esses valores, garantindo que a confiança e o compromisso sejam mantidos.
Princípios Fundamentais do Código de Conduta Profissional
- Primazia do Bem-Estar do Paciente: Os interesses do paciente sempre devem vir em primeiro lugar. O altruísmo é central para esse conceito, e é o altruísmo do cirurgião que fomenta a confiança na relação médico-paciente.
- Autonomia do Paciente: Pacientes devem entender e tomar suas próprias decisões informadas sobre o tratamento. Os médicos devem ser honestos para que os pacientes façam escolhas educadas, garantindo que essas decisões estejam alinhadas com práticas éticas.
- Justiça Social: Como médicos, devemos advogar pelos pacientes individuais enquanto promovemos a saúde do sistema de saúde como um todo. Precisamos equilibrar as necessidades dos pacientes (autonomia) sem desviar recursos escassos que beneficiariam a sociedade (justiça social).
“Não há maior coisa a ser conquistada do que a confiança dos pacientes e da sociedade, pois ela é a base sobre a qual construímos nossas práticas e nossa profissão.” – William Osler
Metabolismo Perioperatório
A melhor forma de se conhecer as necessidades energéticas é através de sua medida por calorimetria indireta, cada vez mais disponível em nosso ambiente hospitalar. Quando não se dispõe de calorimetria indireta, é possível estimar o gasto energético por meio de fórmulas estimativas que levam em conta, entre outros fatores, o peso e altura corpóreos, idade e sexo. Das diferentes fórmulas disponíveis, a equação de Harris-Benedict tem sido muito usada. Para homens a formula é 66,5 + (13.8 x peso [kg])+(5,0 x altura [cm]) – (6,8 x idade [anos]). Para mulheres a formula é diferente: 655 + (9,6 x peso [kg]) + (1,7 x altura [cm]) – (4,7 x idade [anos]). A regra de bolso (30-35 kcal/kg/dia) é mais prática e também é muito utilizada. No período pré-operatório a oferta de proteína deve ser em torno de 1,0-1,5 g/Kg/dia e, após trauma ou intervenção cirúrgica aumenta, podendo chegar até 2,0 g/Kg/dia. Em pacientes com SIRS moderado, a oferta calórica deve ser menor (25-30 kcal/kg/dia). Pacientes em estresse importante (SIRS grave, sepse) devem receber 20-25 kal/kg/dia e 1,5 a 2,0 g de proteínas/kg/dia. Deve-se evitar em pacientes gravemente desnutridos aporte rápido de calorias e proteínas (síndrome da realimentação). Nesses pacientes a oferta deve ser cautelosa com controle diário de fósforo, magnésio e potássio.
Aula: Suporte Nutricional Perioperatório
Tratamento Cirúrgico da Hemorragia digestiva alta por varizes esofágicas | Hipertensão Porta
O sistema portal é uma rede venosa de baixa pressão, com níveis fisiológicos <5 mmHg. Desta forma, o termo hipertensão portal (HP) designa uma síndrome clínica caracterizada pelo aumento mantido na pressão venosa em níveis acima dos fisiológicos. Ela é considerada clinicamente significante quando acima de 10 mmHg; neste nível existe o risco de surgimento de varizes esofagogástricas (VEG). Por sua vez, valores acima de 12 mmHg cursam com risco de rompimento dessas varizes, sua principal complicação.
ARTIGO DE REVISÃO – HIPERTENSÃO PORTAL
O aumento do fluxo como fator preponderante inicial da HP é raro e representado por fístulas arterioportais congênitas, traumáticas ou neoplásicas. O aumento da resistência é a condição fisiopatológica inicial mais comum e pode ser classificada de acordo com o local de obstrução ao fluxo em: pré-hepática, intra-hepática e pós-hepática. A HP intra-hepática responde pela grande maioria dos casos e pode ser subdividida de acordo com o local de acometimento estrutural no parênquima hepático em: pré-sinusoidal (ex: esquistossomose hepatoesplênica – EHE), sinusoidal (ex: cirrose hepática) e pós-sinusoidal (ex: doença venoclusiva). Em nosso meio, a maioria dos casos é decorrente da EHE e das hepatopatias crônicas complicadas com cirrose.
O tratamento da HP depende da causa subjacente, da condição clínica e do momento em que é realizado. Pacientes com função hepática comprometida têm abordagem diversa daqueles com ela preservada, como os portadores de EHE. Além disso, o tratamento pode ser emergencial (durante episódio agudo de hemorragia) ou eletivo, como profilaxia pré-primária, primária ou secundária. Por essa diversidade de situações clínicas, não existe modalidade única de tratamento.
O objetivo da aula abaixo foi avaliar os avanços e as estratégias atuais empregadas no tratamento emergencial e eletivo da hemorragia digestiva varicosa em pacientes cirróticos e esquistossomóticos.
AULA: TRATAMENTO CIRÚRGICO DA HIPERTENSÃO PORTAL
FERIDA PÓS-OPERATÓRIA

A avaliação e os cuidados de feridas pós-operatórias deve ser do domínio de todos os profissionais que atuam na clínica cirúrgica. O conhecimento a cerca dos processos relacionados a cicatrização tecidual é importante tanto nos cuidados como na prevenção de complicações, tais como: infecções e deiscência. Como tal, todos os profissionais médicos, sendo eles cirurgiões ou de outras especialidades, que participam do manejo clínico dos pacientes no período perioperatório devem apreciar a fisiologia da cicatrização de feridas e os princípios de tratamento de feridas pós-operatório. O objetivo deste artigo é atualizar os profissionais médicos de outras especialidades sobre os aspectos importantes do tratamento de feridas pós-operatório através de uma revisão da fisiologia da cicatrização de feridas, os métodos de limpeza e curativo, bem como um guia sobre complicações de feridas pós-operatórias mais prevalentes e como devem ser manejados nesta situação.
Esophagectomy: Anastomotic Complications (Leakage and Stricture)

Esophagectomy can be used to treat several esophageal diseases; it is most commonly used for treatment of esophageal cancer. Esophagectomy is a major procedure that may result in various complications. This article reviews only the important complications resulting from esophageal resection, which are anastomotic complications after esophageal reconstruction (leakage and stricture), delayed emptying or dumping syndrome, reflux, and chylothorax.
Causas de conversão da VIDEOCOLECISTECTOMIA
Atualmente, a colecistectomia laparoscópica é a abordagem preferida para o tratamento da litíase biliar, representando cerca de 90% dos procedimentos realizados, uma marca alcançada nos Estados Unidos em 1992. A popularidade dessa técnica se deve a suas vantagens evidentes: menos dor no pós-operatório, recuperação mais rápida, redução dos dias de trabalho perdidos e menor tempo de hospitalização. Apesar de ser considerada o padrão-ouro na cirurgia biliar, a colecistectomia laparoscópica não está isenta de desafios. Entre 2% e 15% dos casos podem exigir a conversão para cirurgia convencional. Os motivos mais comuns para essa conversão incluem dificuldades na identificação da anatomia, suspeita de lesão da árvore biliar e controle de sangramentos. Identificar os fatores que contribuem para uma maior taxa de conversão é essencial para a equipe cirúrgica. Isso não apenas permite uma avaliação mais precisa da complexidade do procedimento, mas também ajuda na preparação do paciente para possíveis riscos e na mobilização de cirurgiões mais experientes quando necessário. Em um cenário onde a precisão e a segurança são cruciais, a compreensão dos desafios e a preparação adequada podem fazer toda a diferença no resultado da cirurgia.
Relacionados ao Paciente: 1. Obesidade (IMC > 35), 2. Sexo Masculino, 3. Idade > 65 anos, 4. Diabetes Mellitus e 5. ASA > 2.
Relacionadas a Doença: 1. Colecistite Aguda, 2. Líquido Pericolecístico, 3. Pós – CPRE, 4. Síndrome de Mirizzi e 5. Edema da parede da vesícula > 5 mm.
Relacionadas a Cirurgia: 1. Hemorragia, 2. Aderências firmes, 3. Anatomia obscura, 4. Fístulas internas e 5. Cirurgia abdominal prévia.
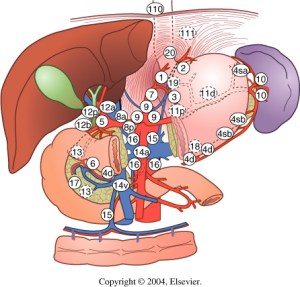
POST-HEPATECTOMY ADVERSE EVENTS
Hepatic resection had an impressive growth over time. It has been widely performed for the treatment of various liver diseases, such as malignant tumors, benign tumors, calculi in the intrahepatic ducts, hydatid disease, and abscesses. Management of hepatic resection is challenging. Despite technical advances and high experience of liver resection of specialized centers, it is still burdened by relatively high rates of postoperative morbidity and mortality. Especially, complex resections are being increasingly performed in high risk and older patient population. Operation on the liver is especially challenging because of its unique anatomic architecture and because of its vital functions. Common post-hepatectomy complications include venous catheter-related infection, pleural effusion, incisional infection, pulmonary atelectasis or infection, ascites, subphrenic infection, urinary tract infection, intraperitoneal hemorrhage, gastrointestinal tract bleeding, biliary tract hemorrhage, coagulation disorders, bile leakage, and liver failure. These problems are closely related to surgical manipulations, anesthesia, preoperative evaluation and preparation, and postoperative observation and management. The safety profile of hepatectomy probably can be improved if the surgeons and medical staff involved have comprehensive knowledge of the expected complications and expertise in their management.
Classroom: Hepatic Resections
The era of hepatic surgery began with a left lateral hepatic lobectomy performed successfully by Langenbuch in Germany in 1887. Since then, hepatectomy has been widely performed for the treatment of various liver diseases, such as malignant tumors, benign tumors, calculi in the intrahepatic ducts, hydatid disease, and abscesses. Operation on the liver is especially challenging because of its unique anatomic architecture and because of its vital functions. Despite technical advances and high experience of liver resection of specialized centers, it is still burdened by relatively high rates of postoperative morbidity (4.09%-47.7%) and mortality (0.24%-9.7%). This review article focuses on the major postoperative issues after hepatic resection and presents the current management.
REVIEW_ARTICLE_HEPATECTOMY_COMPLICATIONS
PANCREATIC PSEUDOCYST
Classroom: Principles of Pancreatic Surgery
The pancreatic pseudocyst is a collection of pancreatic secretions contained within a fibrous sac comprised of chronic inflammatory cells and fibroblasts in and adjacent to the pancreas contained by surrounding structures. Why a fibrous sac filled with pancreatic fluid is the source of so much interest, speculation, and emotion amongst surgeons and gastroenterologists is indeed hard to understand. Do we debate so vigorously about bilomas, urinomas, or other abdominal collections of visceral secretions? Perhaps it is because the pancreatic pseudocyst represents a sleeping tiger, which though frequently harmless, still can rise up unexpectedly and attack with its enzymatic claws into adjacent visceral and vascular structures and cause lifethreatening complications. Another part of the debate and puzzlement about pancreatic pseudocysts is related to confusion about pancreatic pseudocyst definition and nomenclature. The Atlanta classification, developed in 1992, was a pioneering effort in describing and defining morphologic entities in acute pancreatitis. Since then, a working group has been revising this system to incorporate more modern experience into the terminology. In the latest version of this system, pancreatitis is divided into acute interstitial edematous pancreatitis (IEP) and necrotizing pancreatitis (NP), based on the presence of pancreatic tissue necrosis. The fluid collections associated with these two “types” of pancreatitis are also differentiated. Early (<4 weeks into the disease course) peripancreatic fluid collections in IEP are referred to as acute peripancreatic fluid collections (APFC), whereas in NP, they are referred to as postnecrotic peripancreatic fluid collections (PNPFC). Late (>4 weeks) fluid collections in IEP are called pancreatic pseudocysts, and in NP, they are called walled-off pancreatic necrosis (WOPN).
Review of POSTGASTRECTOMY SYNDROMES

The first postgastrectomy syndrome was noted not long after the first gastrectomy was performed: Billroth reported a case of epigastric pain associated with bilious vomiting as a sequel of gastric surgery in 1885. Several classic treatises exist on the subject; we cannot improve on them and merely provide a few references for the interested reader. Surgical procedures on the stomach, performed for reasons such as peptic ulcer disease, cancer, obesity, or gastroesophageal reflux disease, can result in various post-gastrectomy syndromes. These syndromes include chronic symptoms that range from mild discomfort to life-altering conditions. This guide covers the most common syndromes and their characteristics.
GASTRECTOMY VIDEO SURGERY
Dumping Syndrome
Dumping Syndrome is characterized by gastrointestinal and vasomotor symptoms that occur after food intake due to rapid gastric emptying. This syndrome can occur after surgeries that alter the regulation of gastric emptying or gastric compliance, such as gastrectomy, proximal vagotomy, sleeve gastrectomy, fundoplication, pyloroplasty, and gastrojejunostomy (GJ). Depending on the speed of emptying and the osmolarity of gastric contents, symptoms can vary.
- Early Dumping: Occurs within 30 minutes after food intake and is characterized by palpitations, tachycardia, fatigue, a need to lie down after meals, flushing or pallor, sweating, dizziness, hypotension, headache, and possibly syncope. Abdominal symptoms include early satiety, epigastric fullness, abdominal pain, bloating, hypermotility, and splenic blood pooling.
- Late Dumping: Appears 1 to 3 hours after eating, due to reactive hypoglycemia caused by an initially high glucose load leading to an inappropriately high insulin response. Symptoms include sweating, faintness, difficulty concentrating, and altered levels of consciousness.
Diagnosis is confirmed through an oral glucose tolerance test or a gastric emptying scintigraphy study.
Post-Vagotomy Diarrhea
Post-vagotomy diarrhea is a common complication after vagotomy, characterized by frequent episodes of watery diarrhea. It can be attributed to changes in intestinal motility and bile secretion.
Gastric Stasis
Gastric stasis or delayed gastric emptying can occur due to disruption of normal gastric motility. Symptoms include nausea, vomiting, and a feeling of fullness. Diagnosis is confirmed through gastric emptying studies.
Bile Reflux Gastritis
Bile reflux gastritis is caused by the reflux of bile into the stomach, resulting in epigastric pain and bilious vomiting. Diagnosis can be confirmed through upper endoscopy and gastric pH monitoring.
Afferent and Efferent Loop Syndromes
Afferent loop syndrome occurs after Billroth II reconstruction and is characterized by abdominal pain, bilious vomiting, and distention. Efferent loop syndrome occurs when there is an obstruction of the efferent loop, leading to similar symptoms.
Roux Syndrome
Roux syndrome is a complication of Roux-en-Y procedures, characterized by postprandial abdominal pain and vomiting. Diagnosis is made through a contrast gastrointestinal transit study.
Therapeutic Approach
Management of post-gastrectomy syndromes includes dietary modifications, such as eating small frequent meals, separating liquids and solids, increasing protein and fat intake, and reducing simple sugars. In some cases, additional pharmacological or surgical interventions may be necessary. Understanding these syndromes and their therapeutic approaches is crucial to providing effective care and improving the quality of life for post-gastrectomy patients.
This article focuses on the small proportion of patients with severe, debilitating symptoms; these symptoms can challenge the acumen of the surgeon who is providing the patient’s long-term follow-up and care.
POSTGASTRECTOMY_SYNDROMES_REVIEW_ARTICLE
Complications of HEMORROIDH SURGERY
Symptomatic hemorrhoids require a number of therapeutic interventions each of which has its own complications. Office-based therapy such as rubber band ligation carries the risk of pain and bleeding, which are self-limited, but also carries the risk of rare complications such as sepsis, which may be life threatening. Operative treatment of hemorrhoids includes conventional hemorrhoidectomy, stapled hemorrhoidectomy, and the use of energy devices. Complications of pain and bleeding are common but self-limited. Late complications such as stenosis and fecal incontinence are rare. Recurrent disease is related to the initial grade and therapeutic approach. Treatment of recurrent hemorrhoids should be individualized based on previous treatments and the grade of disease. Anesthetic complications, especially urinary retention, are common and related to the anesthetic technique. Practitioners should council their patients as to the risks of the various approaches to treating symptomatic hemorrhoids.
Intra Abdominal Infections
With intra-abdominal infection being one of the most common reasons for surgical consultation, understanding the evaluation and management of these processes becomes paramount in the day- to-day practice of the surgeon. The very broad nature of who is affected coupled with the interplay of patient comorbidities and their medications make dealing with intra-abdominal infections a challenge. As with most complex problems in medicine, it is often useful to break them down into simpler and smaller parts. One useful way to categorize intra-abdominal infections is to divide them into those originating from previous abdominal trauma or operations and those presenting in a “virgin” abdomen.
The latter group most commonly includes those patients presenting with specific organ-based infectious processes such as appendicitis, cholecystitis, or diverticulitis. These individual diseases are covered extensively in other chapters and are discussed only superficially in this chapter. The former are those patients who have sustained intra-abdominal trauma or have undergone previous abdominal interventions and are not recovering in the usual expected course. It is this group that taxes diagnostic and clinical skills and may require the most complex medical decision making.
Several factors should come into play once suspicion for an intra-abdominal infection is entertained. These include resuscitation, antibiotic usage, and source control itself. Patients who present with either a suspected or diagnosed intra-abdominal infection should have some form of volume resuscitation. Even without hypotension, there are several reasons why these patients might be volume depleted. These include nausea and vomiting, fluid sequestration within the abdominal cavity or lumen of the bowel, and poor oral intake. As the process progresses, the patient may develop tachypnea, which results in an evaporative fluid loss. By this time, one can often elicit orthostatic hypotension in most patients.
Fluid resuscitation should begin with the administration of isotonic crystalloid and in general be guided by evidence of end organ perfusion (adequate mental status, urine output, correction of acidosis). There is no utility-using colloid such as albumin or hetastarch in these circumstances, and some data suggest a worse outcome. Should the patient present with hypotension or evidence of poor perfusion, a more aggressive approach to volume resuscitation should be employed. Our recommendation is to follow the current surviving sepsis guidelines, which include fluid challenges, monitoring/assessment of filling pressures, and the potential use of pressors and steroids.
KIDNEY INJURY on perioperative period
ACUTE KIDNEY FAILURE_REVIEW ARTICLE
Alterations in renal function are common after surgical emergencies, trauma, and major operations. In these settings, successful recovery of renal function is dependent on prompt diagnosis and protective management strategies. Acute kidney injury (AKI) is characterized by an acute decrease in glomerular filtration rate (GFR). The true incidence of AKI and acute renal failure (ARF) has been difficult to define, given the broad and various definitions used to quantify and study altered renal function. Relatively recent introduction of consensus definitions, such as RIFLE (risk, failure, loss, and end-stage renal failure) criteria and AKIN (Acute Kidney Injury Network) staging, have provided standard definitions to facilitate more uniform outcome reporting. With use of these definitions, recent studies suggest that AKI occurs in up to two thirds of patients in the intensive care unit (ICU). Moreover, increasing severity of AKI is associated with increasing mortality. AKI is also associated with increased morbidity, such as increased hospital length of stay and cost of care, and has been linked to other in-hospital complications, such as increased difficulty in weaning from mechanical ventilation. Preoperative risk factors for development of AKI include older age, emergent surgery, hepatic disease, obesity, high-risk surgery, vascular disease, and chronic obstructive pulmonary disease (COPD). Prompt recognition of AKI facilitates effective treatment. Although the incidence rate of AKI appears to be rising, overall outcomes from AKI are gradually improving.
The reported mortality rate of AKI is 30% to 60%. If RRT is necessary, reported mortality rates are over 50%. The reason for such high mortality is that AKI now usually occurs as part of a spectrum of multiple organ failure, most often associated with severe sepsis or septic shock. The mortality in this setting is often determined by the underlying septic syndrome, rather than by complications of individual organ failure. Of surviving patients of AKI, a significant number have development of chronic renal insufficiency, which necessitates chronic dialysis. The precise rate of development of chronic renal failure varies greatly in the literature, depending on the patient populations. A recent review of AKI estimates that overall, the risk of necessary chronic dialysis is approximately 12%.
Laparoscopic Surgery for Morbid Obesity
The morbid obesity epidemic continues to spread throughout industrialized nations. It is a condition with a heterogeneous etiology, including genetic, psychosocial, and environmental factors. Prevention methods have currently been unable to halt the further spread of this disease. Obesity has been linked to increased healthcare costs, common physiologic derangements, reduced quality of life, and increased overall mortality. More than one third of adults and almost 17% of children in the United States are obese.
Medical therapy that can cause sustained significant weight loss may be years away. Bariatric surgery, when combined with a multidisciplinary team, continues to be the only proven method to achieve sustained weight loss in most patients. Bariatric procedures modify gastrointestinal anatomy and, in some cases, enteric hormone release to reduce caloric intake, reduce absorption, and alter metabolism to achieve weight loss. Currently, the three most common bariatric operations in the United States are Roux-en-Y gastric bypass, adjustable gastric band, and the vertical sleeve gastrectomy.
GOSSIPIBOMA
O termo “gossipiboma” refere-se a uma matriz de matéria têxtil envolvida por reacção de corpo estranho. O termo é derivado do latim “Gossypium”, algodão, e o Swahili “boma”, que significa “esconderijo”. Também conhecida como textiloma, originada de “textilis” (tecer em latim) e “oma” (doença, tumor ou inchaço em grego). O primeiro caso foi descrito por Wilson em 1884. Gossipibomas foram relatados após operações em muitos processos, e em diferentes órgãos e localização. Mas, o local mais comum é o abdominal. Gaze e compressas são os materiais mais comumente retidos após laparotomia. A incidência de gossipibomas é variável e subnotificada, principalmente devido às implicações legais de sua detecção, mas também porque muitos pacientes permanecem assintomáticos. A apresentação clínica é também variável. O tratamento recomendado é a excisão que pretende evitar as complicações que conduzem a taxa de mortalidade entre11-35%.
Epidemiologia
Ele ocorre entre 1/1000 a 1/1500 nas operações intra-abdominais. A apresentação clínica é variável e depende da localização do corpo estranho e sobre o tipo de reação inflamatória apresentada pela hospedeiro. Podem existir formas agudas e crônicas. A forma aguda tende a apresentar-se com fístulas e abcessos cutâneos, enquanto que a crônica como massa encapsulada (granuloma de corpo estranho) e sintomas inespecíficos. Gossipibomas ocorrem mais comumente após operação abdominal e pélvica. Eles são mais frequentes em pacientes obesos e quando a operação é realizada em emergência. A incidência é maior em nove vezes após operação de emergência, e de quatro em procedimentos não planejados no decorrer de uma intervenção, mudando o que se pretendia realizar. Outros fatores predisponentes incluem operações em campo de batalha, complicações intra-operatórias, tais como perda intensa de sangue, a incapacidade de realizar contagem de materiais cirúrgicos no final do processo, tempo de operação prolongado e as mudanças no pessoal médico e de enfermagem durante o operação.
Evolução clínica
O tempo entre a operação e aparecimento de manifestações clínicas de Gossipiboma é variável, em particular se o material permanecer estéril. Ele depende da localização do material retido e do tipo de reação orgânica, e foi estimado em entre 10 dias a vários anos. Em patologia, duas reações de corpo estranho pode occorer. A primeira resposta é a produção asséptica de fibrina, o que leva à formação de aderências, material de encapsulamento e à formação de granulomas de corpo estranho. Nesta apresentação, o paciente pode permanecer assintomático por meses ou anos. A segunda resposta é exsudativa, com formação de abcessos, fístulas aos órgãos internos como o estômago, intestino, bexiga, cólon ou vagina, ou também fístula externa para a parede abdominal. Os sintomas dependem do órgão afetado principalmente e podem resultar da compressão, obstrução, síndrome de má absorção, ou crescimento bacteriano. Eles incluem dor abdominal, tumor palpável, náuseas, vômitos, sangramento retal, diarréia, disúria, piúria, hematúria e urgência urinária. Os sintomas sistêmicos como febre, anorexia, anemia e perda de peso também podem occurer. No entanto, a resposta inflamatória e aderências podem formar uma cápsula com o bloqueio omental e órgãos adjacentes, podendo o paciente permanecer assintomático. A falta de sintomas pode dificultar ou retardar o diagnóstico, que muitas vezes é realizado incidentalmente.
Possibilidades diagnósticas
O diagnóstico pode ser difícil. Suspeita clínica e o uso de estudos de imagem são importantes, pois é a regra a inexistência ou inespecificidade de sintomas em vários anos após a operação. No pré-operatório pode ser levantada suspeita por meio de estudos radiológicos ou endoscópicos. Muitos casos só são descobertos no intra-operatório. Tomografia computadorizada é o exame complementar de escolha para o diagnóstico e avaliação dessas complicações. Ele fornece informações detalhadas sobre a lesão na maioria dos casos. A aparência pode ser lesão cística espongiforme, cápsula hiperdensa em camadas concêntricas, ou calcificações murais. A presença de gás é indicativa de perfuração do intestino ou à formação de abcessos. Os principais diagnósticos diferenciais são: aderências pós-operatórias, fecalomas, contusões, hematomas, intussuscepção, volvo, tumores e abscessos intracavitários.
Tratamento e Prognóstico
O tratamento de escolha é a remoção cirúrgica que pode ser realizada por laparoscopia ou laparotomia, e visa prevenir complicações. O prognóstico da gossipiboma é variável com taxas de mortalidade de 11 para 35%. Quando a remoção ocorre no período pós-operatório imediato, a morbidade e mortalidade são baixas; no entanto, se o material foi mantido por um longo tempo a remoção pode exigir operação extensa e ter elevado índice de complicações.
Implicações médico-legais
Há muitas implicações médico-legais com gossypiboma. Revisão de negligência médica impetradas entre 1988 e 1994 revelou 40 casos de gossipiboma, que representaram 48% de todos os corpos estranhos. Não foi possível determinar se o material esquecimento representou falta de qualidade do cirurgião ou quadro de enfermagem.
Procedimentos preventivos
A abordagem mais importante é a prevenção. As medidas preventivas necessárias incluem o uso de material têxtil com marcadores radiopacos e contagem minuciosa de materiais cirúrgicos. São recomendadas quatro contagens: na montagem do material, antes da operação, no início do fechamento da cavidade e durante a síntese da pele. Dhillon e Park reforçam a importância da exploração dos quatro quadrantes abdominais no final da operação em todos os casos, mesmo após a contagem das compressas. No caso de contagem incorreta, a menos que o paciente seja considerado instável, a síntese da cavidade não deve ser realizada até que todas elas estejam localizados.
CONCLUSÃO
Gossipiboma é um problema médico-legal sério e sua incidência está aparentemente aumentando. Por isso, os meios e métodos nos procedimentos cirúrgicos durante o ato operatório e no contexto geral da sala de operações precisam ser revistos para tomarem-se medidas preventivas. Formação continuada de profissionais da área médica e estrita adesão à técnica operatória são primordiais para a prevenção de gossipiboma.
Abdominal Hernia Surgical EMERGENCIES
A hernia is a weakness or disruption of the fibromuscular tissues through which an internal organ (or part of the organ) protrudes or slides through. Collectively, inguinal and femoral hernias are often lumped together into groin hernias. Surgery remains the only effective treatment, but the optimal timing and method of repair remain controversial. Although strangulation rates of 3% at 3 months have been reported by some investigators, the largest prospective randomized trial of (watchful waiting) men with minimally symptomatic inguinal hernias showed that watchful waiting is safe. Frequency of strangulation was only 2.4% in patients followed up for as long as 11.5 years. Long-term follow-up shows that more than two-thirds of men using a strategy of watchful waiting cross over to surgical repair, with pain being the most common reasons. This risk of crossover is higher in patients older than 65 years. Once an inguinal hernia becomes symptomatic, surgical repair is clearly indicated. Femoral hernias are more likely to present with strangulation and require emergency surgery and are thus repaired even when asymptomatic. Because this article focuses on incarcerated hernias, nonoperative options are not discussed.
10 Princípios da RELAÇÃO CIRURGIÃO-PACIENTE


Quando a perspectiva de uma cirurgia surge, seja para corrigir uma condição médica, melhorar a estética ou simplesmente enfrentar uma situação inesperada, o medo e a apreensão são reações naturais. A visão de dor, complicações e a sensação de perda de controle podem ser opressoras, especialmente diante dos avanços tecnológicos prometidos pela medicina. No entanto, para enfrentar esses desafios de forma eficaz e justa, é crucial entender o processo cirúrgico e os papéis envolvidos. Aqui estão algumas orientações para pacientes e familiares, com base em princípios éticos e práticos da medicina moderna.
1. Relação Paciente-Cirurgião (ã): Construindo Confiança
A confiança mútua entre paciente e médico é fundamental. Evite se submeter a pressões para procedimentos rápidos e impessoais. Um relacionamento humanizado, onde o médico dedica tempo para entender o paciente, é essencial para evitar acusações injustas e frustrações. As consultas devem ser um espaço para esclarecimentos detalhados e empáticos, não apenas para realizar procedimentos.
2. Clareza e Transparência na Informação
Informações claras sobre o procedimento, suas consequências e riscos são essenciais. Evite jargões técnicos e explique cada aspecto da cirurgia em termos compreensíveis. A comunicação aberta reduz a ansiedade e prepara os pacientes para os possíveis desdobramentos da cirurgia.
3. Expectativas Realistas
Especialmente em procedimentos estéticos, alinhar as expectativas do paciente com a realidade é crucial. Muitas vezes, expectativas irreais podem levar a descontentamentos. É importante discutir de maneira honesta o que a cirurgia pode realmente alcançar e o que pode ser meramente aspiracional.
4. Avaliação Abrangente do Risco
O risco cirúrgico não se limita a aspectos cardíacos. Uma avaliação completa deve considerar todos os sistemas do corpo e a saúde mental do paciente. Exames físicos completos e, se necessário, avaliações psicológicas são partes vitais do pré-operatório.
5. O Papel do Anestesiologista
A escolha e a administração da anestesia são responsabilidades cruciais e devem ser discutidas com o anestesiologista. A decisão sobre o tipo de anestesia deve considerar as melhores práticas e o estado de saúde do paciente, não apenas a preferência do cirurgião.
6. Preparação para Possíveis Mudanças
A cirurgia pode trazer surpresas. É importante que o paciente esteja ciente de que o plano cirúrgico pode mudar com base nas condições encontradas durante o procedimento. Essas mudanças podem influenciar o tempo de recuperação e os custos envolvidos.
7. Documentação Completa
Preencher adequadamente o prontuário médico é crucial. Todos os detalhes, desde os exames realizados até os esclarecimentos fornecidos, devem estar documentados com precisão. Essa prática não apenas protege o paciente, mas também o profissional médico.
8. Comunicação Detalhada do Procedimento
Descreva minuciosamente o ato cirúrgico e os materiais encaminhados para análise. Certifique-se de que todos os procedimentos sejam seguidos corretamente e que todos os materiais estejam devidamente identificados.
9. Pós-Operatório: Acompanhamento e Cuidados
O acompanhamento pós-operatório deve ser meticuloso. Registre as datas e horários das visitas médicas e todas as providências tomadas. Forneça orientações claras sobre a alta e o acompanhamento ambulatorial.
10. Atenção ao Estado Emocional do Paciente
Pacientes com instabilidade emocional podem ter uma experiência mais difícil com a cirurgia. É vital que essas questões sejam abordadas com apoio especializado para garantir que o paciente esteja mentalmente preparado para o procedimento.
Conclusão
A ética na medicina, especialmente na cirurgia, vai além dos conceitos de eficiência técnica e competência. Trata-se de respeito mútuo e comunicação aberta entre médico e paciente. A prática médica ideal exige não apenas habilidades técnicas e conhecimento, mas também empatia, compreensão e um compromisso com a integridade e o bem-estar do paciente. Assim, com preparação cuidadosa e uma abordagem centrada no paciente, é possível enfrentar os desafios da cirurgia com confiança e esperança. Esta abordagem humanizada e informativa ajuda a construir uma relação de confiança, minimizando o medo e a ansiedade associados ao tratamento cirúrgico e garantindo que todos os aspectos do cuidado sejam geridos com a maior consideração e respeito.
The General Surgery Job Market

There is a current shortage of general surgeons nationwide. A growing elderly population and ongoing trends toward increased health care use have contributed to a higher demand for surgical services, without a corresponding increase in the supply of surgeons. The number of general surgeons per 100,000 people in the United States declined by 26% from the 1980s to 2005. Cumulative growth in demand for general surgery is projected to exceed 25% by 2025. The Association of American Medical Colleges has projected a shortage of 41,000 general surgeons by 2025. General surgeons make up 33% of the total projected physician shortage, the second highest after primary care physicians, who make up 37% of the total shortage. Despite the demand for general surgeons, the percentage of general surgery trainees going directly into practice is decreasing while the percentage of trainees pursuing subspecialty training is increasing. A recent study reported that graduating residents who lacked confidence in their skills to operate independently were more likely to pursue subspecialty training. This suggests that some graduating residents are motivated to obtain subspecialty training to gain more experience rather than narrow their clinical scope of practice. Given the projected shortage of general surgeons, this will be a crucial distinction when reforming surgical education. General surgery trainees interested in career planning would benefit from understanding the demand for general and/or specialty skills in a job market heavily influenced by a constant stream of new graduates. However, little is currently known about the demand for subspecialty vs general surgical skills in the current job market. The goal of this study was to describe the current job market for general surgeons in the United States, using Oregon and Wisconsin as surrogates. Furthermore, we sought to compare the skills required by the job market with those of graduating trainees with the goal of gaining insight that might assist in workforce planning and surgical education reform.
PRINCIPLES OF OSTOMY MANAGEMENT

The creation of a stoma is a technical exercise. Like most undertakings, if done correctly, the stoma will usually function well with minimal complications for the remainder of the ostomate’s life. Conversely, if created poorly, stoma complications are common and can lead to years of misery. Intestinal stomas are in fact enterocutaneous anastomoses and all the principles that apply to creation of any anastomosis (i.e., using healthy intestine, avoiding ischemia and undue tension) are important in stoma creation.
MOST COMMOM POSTOPERATIVE PROBLEMS
Despite good preoperative assessment, surgical and anaesthetic technique and perioperative management, unexpected symptoms or signs arise after operation that may herald a complication. Detecting these early by regular monitoring and surgical review means early treatment can often forestall major deterioration. Managing problems such as pain, fever or collapse requires correct diagnosis then early treatment. Determining the cause can be challenging, particularly if the patient is anxious, in pain or not fully recovered from anaesthesia. It is vital to see and assess the patient and if necessary, arrange investigations, whatever the hour, when deterio-ration suggests potentially serious but often remediable complications. Consider also whether and when to call for senior help.
Survival Guide for SURGERY ROUND

SURGERY ROUND
Medical students are often attached to the various services. They can provide a significant contribution to patient care. However, their work requires supervision by the surgical intern/resident who takes primary clinical responsibility. Subinterns are senior medical students who are seeking additional clinical experience. Their assistance is needed and appreciated, but again, close supervision of their clinical responsibilities by the intern/resident is mandatory.Outside reading is recommended, including textbooks, reference sources, and monthly journals.Eating is prohibited in patient care areas.Maintain patient confidentiality at all times.At conferences use only patient initials in presentations; and speak carefully and respectfully on work rounds.
PRINCIPLES
1. Always be punctual (this includes ward rounds, operating room, clinics, conferences, morbidity and mortality). Personal appearance is very important. Maintain a high standard including clean shirt and tie (or equivalent) and a clean white coat. The day begins early. Be ready with all the data to start rounds with the senior resident or chief resident. Be sure to provide enough time each morning to examine your patients before rounds.
ABOUT NOTES
2.Aim to get all of your chart notes written as soon as possible; this will greatly increase your effi ciency during the day. Sign and print your name, and include your beeper number, date, and time. Progress notes on patients are required daily. Surgical progress notes should be succinct and accurate, briefl y summarizing the patient’s clinical status and plan of management. Someone unfamiliar with the case should be able to get a good understanding of the patient’s condition from one or two notes. Operative consent is obtained after admitting the patient, performing the history and physical examination, discussing the risks, benefi ts, and alternatives of the procedure(s), and having the patient’s nurse sign the consent with the patient. If you are unaware of the risks and benefi ts of a procedure, discuss this with the service chief resident. Blood transfusion attestation forms need to be signed by the counseling physician before each surgical procedure.
OPERATING ROOM
3. Arrive in the operating room with the patient and before the attending physician or chief resident. Make sure that the charts and all of the relevant x-rays are in the operating room. Make sure that the x-rays are on the x-ray view box prior to the commencement of the case. The intern or resident performing the case should be familiar with the patient’s history and physical exam, current medications, and comorbidities, and be familiar with the principles of the operation prior to arriving in the operating room. Make it a habit to introduce yourself to the patient before the operation. It is mandatory that the surgical resident involved with a case in the operating room attend the start of the case punctually. Scheduled operative cases do not necessarily occur at the listed time. For this reason, it is necessary to check with the operating room front desk frequently. Do not rely on being paged. Conduct in the operating room includes assisting with the preoperative positioning and preparation of the patient; this includes shaving, catheterization, protection of pressure points, and thromboembolism protection. The resident should escort the patient from the operating room to the intensive care unit (ICU) or the postanesthetic care unit with the anesthesiologists. The operating surgeon is responsible for dictating the case. The resident must record all cases performed. For cases admitted to the surgery ICU, a hand-over to the surgery ICU resident is mandatory.This includes discussing all the preoperative assessment, operative details, and postoperative management of the case with the ICU resident.
ROUNDS
4. Signing out to cross-cover services must be performed in a meticulous and careful fashion. All patients should be discussed between the surgical intern and the cross-covering intern to cover all potential problems. A sign-out list containing all the patients, patient locations, and the responsible attendings should be given personally to the cross-cover intern. Any investigations performed at night (e.g., lab studies, chest x-ray, electrocardiogram [ECG]) should be checked that night by the covering intern. No test order should go unchecked. Abnormal lab values should be reviewed and discussed with the senior resident or the attending staff, especially on preoperative patients. Starting antibiotics should be a decision left to the senior resident or attending staff. If consultants are asked to see patients, their recommendations mustbe discussed with your senior resident or attending priorto initiating any new plans. Independent thought is good; independent action is bad.
SUPERVISION
5. Document all procedures performed on patients—including arterial lines, chest tubes, and central lines—with a short procedure note in the chart. Every patient contact should be documented in the patient record.If you see a patient in the middle of the night, write a short note to describe your assessment and plan. Remember, if there is no documentation, then nobody responded to the patient’s complaint or needs. Obtain appropriate supervision for procedures. There are always more senior residents available if your chief is not. Protect yourself; practice universal precautions! Wash your hands before and after examining a patient. Wear gloves. All wounds should be inspected every day by the surgical intern as part of the clinical examination. Please re-dress them; the nursing staff is not always immediately available to do so. There should never be any surprises in the morning.
RESIDENTS
Your senior resident is responsible for the service and should be kept aware of any problems, regardless of the time of day. If the senior resident is not available, the attending staff should be contacted directly. There are always senior residents in the hospital who are available to be used as resources for emergencies. Always be aware of who is in-house (i.e., consult resident, ICU resident, trauma chief). A surgery resident’s days are long. They start early and they fi nish late. Always remember the three A’s to being a successful resident: Affable, Available, and Able. Be prepared to maintain a flexible daily schedule depending on the workload of the service and the requirement for additional manpower.
PREVENTION COMPLICATIONS OF COLON SURGERY
COMPLICATIONS OF COLON SURGERY_REVIEW ARTICLE


Colon surgery represents a high number of patients treated at a department of gastrointestinal surgery and is not limited to colon cancer. It includes other non-neoplastic pathologies such as inflammatory bowel disease, diverticular disease or colonic volvulus. As with any major procedure, colon surgery patients may present serious or even fatal complications. The incidence of postoperative complications from colon surgery has been estimated at between 10% and 30% according to selected series. Preventive measures against surgical complications include selection of an appropriate procedure for the patient as well as good preoperative care, appropriate surgical technique and good postoperative management. When diagnosis has been established, risks for patient should be assessed according to patient’s health conditions and type of surgery accomplished. When the patient meets the surgical requirements, an appropriate course of preoperative care should be carried out including colon wash antibiotics and antithrombotic prophylaxis. Postoperative period will be equivalent to any major abdominal surgery. Typically, it was considered appropriate to wait a few days before initiating feeding in order to protect anastomosis; however, some authors agree that an early oral diet hours after intervention is not associated with a higher risk of anastomotic dehiscence and other complications.
Sleeve Gastrectomy: Complications and Management
SLEEVE GASTRECTOMY COMPLICATIONS_REVIEW ARTICLE
 Obesity is a common disease affecting adults and children. The incidence of obesity in worldwide is increasing. Laparoscopic sleeve gastrectomy (LSG) is a relatively new and effective procedure for weight loss. Owing to an increase in the number of bariatric surgical procedures, general surgeons should have an understanding of the complications associated with LSG and an approach for dealing with them. Early postoperative complications following LSG that need to be identified urgently include bleeding, staple line leak and development of an abscess. Delayed complications include strictures, nutritional deficiencies and gastresophageal reflux disease. We discuss the principles involved in the management of each complication.
Obesity is a common disease affecting adults and children. The incidence of obesity in worldwide is increasing. Laparoscopic sleeve gastrectomy (LSG) is a relatively new and effective procedure for weight loss. Owing to an increase in the number of bariatric surgical procedures, general surgeons should have an understanding of the complications associated with LSG and an approach for dealing with them. Early postoperative complications following LSG that need to be identified urgently include bleeding, staple line leak and development of an abscess. Delayed complications include strictures, nutritional deficiencies and gastresophageal reflux disease. We discuss the principles involved in the management of each complication.
“COMO PODEMOS CURAR A MEDICINA?”
“Nos últimos anos percebemos que estávamos na mais profunda crise da existência da medicina, devido a algo sobre o que você normalmente não pensa quando você é um médico preocupado em fazer o bem para as pessoas, que é o custo do tratamento de saúde. Não há um país no mundo que não esteja perguntando agora se podemos custear o que médicos fazem. A luta política que desenvolvemos tornou-se aquela sobre se o governo é o problema ou se as companhias de seguro são o problema. E a resposta é sim e não; é mais profundo que tudo isso. A causa de nossos problemas é, na verdade, a complexidade que a ciência nos deu. E para entender isso, voltarei algumas gerações…”
PERIOPERATIVE FLUID MANAGEMENT IN SURGERY
REVIEW ARTICLE_FLUID MANAGEMENT IN ELECTIVE SURGERY
The purpose of the thesis was to investigate the pathophysiology and functional outcomes of various fluid administration regimens in elective surgical procedures and describe factors of importance in perioperative fluid management. The goal was to create a rational physiologic background on which to design future ran-domized, clinical trials focusing on clinical outcomes aiming to produce evidence-based guidelines for rational perioperative fluid therapy. The main hypothesis of the thesis was thatthe ”liberal” fluid administration regimens seen in daily clinical practice may be detrimental and contribute to increased perioperative morbid-ity primarily due to increased functional demands of the cardi-opulmonary system and gastrointestinal tract as well as de-creased tissue oxygenation (impaired wound healing).
“CIRURGIA: PASSADO, PRESENTE e FUTURO ROBÓTICO”
A cirurgiã e inventora Catherine Mohr nos guia pela história da cirurgia (e seu passado pré-anestesia e pré-antissepsia), e depois demonstra algumas das mais novas ferramentas para cirurgias realizadas através de pequenas incisões, usando ágeis mãos robóticas.
Ebook: Princípios da Cirurgia Hepatobiliar

Cirurgia Hepatobiliar
Considera-se que a cirurgia hepática começou após o advento da anestesia e da anti-sepsia. No entanto, muito antes disso, diversos autores já relatavam suas experiências com ressecções do fígado. As primeiras descrições de “cirurgias hepáticas” consistiam no relato de avulsões parciais ou totais de porções do fígado após lesões traumáticas do abdome. O relato de Elliot (1897) exemplifica muito dos temores dos cirurgiões da época: “O fígado (…) é tão friável, tão cheio de vasos e tão evidentemente impossível de ser suturado que parece ser improvável o manejo bem sucedido de grandes lesões de seu parênquima”.
CIRURGIA HEPATOBILIAR_ASPECTOS BÁSICOS
Lymph Node Dissection in Gastric Adenocarcinoma
Extent of lymph node dissection has been an area of controversy in gastric adenocarcinoma for many years. Some surgeons believe that cancer metastasizes through a stepwise progression, and an extensive lymphadenectomy is necessary to improve survival and/or cure the patient. Other physicians argue that extensive ly-mphadenectomies only add pe-rioperative morbidity and mor-tality and do not improve survival. Asian countries have been performing extended lymphadenectomies routinely for many years with promising survival data, although Western countries have not been able to reproduce those results. Much of the controversy surrounding lymphadenectomies started in the 1980s when Japanese studies reported superior survival rates matched stage for stage, compared to the United States. This was theorized to be secondary to the more extensive lymphadenectomy performed in Japan compared to the United States.

A United Kingdom study randomized 400 patients to either a D1 or a D2 lymph node dissection. Those patients with tumors in the upper or middle third of the stomach underwent a distal pancreaticosplenectomy to obtain retropancreatic and splenic hilar nodes. While the 5-year survival rates were not statistically significant between the two groups, on multivariate analyses it was noted that those patients in the D2 group that did not undergo the distal pancreaticosplenectomy had an increased survival compared with the D1 group. A trial in the Netherlands randomized 380 gastric cancer patients to a D1 lymphadenectomy and 331 patients to a D2 lymphadenectomy. Similar to the United Kingdom study, there was not a significant difference in survival between the two groups, even when followed out to 11 years. There was a significant increase in postoperative complications in the D2 group compared with the D1 group (43 % vs. 25 %, respectively) as well as mortality (10 % vs. 4 %, respectively).
The data from these two studies suggest that a pancreaticosplenectomy performed to harvest lymph nodes seems to only add morbidity and mortality while not improving survival. One concern raised about the prior two studies was the variation in surgical technique and lack of standardization of surgeon experience. A Taiwanese study accounted for this by performing the study at a single institution with three surgeons, each of whom had completed at least 25 D3 lymph node dissections prior to the study. Patients with gastric cancer were randomized to a D1 lymph node dissection (defined as resection of perigastric lymph nodes along the lesser and greater curves of the stomach) or a D3 lymph node dissection (defined as resection of additional lymph nodes surrounding the splenic, common hepatic, left gastric arteries, nodes in the hepatoduodenal ligament, and retropancreatic lymph nodes). There was an overall 5-year survival benefit with the D3 group of 60 % compared with the D1 group of 54 %. A Japanese study evaluated a more aggressive lymph node dissection and randomized patients to a D2 dissection or a para-aortic lymph node dissection (PAND). There was no significant difference in 5-year survival between the two groups with a trend toward an increase in complications in the PAND group. Multiple studies have shown that the number of positive lymph nodes is a significant predictor of survival. Current AJCC guidelines stipulate that at least 15 lymph nodes are needed for pathologic examination to obtain adequate staging.
Laparoscopic techniques have become an integral part of surgical practice over the past several decades. For gastric cancer, multiple retrospective studies have reported the advantages of laparoscopic gastrectomy (LG) over open gastrectomy (OG). A recent meta-analysis of 15 nonrandomized comparative studies has also shown that although LG had a longer operative time than OG, it was associated with lower intraoperative blood loss, overall complication rate, fewer wound-related complications, quicker recovery of gastrointestinal motility with shorter time to first flatus and oral intake, and shorter hospital stay. A randomized prospective trial comparing laparoscopic assisted with open subtotal gastrectomy reported that LG had a significantly lower blood loss (229 ± 144 ml versus 391 ± 136 ml; P< 0.001), shorter time to resumption of oral intake (5.1 ± 0.5 days versus 7.4 ± 2 days; P< 0.001), and earlier discharge from hospital (10.3 ± 3.6 days versus 14.5 ± 4.6 days; P< 0.001).
Como funciona o GRAMPEADOR INTESTINAL ?
A Busca pela Segurança e Eficiência na Cirurgia Moderna
Introdução O objetivo primordial de qualquer cirurgião, ao iniciar uma intervenção, é garantir que o procedimento seja seguro e eficiente. A “regra de ouro” da cirurgia moderna permanece clara: o ato operatório deve ser o mais breve possível, gerando o menor trauma tecidual e restaurando a função do órgão. O resultado esperado é sempre a minimização das intercorrências no pós-operatório. Embora a cirurgia atual atinja esses objetivos de forma bastante satisfatória, as complicações relacionadas às suturas e à cicatrização ainda são desafios presentes na rotina hospitalar.
A Evolução Histórica e os Desafios da Cicatrização A confiabilidade das suturas gastrointestinais, por exemplo, é uma conquista relativamente recente. Foi apenas no final do século XIX que a compreensão dos princípios básicos da cicatrização tecidual permitiu avanços significativos nesta área. Sabemos hoje que o sucesso do reparo tecidual não depende apenas da técnica empregada, mas é uma equação complexa que envolve o paciente e a área operada. Diversos fatores podem retardar ou prejudicar drasticamente a cicatrização, entre eles:
-
Isquemia (falta de suprimento sanguíneo);
-
Edema (inchaço excessivo);
-
Infecção local ou sistêmica;
-
Desnutrição do paciente.
O Fator Humano e o Surgimento da Tecnologia Existe uma variável crítica na cirurgia: a habilidade manual. Naturalmente, há uma variação na destreza e na técnica entre diferentes cirurgiões. Foi justamente essa disparidade que motivou o desenvolvimento de novos dispositivos cirúrgicos. O objetivo da inovação tecnológica na cirurgia é superar as diferenças individuais, funcionando como um equalizador. Ao utilizar dispositivos que padronizam etapas críticas (como as suturas mecânicas), permite-se que técnicas complexas sejam executadas adequadamente, independente de quem opera.
Conclusão Para que a medicina avance, uma técnica não pode depender apenas do talento de poucos. Ela deve ser reproduzível de forma confiável pelo maior número possível de cirurgiões. Somente através dessa padronização e do auxílio tecnológico é que os resultados cirúrgicos podem ser amplamente adotados, reconhecidos como eficazes e, acima de tudo, seguros para o paciente.
POSTOPERATIVE ILEUS
POSTOPERATIVE ILEUS_REVIEW ARTICLE
 In systems that try to minimize hospital stay after abdominal surgery, one of the principal limiting factors is the recovery of adequate bowel function, which can delay discharge or lead to readmission. Postoperative ileus (POI) is the term given to the cessation of intestinal function following surgery. Although all surgical procedures put the patient at risk for POI, gastrointestinal tract surgeries in particular are associated with a temporary cessation of intestinal function. The duration of POI varies, lasting from a few hours to several weeks. Prolonged postoperative ileus, also known as pathologic postoperative ileus, can be caused by a myriad of pathologic processes that are treated with limited success by clinical and pharmacologic management. Studies of large administrative databases show that, on average, patients with a diagnosis of POI stay 5 days longer in hospital after abdominal surgery than patients without POI. Over the last decade, substantial efforts have been made to minimize the duration of POI, as there appears to be no associated physiologic benefit, and it is currently the primary factor delaying recovery for most patients. In this review, we define POI, describe the pathogenesis and briefly discuss clinical management before detailing current pharmacologic management options.
In systems that try to minimize hospital stay after abdominal surgery, one of the principal limiting factors is the recovery of adequate bowel function, which can delay discharge or lead to readmission. Postoperative ileus (POI) is the term given to the cessation of intestinal function following surgery. Although all surgical procedures put the patient at risk for POI, gastrointestinal tract surgeries in particular are associated with a temporary cessation of intestinal function. The duration of POI varies, lasting from a few hours to several weeks. Prolonged postoperative ileus, also known as pathologic postoperative ileus, can be caused by a myriad of pathologic processes that are treated with limited success by clinical and pharmacologic management. Studies of large administrative databases show that, on average, patients with a diagnosis of POI stay 5 days longer in hospital after abdominal surgery than patients without POI. Over the last decade, substantial efforts have been made to minimize the duration of POI, as there appears to be no associated physiologic benefit, and it is currently the primary factor delaying recovery for most patients. In this review, we define POI, describe the pathogenesis and briefly discuss clinical management before detailing current pharmacologic management options.
Colonoscopia : Quais as principais complicações?
Colonoscopy is a commonly performed procedure for the diagnosis and treatment of a wide range of conditions and symptoms and for the screening and surveillance of colorectal neoplasia. Although up to 33% of patients report at least one minor, transient GI symptom after colonoscopy, serious complications are uncommon. In a 2008 systematic review of 12 studies totaling 57,742 colonoscopies performed for average risk screening, the pooled overall serious adverse event rate was 2.8 per 1000 procedures. The risk of some complications may be higher if the colonoscopy is performed for an indication other than screening. The colorectal cancer miss rate of colonoscopy has been reported to be as high as 6% and the miss rate for adenomas larger than 1 cm is 12% to 17%. Although missed lesions are considered a poor outcome of colonoscopy, they are not a complication of the procedure per se and will not be discussed further in this document. Over 85% of the serious colonoscopy complications are reported in patients undergoing colonoscopy with polypectomy. An analysis of Canadian administrative data, including over 97,000 colonoscopies, found that polypectomy was associated with a 7-fold increase in the risk of bleeding or perforation. However, complication data are often not stratified by whether or not polypectomy was performed. Therefore, complications of polypectomy are discussed with those of diagnostic colonoscopy. A discussion of the diagnosis and management of all complications of colonoscopy is beyond the scope of this document, although general principles are reviewed.
Prontuário Médico | EVOLUÇÃO CIRÚRGICA S.O.A.P

INTRODUÇÃO
O prontuário médico é o conjunto de documentos padronizados e ordenados, onde devem ser registrados todos os cuidados profissionais prestados aos pacientes e que atesta o atendimento médico a uma pessoa numa instituição de assistência médica ou num consultório médico. É também o documento repositório do segredo médico do paciente. O preenchimento do prontuário médico é obrigação e responsabilidade intransferíveis do médico, fazendo-se exceção aos hospitais de ensino, onde alunos de medicina o fazem sob supervisão, correção e responsabilidade de médicos, sejam professores de medicina ou do staff do hospital de ensino. É prática antiética e ilegal, portanto condenável, delegar seu preenchimento a outrem que não médico habilitado perante o Conselho de Medicina. O prontuário médico corretamente preenchido é, e efetivamente tem sido, a principal peça de defesa do médico nos casos de denúncias por mal atendimento com indícios de imperícia, imprudência ou negligência, ou seja, na presunção da existência de erro médico. Este é o primeiro documento que a polícia, a Justiça e o próprio Conselho solicitam aos hospitais/médicos denunciados para apreciação dos fatos da denúncia.
ASPECTOS HISTÓRICOS
Na década de 1960, Lawrence Weed publicou um artigo (Weed LL. Medical records that guide and teach. N Engl J Med; 1968) que descreve um modelo de prontuário que é atualmente adotado em diversos centros médicos de todo o mundo. O modelo de Weed se destaca pela objetividade, organização, maior facilidade de acesso às informações para tomada de decisões e pela descrição sistemática das evidencias e das razões que apoiam as conclusões e os planos diagnósticos e terapêuticos durante o acompanhamento do paciente. O termo originalmente utilizado por Weed para o seu modelo de prontuário foi Prontuário Médico Orientado por Problemas (Problem-Oriented Medical Record).
No Brasil este modelo ficou conhecido como Prontuário Orientado por Problemas e Evidências (POPE) para destacar uma das características básicas deste modelo que é a ênfase nas evidências clínicas e científicas. No POPE as notas de evolução são orientadas pelos problemas ativos do paciente e segue o contexto descrito como SOAP. Cada letra da sigla SOAP se refere a um dos quatro aspectos fundamentais das notas de evolução diária, ou seja os dados subjetivos (S), os dados objetivos (O), a avaliação (A) e o planejamento (P).
COMO DEVE SER PREENCHIDO O PRONTUÁRIO NO SISTEMA S.O.A.P.?
No momento da realização das anotações o médico deverá identificar o paciente pelo nome e sobrenome, juntamente com a idade, a Clínica ao qual esta internado e o horário. Os itens de evolução médica são assim transcritos:
1. Os dados subjetivos (S) compreendem as queixas dos pacientes e outras informações fornecidas pelos pacientes, parentes ou acompanhantes.
2. Os dados objetivos (O) incluem os achados de exame físico e os achados de exames complementares.
3. A avaliação (A) se refere às conclusões sobre a situação do paciente, os pensamentos relativos ao diagnóstico e a resposta ao tratamento, tomando por base os achados subjetivos e objetivos.
4. Os planos (P) inclui os exames a serem solicitados visando o diagnóstico, as razões para inclusão, modificação de doses ou retirada de itens da terapêutica e as informações prestadas aos pacientes e familiares visando orientação e educação.
ASPECTOS ÉTICOS E LEGAIS
A “medicina de defesa” reforça a importância do prontuário e de seu preenchimento completo. O documento, para ser admitido em juízo como elemento de prova, necessita de ter sua autenticidade reconhecida, estar datado e assinado. A ausência desses elementos demonstra má qualidade da assistência prestada ao paciente. Rasuras comprometem o valor legal. Em casos de retificações, aconselha-se a escrever entre parênteses indicações como sem efeito, digo ou expressões análogas e, a seguir, escrever a correção.
Segundo o artigo 299 do Código Penal, a anotação incorreta, incompleta, falseada ou inexistente no prontuário quanto aos fatos relacionados com o paciente pode caracterizar falsidade ideológica: “Omitir, em documento público ou particular, declaração que dele devia constar ou nele inserir ou fazer inserir declaração falsa ou diversa da que devia ser escrita, com o fim de prejudicar direito, criar obrigação ou alterar a verdade sobre fato juridicamente relevante. Pena – reclusão de 1 (um) a 5 (cinco) anos, e multa, se o documento é público, e reclusão de 1 (um) ano a 3 (três) anos, e multa, se o documento é particular”. Se o agente for funcionário público e cometer o crime, prevalecendo-se do cargo, aumenta-se a pena de sexta parte.
Desta forma deverão constar em cada folha de evolução clínica do paciente as seguintes informações:
1. Identificação: Nome, idade e sexo; 2. Dias de Internação; 3. Diagnósticos (Sindrômico, Anatômico e Etiológico); 4. Terapêutica Básica; e 5.Data e hora de atendimento;
Os autores de todos os registros no prontuário deverão ser identificados através do nome completo e assinatura do profissional assistente com seu número de inscrição no respectivo conselho de classe. Recomenda-se SEMPRE USAR CARIMBO. Em caso de não-profissionais assistentes, como alunos em treinamento, é necessário que sua assinatura conste ao lado da do titular atendente.
A caligrafia faz parte da ética profissional do médico. As anotações precisam ser legíveis. “É vedado ao médico receitar ou atestar de forma secreta ou ilegível, assim como assinar em branco papeletas de receituários, laudos, atestados ou quaisquer outros documentos médicos” (artigo 39 do Código de Ética Médica). Nos prontuários em suporte de papel, é obrigatória a legibilidade da letra do profissional que atendeu o paciente (Resolução CFM n.º 1.638/02).
Laparoscopic Colorectal Surgery
With the introduction of laparoscopic colectomy nearly 20 years ago, a relatively slow adoption of laparoscopic colorectal surgery into surgical practice has taken place. It is estimated that 10% to 25% of all colorectal resections are performed utilizing laparoscopy. The persistent steep learning curve, the lack of high-volume colorectal surgery by general surgeons (who perform the bulk of colonic resection in the United States), and the modest advantages reported are but a few of the reasons that the percentage of laparoscopic colorectal procedures has not dramatically risen. With the publication of several large, prospective randomized trials for colon cancer, along with the interest in single-port surgery and natural orifice surgery, there appears to be a renewed interest in minimally invasive procedures for the colon and rectum. This chapter will provide an overview of these issues and offer a current assessment of the common diseases to which minimally invasive techniques have been applied.
Learning Curve
Numerous previous studies have evaluated the learning curve involved in laparoscopic colectomy. It is estimated by conventional laparoscopic techniques that the learning curve for laparoscopic colectomy is at least 20 cases but more likely 50 cases. The need to work in multiple quadrants of the abdomen, the need for a skilled laparoscopic assistant, and the lack of yearly volume has kept the learning curve relatively steep. The surgeon may also need to work in reverse angles to the camera. All of these combined add to the complexity of the procedure and result in the need to perform a number of cases before the surgeon and surgical team become proficient. More recent publications have suggested the learning curve is more than 20 cases. In a prospective randomized study of colorectal cancer in the United Kingdom, the CLASICC trial, surgeons had to perform at least 20 laparoscopic resections before they were allowed to enter the study. The study began in July 1996 and was completed in July 2002. Despite the surgeons’ prior experience, the rate of conversion dropped from 38% to 16% over the course of the study, suggesting that a minimum of 20 cases may not be enough to overcome the learning curve. In the COLOR trial from Europe, another prospective randomized study for colon cancer that required a prerequisite experience in laparoscopic colon resection before surgeons could enter patients in the study, surgeon and hospital volume were directly related to a number of operative and postoperative outcomes. The median operative time for high-volume hospitals (>10 cases/year) was 188 minutes, compared to 241 minutes for low-volume hospitals (<5 cases/year); likewise, conversion rates were 9% versus 24% for the two groups. High-volume groups also had more lymph nodes in the resected specimens, fewer complications, and shortened hospital stays. These two relatively recent multicenter studies suggest that the learning curve is clearly greater than 20 cases and that surgeons need to perform a minimum yearly number of procedures to maintain their skills.
Outcomes
There may not be another area in recent surgical history that has been more heavily scrutinized than laparoscopic colorectal surgery. The plethora of accumulated data allows a careful assessment of all outcome measures for nearly every colorectal disease and procedure. In comparison to conventional colorectal surgery, the benefits of laparoscopy for colorectal procedures compared to open techniques include a reduction in postoperative ileus, postoperative pain, and a concomitant reduction in the need for analgesics; an earlier tolerance of diet; a shortened hospital stay; a quicker resumption of normal activities; improved cosmesis; and possibly preservation of immune function. This is offset by a prolongation in operative time, the cost of laparoscopic equipment, and the learning curve for these technically challenging procedures. When reporting the outcomes of laparoscopic colectomy, a natural selection bias applies when comparing conventional and laparoscopic cases. The most complex cases are generally not suitable for a laparoscopic approach and therefore are performed via an open approach. Also, in many series the results of the successfully completed laparoscopic cases are compared to conventional cases, and the cases converted from a laparoscopic to a conventional procedure may be analyzed separately. Few studies, with the exception of the larger prospective randomized studies, leave the converted cases in the laparoscopic group as part of the “intention to treat” laparoscopic group. This clearly introduces selection bias.
Although the results of prospective randomized trials are available for almost every disease process requiring colorectal resection, the majority of studies of laparoscopic colectomy are retrospective case-control series or noncomparative reports. The conclusions regarding patient outcomes must therefore come from the repetitiveness of the results rather than the superiority of the study design. For any one study, the evidence may be weak; but collectively, because of the reproducibility of results by a large number of institutions, even with different operative techniques and postoperative management parameters, the preponderance of evidence favors a minimally invasive approach with respect to postoperative outcomes.
Operative Time
Nearly all the comparative studies provide information regarding operative times. The definition of the operative time may vary with each series, and there may be different groups of surgeons performing the laparoscopic and conventional procedures. With the exception of a few reports, nearly all studies demonstrated a prolonged operative time associated with laparoscopic procedures. In prospective randomized trials, the procedure was roughly 40 to 60 minutes longer in the laparoscopic groups. As the surgeon and team gain experience with laparoscopic colectomy, the operating times do reliably fall, but rarely do they return to the comparable time for a conventional approach.
Return of Bowel Activity and Resumption of Diet
Reduction in postoperative ileus is one of the proposed major advantages of minimally invasive surgery. Nearly all of the retrospective and prospective studies comparing open and laparoscopic colectomy have shown a statistically significant reduction in the time to passage of flatus and stool. Most series demonstrate a 1- to 2-day advantage for the laparoscopic group. Whether the reduction of ileus relates to less bowel manipulation or less intestinal exposure to air during minimally invasive surgery remains unknown. With the reduction in postoperative ileus, the tolerance by the patient of both liquids and solid foods is quicker following laparoscopic resection. The time to resumption of diet varies from 2 days to 7 days, but in the majority of comparative studies, this is still 1 to 2 days sooner than in patients undergoing conventional surgery. Again, the physician and patient were not blinded in nearly all studies, which may have altered patient expectations. However, the overwhelming reproducible data reported in both retrospective and prospective studies of laparoscopic procedures does likely favor a reduction of postoperative ileus and tolerance of liquid and solid diets.
Postoperative Pain
To measure postoperative pain, a variety of assessments have been performed to demonstrate a significant reduction in pain following minimally invasive surgery; some studies utilize an analog pain scale, and others measure narcotic requirements. Physician bias and psychologic conditioning of patients may interfere with the evaluation of postoperative pain. There are also cultural variations in the response to pain. Three of the early prospective randomized trials have evaluated pain postoperatively, and all three have found a reduction in narcotic requirements in patients undergoing laparoscopic colectomy. In the COST study, the need both for intravenous and oral analgesics was less in patients undergoing successfully completed laparoscopic resections. Numerous other nonrandomized studies have shown a reduction in postoperative pain and narcotic usage.
Length of Stay
The quicker resolution of ileus, earlier resumption of diet, and reduced postoperative pain has resulted in a shortened length of stay for patients after laparoscopic resection when compared to traditional procedures. Recovery after conventional surgery has also been shortened, but in the absence of minimally invasive techniques, it would seem unlikely that the length of stay could be further reduced. In nearly all comparative studies, the length of hospitalization was 1 to 6 days less for the laparoscopic group. Although psychological conditioning of the patient cannot be helped and likely has a desirable effect, the benefits of minimally invasive procedures on the overall length of stay cannot be discounted. The benefit, however, is more likely a 1 to 2 day advantage only. The more recent introduction of clinical pathways, both in conventional and laparoscopic surgery, has also narrowed the gap but appears to be more reliable in patients undergoing a minimally invasive approach.
Hospital Costs
One of the disadvantages of laparoscopy is the higher cost related to longer operative times and increased expenditures in disposable equipment. Whether the total cost of the hospitalization (operative and hospital costs) is higher following laparoscopic colectomy is debatable. A case-control study from the Mayo Clinic looked at total costs following laparoscopic and open ileocolic resection for Crohn’s disease (CD). In this study, 66 patients underwent laparoscopic or conventional ileocolic resection and were well matched. Patients in the laparoscopic group had less postoperative pain, tolerated a regular diet 1 to 2 days sooner, and had a shorter length of stay (4 vs. 7 days). In the cost analysis, despite higher operative costs, the overall mean cost was $3273 less in the laparoscopic group. The procedures were performed by different groups of surgeons at the institution, and although the surgeons may have introduced biases, this study was undertaken during the current era of cost containment, in which all physicians are encouraged to reduce hospital stays. The results are similar for elective sigmoid diverticular resection with a mean cost savings of $700 to $800. Clearly, if operative times and equipment expenditure are minimized, the overall cost of a laparoscopic resection should not exceed a conventional approach.
Tratamento Laparoscópica da DIVERTICULITE AGUDA
O aumento da prevalência de doença diverticular fez o seu adequado manuseio mais um assunto de debate constante. Especialmente para os casos de diverticulite, progresso considerável tem sido feito em termos de diagnóstico e tratamento. Diagnóstico apropriado em TC e técnicas intervencionistas são agora amplamente disponíveis, bem como agentes antimicrobianos eficazes. Finalmente, como a ressecção cirúrgica do cólon envolvido é a única maneira de erradicar definitivamente essa condição, a colectomia eletiva laparoscópica surgiu como uma opção segura e interessante entre as opções de tratamento. Embora tenha sido recentemente contestada sobre a sua progressão, a história natural da diverticulite é assumida como sendo a de recorrência ao longo do tempo, pelo menos, em um terço dos pacientes. O medo das complicações desta doença benigna e prevalente tem motivado sociedades médicas e cirúrgicas para produzir orientações e consensos sobre o assunto. A mortalidade geralmente vem de sepse recorrente e/ou operações de emergência para casos mais complicados. Como resultado, o procedimento cirúrgico mais realizado, a sigmoidectomia eletiva, é normalmente indicada para todos os casos complicados e muitos dos não-complicados. A abordagem laparoscópica para a colectomia esquerda tem evoluído e condições seguras são oferecidas aos pacientes, quando realizado por cirurgiões experientes em laparoscopia.






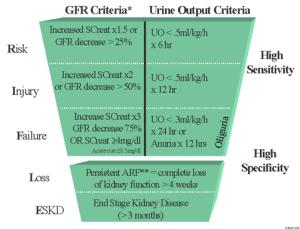




 The risk of complications and mortality in bariatric surgery is associated with certain factors that are common to other patients and procedures, including age above 65 years, the presence of associated diseases (cardiovascular and pulmonary disease, chronic renal failure, liver cirrhosis, etc.), prior abdominal surgery, and the experience of the surgeon and the institution, especially concerning the ability to make an early diagnosis and address complications. The surgical complications observed in the early postoperative period following surgeries performed to treat severe obesity are similar to those associated with other major surgeries of the gastrointestinal tract. However, given the more frequent occurrence of medical comorbidities (such as diabetes, arterial hypertension, and sleep apnea), as well as the difficulty in making an early diagnosis of the complications (due to limitations of the clinical abdominal workup and imaging methods, such as ultrasonography and computed tomography, particularly in highly obese patients with body mass indices >50 kg/m²), these patients require special attention in the early post operative follow-up. Pulmonary thromboembolism, a complication associated with bariatric surgery, also requires greater attention from the medical team given the high mortality rate associated with this condition. Early diagnosis and appropriate treatment of these complications are directly associated with a greater probability of control.
The risk of complications and mortality in bariatric surgery is associated with certain factors that are common to other patients and procedures, including age above 65 years, the presence of associated diseases (cardiovascular and pulmonary disease, chronic renal failure, liver cirrhosis, etc.), prior abdominal surgery, and the experience of the surgeon and the institution, especially concerning the ability to make an early diagnosis and address complications. The surgical complications observed in the early postoperative period following surgeries performed to treat severe obesity are similar to those associated with other major surgeries of the gastrointestinal tract. However, given the more frequent occurrence of medical comorbidities (such as diabetes, arterial hypertension, and sleep apnea), as well as the difficulty in making an early diagnosis of the complications (due to limitations of the clinical abdominal workup and imaging methods, such as ultrasonography and computed tomography, particularly in highly obese patients with body mass indices >50 kg/m²), these patients require special attention in the early post operative follow-up. Pulmonary thromboembolism, a complication associated with bariatric surgery, also requires greater attention from the medical team given the high mortality rate associated with this condition. Early diagnosis and appropriate treatment of these complications are directly associated with a greater probability of control.