Surgeons and Performance
SURGEONS ARE HIGH PERFORMANCE ATHLETES
In a 2011 New Yorker article, Dr. Atul Gawande explored the idea that surgeons should consider a performance coach. Like athletes, he reasons, surgeons rely on complex physical movements to achieve their goals. Guidance and refinement by a trained eye could improve their performance.
Surgical coaching is a controversial topic (one which colleagues and I are actively investigating). But in the years following Dr. Gawande’s article, this idea opened the door to a broader concept: the “surgeon athlete.” An “athlete” is one whose performance depends on a carefully choreographed interplay between mind and body: heightened focus and anticipation along with quick decision-making and coordination. Combined with the reliance on teamwork and requisite stamina, this is wholly within the job description of a surgeon. Many surgeons are likely to find this concept silly. But our profession has imprudently encouraged surgical trainees to disregard the critical fine-tuning of their minds and bodies. We demand perfection, stamina, and encyclopedic knowledge, while discouraging the healthy habits that improve performance. Ironically, the sports world is more advanced in applying science to their training. And by ignoring this indisputable science, we are really hurting our patients. Because in order to best take care of them, we need to first take care of ourselves.
Hepatic Surgery: Portal Vein Embolization

INTRODUCTION
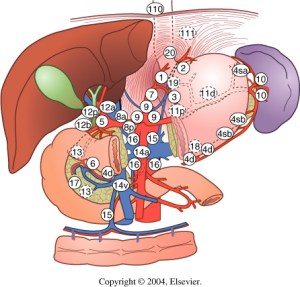
Portal vein Embolizations (PVE) is commonly used in the patients requiring extensive liver resection but have insufficient Future Liver Remanescent (FLR) volume on preoperative testing. The procedure involves occluding portal venous flow to the side of the liver with the lesion thereby redirecting portal flow to the contralateral side, in an attempt to cause hypertrophy and increase the volume of the FLR prior to hepatectomy.
PVE was first described by Kinoshita and later reported by Makuuchi as a technique to facilitate hepatic resection of hilar cholangiocarcinoma. The technique is now widely used by surgeons all over the world to optimize FLR volume before major liver resections.
PHYSIOPATHOLOGY
PVE works because the extrahepatic factors that induce liver hypertrophy are carried primarily by the portal vein and not the hepatic artery. The increase in FLR size seen after PVE is due to both clonal expansion and cellular hypertrophy, and the extent of post-embolization liver growth is generally proportional to the degree of portal flow diversion. The mechanism of liver regeneration after PVE is a complex phenomenon and is not fully understood. Although the exact trigger of liver regeneration remains unknown, several studies have identified periportal inflammation in the embolized liver as an important predictor of liver regeneration.

THECNICAL ASPECTS
PVE is technically feasible in 99% of the patients with low risk of complications. Studies have shown the FLR to increase by a median of 40–62% after a median of 34–37 days after PVE, and 72.2–80% of the patients are able to undergo resection as planned. It is generally indicated for patients being considered for right or extended right hepatectomy in the setting of a relatively small FLR. It is rarely required before extended left hepatectomy or left trisectionectomy, since the right posterior section (segments 6 and 7) comprises about 30% of total liver volume.
PVE is usually performed through percutaneous transhepatic access to the portal venous system, but there is considerable variability in technique between centers. The access route can be ipsilateral (portal access at the same side being resected) with retrograde embolization or contralateral (portal access through FLR) with antegrade embolization. The type of approach selected depends on a number of factors including operator preference, anatomic variability, type of resection planned, extent of embolization, and type of embolic agent used. Many authors prefer ipsilateral approach especially for right-sided tumors as this technique allows easy catheterization of segment 4 branches when they must be embolized and also minimizes the theoretic risk of injuring the FLR vasculature or bile ducts through a contralateral approach and potentially making a patient ineligible for surgery.
However, majority of the studies on contralateral PVE show it to be a safe technique with low complication rate. Di Stefano et al. reported a large series of contralateral PVE in 188 patients and described 12 complications (6.4%) only 6 of which could be related to access route and none precluded liver resection. Site of portal vein access can also change depending on the choice of embolic material selected which can include glue, Gelfoam, n-butyl-cyanoacrylate (NBC), different types and sizes of beads, alcohol, and nitinol plus. All agents have similar efficacy and there are no official recommendations for a particular type of agent.
RESULTS
Proponents of PVE believe that there should be very little or no tumor progression during the 4–6 week wait period for regeneration after PVE. Rapid growth of the FLR can be expected within the first 3–4 weeks after PVE and can continue till 6–8 weeks. Results from multiple studies suggest that 8–30% hypertrophy over 2–6 weeks can be expected with slower rates in cirrhotic patients. Most studies comparing outcomes after major hepatectomy with and without preoperative PVE report superior outcomes with PVE. Farges et al. demonstrated significantly less risk of postoperative complications, duration of intensive care unit, and hospital stay in patients with cirrhosis who underwent right hepatectomy after PVE compared to those who did not have preoperative PVE. The authors also reported no benefit of PVE in patients with a normal liver and FLR >30%. Abulkhir et al. reported results from a meta-analysis of 1088 patients undergoing PVE and showed a markedly lower incidence of Post Hepatectomy Liver Failure (PHLF) and death compared to series reporting outcomes after major hepatectomy in patients who did not undergo PVE. All patients had FLR volume increase, and 85% went on to have liver resection after PVE with a PHLF incidence of 2.5% and a surgical mortality of 0.8%. Several studies looking at the effect of systemic neoadjuvant chemotherapy on the degree of hypertrophy after PVE show no significant impact on liver regeneration and growth.
VOLUMETRIC RESPONSE

The volumetric response to PVE is also a very important factor in understanding the regenerative capacity of a patient’s liver and when used together with FLR volume can help identify patients at risk of poor postsurgical outcome. Ribero et al. demonstrated that the risk of PHLF was significantly higher not only in patients with FLR ≤ 20% but also in patients with normal liver who demonstrated ≤5% of FLR hypertrophy after PVE. The authors concluded that the degree of hypertrophy >10% in patients with severe underlying liver disease and >5% in patients with normal liver predicts a low risk of PHLF and post-resection mortality. Many authors do not routinely offer resection to patients with borderline FLR who demonstrate ≤5% hypertrophy after PVE.
Predicting LIVER REMNANT Function
Careful analysis of outcome based on liver remnant volume stratified by underlying liver disease has led to recommendations regarding the safe limits of resection. The liver remnant to be left after resection is termed the future liver remnant (FLR). For patients with normal underlying liver, complications, extended hospital stay, admission to the intensive care unit, and hepatic insufficiency are rare when the standardized FLR is >20% of the TLV. For patients with tumor-related cholestasis or marked underlying liver disease, a 40% liver remnant is necessary to avoid cholestasis, fluid retention, and liver failure. Among patients who have been treated with preoperative systemic chemotherapy for more than 12 weeks, FLR >30% reduces the rate of postoperative liver insufficiency and subsequent mortality.
When the liver remnant is normal or has only mild disease, the volume of liver remnant can be measured directly and accurately with threedimensional computed tomography (CT) volumetry. However, inaccuracy may arise because the liver to be resected is often diseased, particularly in patients with cirrhosis or biliary obstruction. When multiple or large tumors occupy a large volume of the liver to be resected, subtracting tumor volumes from liver volume further decreases accuracy of CT volumetry. The calculated TLV, which has been derived from the association between body surface area (BSA) and liver size, provides a standard estimate of the TLV. The following formula is used:
TLV (cm3) = –794.41 + 1267.28 × BSA (square meters)
Thus, the standardized FLR (sFLR) volume calculation uses the measured FLR volume from CT volumetry as the numerator and the calculated TLV as the denominator: Standardized FLR (sFLR) = measured FLR volume/TLV Calculating the standardized TLV corrects the actual liver volume to the individual patient’s size and provides an individualized estimate of that patient’s postresection liver function. In the event of an inadequate FLR prior to major hepatectomy, preoperative liver preparation may include portal vein embolization (PVE).
Classroom: Principles of Hepatic Surgery
Surgical Management of Cholangiocarcinoma
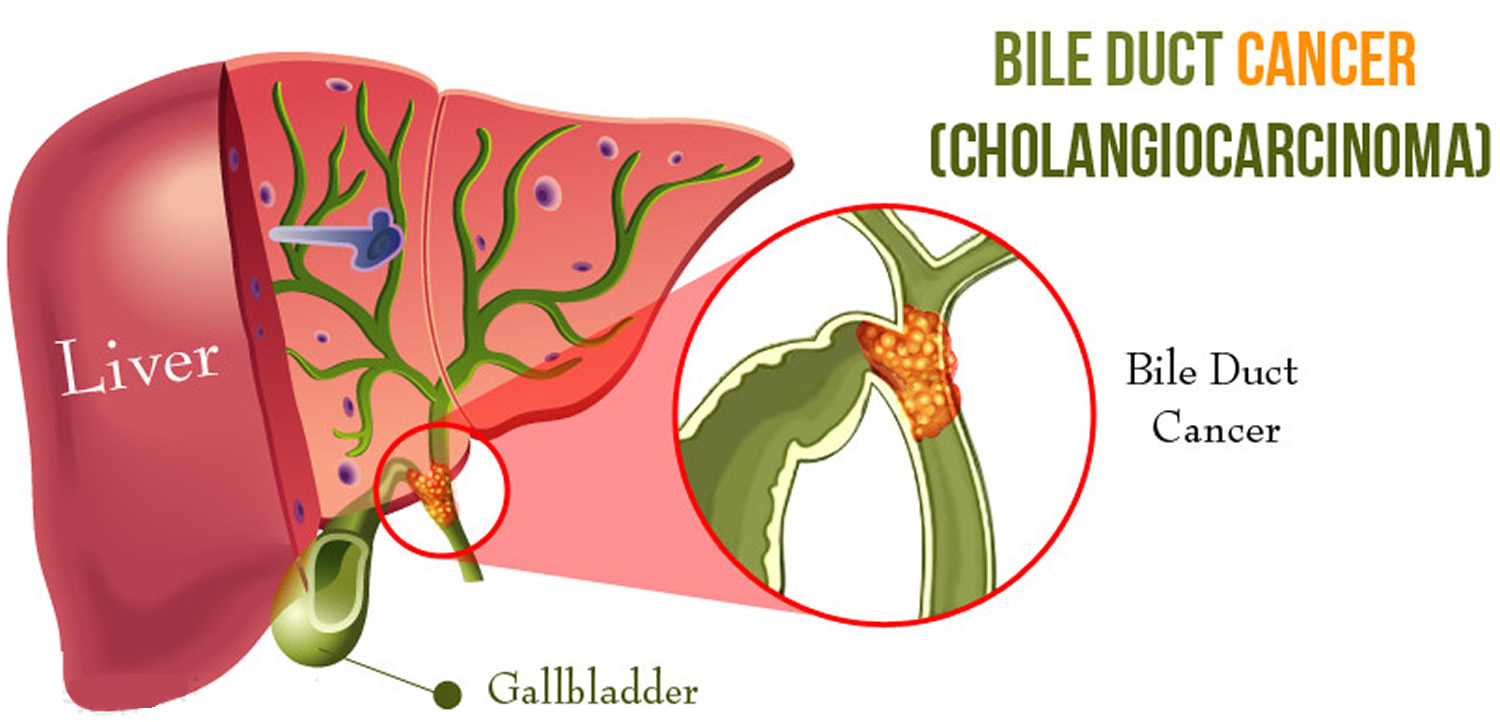
Cholangiocarcinoma (CCA) is a rare but lethal cancer arising from the bile duct epithelium. As a whole, CCA accounts for approximately 3 % of all gastrointestinal cancers. It is an aggressive disease with a high mortality rate. Unfortunately, a significant proportion of patients with CCA present with either unresectable or metastatic disease. In a retrospective review of 225 patients with hilar cholangiocarcinoma, Jarnagin et al. reported that 29 % of patients had either unresectable disease were unfit for surgery. Curative resection offers the best chance for longterm survival. Whereas palliation with surgical bypass was once the preferred surgical procedure even for resectable disease, aggressive surgical resection is now the standard.
Classroom: Surgical Management of Cholangiocarcinoma
Minimally Invasive Approach to Choledocholithiasis
Introduction
The incidence of choledocholithiasis in patients undergoing cholecystectomy is estimated to be 10 %. The presence of common bile duct stones is associated with several known complications including cholangitis, gallstone pancreatitis, obstructive jaundice, and hepatic abscess. Making the diagnosis early and prompt management is crucial. Traditionally, when choledocholithiasis is identified with intraoperative cholangiography during the cholecystectomy, it has been managed surgically by open choledochotomy and place- ment of a T-tube. This open surgical approach has a morbidity rate of 10–15 %, mortality rate of <1 %, with a <6 % incidence of retained stones. Patients who fail endoscopic retrieval of CBD stones, as well as cases in which an endoscopic approach is not appropriate, should be explored surgically.
Clinical Manifestation
Acute obstruction of the bile duct by a stone causes a rapid distension of the biliary tree and activation of local pain fibers. Pain is the most common presenting symptom for choledocholithiasis and is localized to either the right upper quadrant or to the epigastrium. The obstruction will also cause bile stasis which is a risk factor for bacterial over- growth. The bacteria may originate from the duodenum or the stone itself. The combination of biliary obstruction and colo- nization of the biliary tree will lead to the development of fevers, the second most common presenting symptom of cho- ledocholithiasis. Biliary obstruction, if unrelieved, will lead to jaundice. When these three symptoms (pain, fever, and jaundice) are found simultaneously, it is known as Charcot’s triad. This triad suggests the diagnosis of acute ascending cholangitis, a potentially life-threatening condition. If not treated promptly, this can lead to hypotension and decreased metal status, both signs of severe sepsis. When combined with Charcot’s triad, this constellation of symptoms is commonly referred to as Reynolds pentad.
Laparoscopic common bile duct exploration
Laparoscopic common bile duct exploration (LCBDE) allows for single stage treatment of gallstone disease, reducing overall hospital stay, improving safety and cost-effectiveness when compared to the two-stage approach of ERCP and laparoscopic cholecystectomy. Bile duct clearance can be confirmed by direct visualization with a choledochoscope. But, before the advent of choledochoscope, bile duct clearance was uncertain, and blind instrumentation of the duct resulted in accentuated edema and inflammation. Due to advancement in instruments, optical magnification, and direct visualization, laparoscopic exploration of the CBD results in fewer traumas to the bile duct. This has led to an increasing tendency to close the duct primarily, reducing the need for placement of T-tubes. Still, laparoscopic bile duct exploration is being done in only a few centers. Apart from the need for special instruments, there is also a significant learning curve to acquire expertise to be able to perform a laparoscopic bile duct surgery.
Morbidity and mortality rates of laparoscopic exploration are comparable to ERCP (2–17 and 1–5 %), and there is no clear difference in primary success rates between the two approaches. However, the endoscopic approach may be preferable for elderly and frail patients, who are at higher risk with surgery. Patients older than 70–80 years of age have a 4–10 % mortality rate with open duct exploration. It may be as high as 20 % in elderly patients undergoing urgent procedures. In comparison, advanced age and comor- bidities do not have a significant impact on overall complication rates for ERCP. A success rate of over 90 % has been reported with laparoscopic CBD exploration. Availability of surgical expertise and appropriate equipment affect the success rate of laparoscopic exploration, as does the size, number of the CBD stones, as well as biliary anatomy. Over the years, laparoscopic exploration has become efficient, safe, and cost effective. Complications include CBD laceration, stricture formation, bile leak, abscess, pancreatitis, and retained stones.
In cases of failure of laparoscopic CBD exploration, a guidewire or stent can be passed through the cystic duct, common bile duct, and through the ampulla into the duodenum followed by cholecystectomy. This makes the identification and cannulation of the ampulla easier during the post- operative ERCP. Laparoscopic common bile duct exploration is traditionally performed through a transcystic or transductal approach. The transcystic approach is appropriate under certain circumstances. These include a small stone (<10 mm) located in the CBD, presence of small common bile duct (<6 mm), or if there is poor access to the common duct. The transductal approach is preferable in cases of large stones, stones in proximal ducts (hepatic ducts), large occluding stones in a large duct, presence of multiple stones, or if the cystic duct is small (<4 mm) or tortuous. Contraindications for laparoscopic approach include lack of training, and severe inflammation in the porta hepatis making the exploration difficult and risky.
Key Points
With advancement in imaging technology, laparoscopic and endoscopic techniques, management of common bile duct stone has changed drasti- cally in recent years. This has made the treatment of this condition safe and more efficient. Many options are now available to manage this condition, and any particular modality for treatment should be chosen carefully based on the patient related factors, institutional protocol, available expertise, resources, and cost-effectiveness.
Classroom: M.I.A. of Choledocholithiasis
IPMN Surgical Management

INTRODUCTION
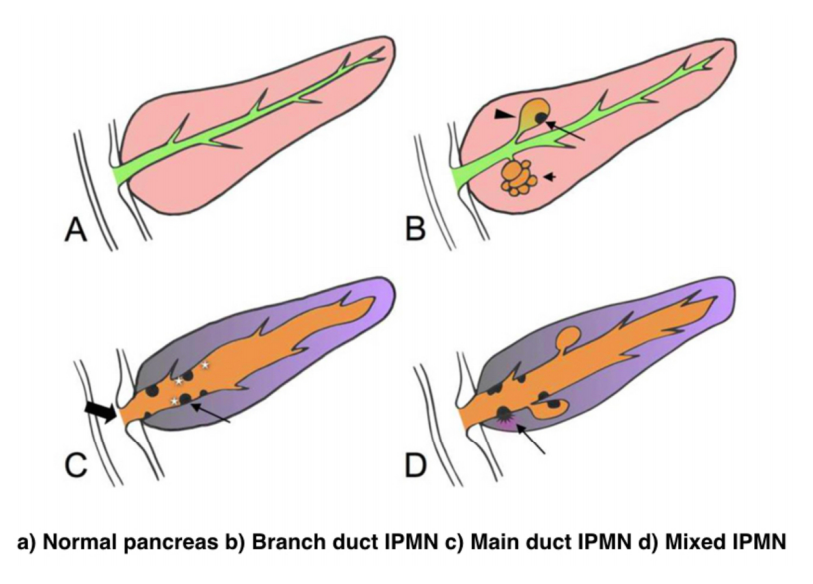
IPMNs were first recognized in 1982 by Ohashi, but the term IPMN was not officially used until 1993. IPMNs are defined in the WHO Classification of Tumors of the Digestive System as an intraductal, grossly visible epithelial neoplasm of mucin-producing cells. Using imaging and histology, IPMNs can be classified into three types based on duct involvement:
1. Main-duct IPMN (approximately 25% of IPMNs): Segmental or diffuse dilation of the main pancreatic duct (>5 mm) in the absence of other causes of ductal obstruction.
2. Branch-duct IPMN (approximately 57% of IPMNs): Pancreatic cysts (>5 mm) that communicate with the main pancreatic duct.
3. Mixed type IPMN (approximately 18% of IPMNs): Meets criteria for both main and branch duct.
Due to the asymptomatic nature of the disease, the overall incidence of IPMNs is difficult to define but is thought to account for approximately 3% to 5% of all pancreatic tumors. Most IPMNs are discovered as incidental lesions from the workup of an unrelated process by imaging or endoscopy. IPMNs are slightly more prevalent in males than in females, with a peak incidence of 60 to 70 years of age. Branch-duct IPMNs tend to occur in a slightly younger population and are less associated with malignancy compared with main-duct or mixed variants.
Because a majority of IPMNs are discovered incidentally, most are asymptomatic. When symptoms do occur, they tend to be nonspecific and include unexplained weight loss, anorexia, abdominal pain, and back pain. Jaundice can occur with mucin obstructing the ampulla or with an underlying invasive carcinoma. The obstruction of the pancreatic duct can also lead to pancreatitis. IPMNs may represent genomic instability of the entire pancreas. This concept, known as a “field defect,” has been described as a theoretical risk of developing a recurrent IPMN or pancreatic adenocarcinoma at a site remote from the original IPMN. The three different types of IPMNs, main duct, branch duct, and mixed duct, dictate different treatment algorithms.
MAIN DUCT IPMNs
Main-duct IPMNs should be resected in all patients unless the risks of existing comorbidities outweigh the benefits of resection. The goal of operative management of IPMNs is to remove all adenomatous or potentially malignant epithelium to minimize recurrence in the pancreas remnant. There are two theories on the pathophysiologic basis of IPMNs. The first groups IPMNs into a similar category as an adenocarcinoma, a localized process involving only a particular segment of the pancreas. The thought is that removal of the IPMN is the only treatment necessary. In contrast, some believe IPMNs to represent a field defect of the pancreas. All of the ductal epithelium remains at risk of malignant degeneration despite removal of the cyst. Ideally, a total pancreatectomy would eliminate all risk, but this is a radical procedure that is associated with metabolic derangements and exocrine insufficiency. Total pancreatectomy should be limited to the most fit patients, with a thorough preoperative assessment and proper risk stratification prior to undertaking this surgery.
There is less uncertainty with treatment of main-duct IPMNs. The high incidence of underlying malignancy associated with the IPMNs warrants surgical resection. IPMNs localized to the body and tail (approximately 33%) can undergo a distal pancreatectomy with splenectomy. At the time of surgery, a frozen section of the proximal margin should be interpreted by a pathologist to rule out high-grade dysplasia. A prospective study identified a concordance rate of 94% between frozen section and final pathologic examination. If the margin is positive (high-grade dysplasia, invasion) additional margins may be resected from the pancreas until no evidence of disease is present. However, most surgeons will proceed to a total pancreatectomy after two subsequent margins demonstrate malignant changes. This more extensive procedure should be discussed with the patient prior to surgery, and the patient should be properly consented regarding the risks of a total pancreatectomy.
IPMNs localized to the head or uncinate process of the pancreas should undergo a pancreaticoduodenectomy. A frozen section of the distal margin should be analyzed by pathology for evidence of disease. As mentioned before, after two additional margins reveal malignant changes, a total pancreatectomy is usually indicated (approximately 5%). The absence of abnormal changes in frozen sections does not equate to negative disease throughout the pancreas remnant. Rather, skip lesions involving the remainder of the pancreas can exist and thus patients ultimately still require imaging surveillance after successful resection. A prophylactic total pancreatectomy is rarely performed because the subsequent pancreatic endocrine (diabetes mellitus) and exocrine deficits (malnutrition) carry an increased morbidity.
BRANCH DUCT IPMNs
Localized branch-duct IPMN can be treated with a formal anatomic pancreatectomy, pancreaticoduodenectomy, or distal pancreatectomy, depending on the location of the lesion. However, guidelines were established that allow for nonoperative management with certain branch- type IPMN characteristics.
These include asymptomatic patients with a cyst size less than 3 cm and lack of mural nodules. The data to support this demonstrate a very low incidence of malignancy (approximately 2%) in this patient group. Which nearly matches the anticipated mortality of undergoing a formal anatomic resection. In approximately 20% to 30% of patients with branch- duct IPMNs, there is evidence of multifocality. The additional IPMNs can be visualized on high-resolution CT or MRI imaging. Ideally, patients with multifocal branch-duct IPMNs should undergo a total pancreatectomy. However, as previously mentioned, the increased morbidity and lifestyle alterations associated with a total pancreatectomy allows for a more conservative approach. This would include removing the most suspicious or dominant of the lesions in an anatomic resection and follow-up imaging surveillance of the remaining pancreas remnant. If subsequent imaging demonstrates malignant charac- teristics, a completion pancreatectomy is usually indicated.
RECURRENCE RATES
Recurrence rates with IPMNs are variable. An anatomic resection of a branch-duct IPMN with negative margins has been shown to be curative. The recurrence of a main- duct IPMN in the remnant gland is anywhere from 0% to 10% if the margins are negative and there is no evidence of invasion. Most case series cite a 5-year survival rate of at least 70% after resection of noninvasive IPMNs. In contrast, evidence of invasive disease, despite negative margins, decreases 5-year survival to 30% to 50%. The recurrence rate in either the pancreatic remnant or distant sites approaches 50% to 90% in these patients. Histopathologic subtype of the IPMN is correlated with survival. The aggressive tubular subtype has a 5-year survival ranging from 37% to 55% following surgical resection, whereas the colloid subtype has 5-year survival ranging from 61% to 87% post resection. Factors associated with decreased survival include tubular subtype, lymph node metastases, vascular invasion, and positive margins. IPMNs with evidence of invasion should be treated similar to pancreatic adenocarcinomas. Studies show that IPMNs tend to have better survival than pancreatic adenocarcinoma. This survival benefit may be secondary to the less aggressive tumor biology or the earlier diagnosis of IPMNs.
SURVEILLANCE
All patients who have a resected IPMN should undergo imaging surveillance. There is continual survival benefit with further resection if an IPMN does recur. International Consensus Guidelines published in 2017 offer recom- mendations for the frequency and modality of imaging surveillance after resection. Routine serum measurement of CEA and CA 19-9 has a limited role for detection of an IPMN recurrence. Of note, a new pancreatic lesion discovered on imaging after resection could represent a postoperative pseudocyst, a recurrence of the IPMN from inadequate resection, a new IPMN, or an unrelated new neoplastic process. IPMNs may also be associated with extrapancreatic neoplasms (stomach, colon, rectum, lung, breast) and pancreatic ductal adenocarcinoma. It is unclear if this represents a true genetic syndrome. However, patients with IPMNs should have a discussion about the implications of their disease with their physician and are encouraged to undergo colonoscopy to exclude a synchronous neoplastic process.
The incidence of PANCREATIC CYSTIC LESIONS will continue to increase as imaging technology improves. EUS, cytology, and molecular panels have made differentiating the type of PCN less problematic. The importance of an accurate preoperative diagnosis ensures that operative management is selectively offered to those with high-risk lesions. Management beyond surgery, including adjuvant therapy and surveillance, continue to be active areas of research.
Hepatocellular Carcinoma: Resection Versus Transplantation

Hepatocellular carcinoma is the second most common cause of cancer mortality worldwide and its incidence is rising in North America, with an estimated 35,000 cases in the U.S. in 2014. The best chance for cure is surgical resection in the form of either segmental removal or whole organ transplantation although recent survival data on radiofrequency ablation approximates surgical resection and could be placed under the new moniker of “thermal resection”. The debate between surgical resection and transplantation focuses on patients with “within Milan criteria” tumors, single tumors, and well compensated cirrhosis who can safely undergo either procedure. Although transplantation historically has had better survival outcomes, early diagnosis, reversal of liver disease, and innovations in patient selection and neo-adjuvant therapies have led to similar 5-year survival. Transplantation clearly has less risk of tumor recurrence but exposes recipients to long term immunosuppression and its side effects. Liver transplantation is also limited by the severe global limit on the supply of organ donors whereas resection is readily available. The current data does not favor one treatment over the other for patients with minimal or no portal hypertension and normal synthetic function. Instead, the decision to resect or transplant for HCC relies on multiple factors including tumor characteristics, biology, geography, co-morbidities, location, organ availability, social support and practice preference.
Resection Versus Transplantation
The debate between resection and transplantation revolves around patients who have well compensated cirrhosis with Milan criteria resectable tumors. Patients within these criteria represent a very small proportion of those who initially present with HCC. This is especially true in western countries where hepatitis C is the most common cause of liver failure and HCC is a result of the progressive and in most cases advanced cirrhosis.
Given the need for a large number of patients to show statistical significance, it would be difficult to perform a high-quality prospective randomized controlled trial comparing resection and transplantation. In fact the literature revealed that no randomized controlled trials addressing this issue exist. Instead, outcomes of surgical treatment for HCC stem from retrospective analyses that have inherent detection, selection and attrition biases.
Given the numerous articles available on this subject, several meta-analyses have been published to delineate the role of transplantation and resection for treatment of HCC. However, there is reason to be wary of these meta-analyses because they pool data from heterogeneous populations with variable selection criteria and treatment protocols. One such meta-analysis by Dhir et al. focused their choice of articles to strict criteria which excluded studies with non-cirrhotic patients, fibrolamellar HCC and hepato-cholangiocarcinomas but included those with HCC within Milan criteria and computation of 5-year survival; between 1990 and 2011 they identified ten articles that fit within these criteria, of which six were ITT analyses, six included only well-compensated cirrhotics (Child-Pugh Class A without liver dysfunction) and three were ITT analyses of well-compensated cirrhotics.
Analysis of the six ITT studies that included all cirrhotics (n = 1118) (Child-Pugh Class A through C) showed no significant difference in survival at 5 years (OR = 0.600, 95 % CI 0.291– 1.237 l; p=0.166) but ITT analysis of only well-compensated cirrhotics (Child- Pugh Class A) revealed that patients undergoing transplant had a significantly higher 5-year survival as compared to those with resection (OR=0.521, 95 % CI 0.298–0.911; p=0.022).
A more recent ITT retrospective analysis from Spain assessed long-term survival and tumor recurrence following resection or transplant for tumors <5 cm in 217 cirrhotics (Child-Pugh Class A, B and C) over the span of 16 years. Recurrence at 5 years was significantly higher in the resection group (71.6 % vs. 16 % p<0.001) but survival at 4 years was similar (60 % vs. 62 %) which is likely explained by the evolving role of adjuvant therapies to treat post-resection recurrence.
Conclusions
- Patients with anatomically resectable single tumors and no cirrhosis or Child-Pugh Class A cirrhosis with normal bilirubin, HVPG (<10 mmHg), albumin and INR can be offered resection (evidence quality moderate; strong recommendation).
- Patients with Milan criteria tumors in the setting of Child- Pugh Class A with low platelets and either low albumin or high bilirubin or Child-Pugh Class B and C cirrhosis, especially those with more than one tumor, should be offered liver transplantation over resection (evidence quality moderate; strong recommendation).
- Those with Milan criteria tumors and Child-Pugh Class A cirrhosis without liver dysfunction should be considered for transplantation over resection (evidence quality low; weak recommendation).
- No recommendation can be made in regard to transplanting tumors beyond Milan criteria (evidence quality low) except to follow regional review board criteria.
- Pre-transplant therapies such as embolic or thermal ablation are safe and by expert opinion considered to be effective in decreasing transplant waitlist dropout and bridging patients to transplant (evidence quality low, weak recommendation). These interventions should be considered for those waiting longer than 6 months (evi- dence quality low, moderate recommendation).
- Living donor liver transplantation is a safe and effective option for treatment of HCC that are within and exceed Milan criteria (evidence quality moderate, weak recommendation).
The century of THE SURGEONS
Surgery is a profession defined by its authority to cure by means of bodily invasion. The brutality and risks of opening a living person’s body have long been apparent, the benefits only slowly and haltingly worked out. Nonetheless, over the past two centuries, surgery has become radically more effective, and its violence substantially reduced — changes that have proved central to the development of mankind’s abilities to heal the sick.
Consider, for instance, amputation of the leg.
The procedure had long been recognized as lifesaving, in particular for compound fractures and other wounds prone to sepsis, and at the same time horrific. Before the discovery of anesthesia, orderlies pinned the patient down while an assistant exerted pressure on the femoral artery or applied a tourniquet on the upper thigh.
Surgeons using the circular method proceeded through the limb in layers, taking a long curved knife in a circle through the skin first, then, a few inches higher up, through the muscle, and finally, with the assistant retracting the muscle to expose the bone a few inches higher still, taking an amputation saw smoothly through the bone so as not to leave splintered protrusions. Surgeons using the flap method, popularized by the British surgeon Robert Liston, stabbed through the skin and muscle close to the bone and cut swiftly through at an oblique angle on one side so as to leave a flap covering the stump.
The limits of patients’ tolerance for pain forced surgeons to choose slashing speed over precision. With either the flap method or the circular method, amputation could be accomplished in less than a minute, though the subsequent ligation of the severed blood vessels and suturing of the muscle and skin over the stump sometimes required 20 or 30 minutes when performed by less experienced surgeons.
No matter how swiftly the amputation was performed, however, the suffering that patients experienced was terrible. Few were able to put it into words. Among those who did was Professor George Wilson. In 1843, he underwent a Syme amputation — ankle disarticulation — performed by the great surgeon James Syme himself. Four years later, when opponents of anesthetic agents attempted to dismiss them as “needless luxuries,” Wilson felt obliged to pen a description of his experience:
“The horror of great darkness, and the sense of desertion by God and man, bordering close on despair, which swept through my mind and overwhelmed my heart, I can never forget, however gladly I would do so. During the operation, in spite of the pain it occasioned, my senses were preternaturally acute, as I have been told they generally are in patients in such circumstances. I still recall with unwelcome vividness the spreading out of the instruments: the twisting of the tourniquet: the first incision: the fingering of the sawed bone: the sponge pressed on the flap: the tying of the blood-vessels: the stitching of the skin: the bloody dismembered limb lying on the floor.”
It would take a little while for surgeons to discover that the use of anesthesia allowed them time to be meticulous. Despite the advantages of anesthesia, Liston, like many other surgeons, proceeded in his usual lightning-quick and bloody way. Spectators in the operating-theater gallery would still get out their pocket watches to time him. The butler’s operation, for instance, took an astonishing 25 seconds from incision to wound closure. (Liston operated so fast that he once accidentally amputated an assistant’s fingers along with a patient’s leg, according to Hollingham. The patient and the assistant both died of sepsis, and a spectator reportedly died of shock, resulting in the only known procedure with a 300% mortality.)
The Surgical Personality

Surgical stereotypes are remnants of the days of pre-anaesthesia surgery and include impulsivity, narcissism, authoritativeness, decisiveness, and thinking hierarchically. Medical students hold these stereotypes of surgeons early in their medical training. As Pearl Katz says in the The Scalpel’s Edge: ‘Each generation perpetuates the culture and passes it on by recruiting surgical residents who appear to resemble them and training these residents to emulate their thinking and behaviour.’ The culture of surgery has evolved, and certain behaviours are rightly no longer seen as acceptable, Non-technical skills such as leadership and communication have become incorporated into surgical training. Wen Shen, Associate Professor of Clinical Surgery at University of California San Francisco, argues that this has gone too far: ‘Putting likeability before surgical outcomes is like judging a restaurant by the waiters and ignoring the food,’ I would argue that operative and communication skills are indivisible, An aggressive surgeon is a threat to patient safety if colleagues are frightened to speak up for fear of a colleague shouting or, worse, throwing instruments. Conversely, a flattened hierarchy promotes patient safety.
Read More
Article: The Surgical Personality
The “GOOD” Surgeon
Surgery is an extremely enjoyable, intellectually demanding and satisfying career, and many more people apply to become surgeons each year than there are available places.
Those who are successful have to be ready not just to learn a great deal, but have the right kind of personality for the job.
Is a surgical career right for you?
Read the link…
THE GOOD SURGEON

Modern Concepts of Pancreatic Surgery
 Operations on the gallbladder and bile ducts are among the surgical procedures most commonly performed by general surgeons. In most hospitals, cholecystectomy is the most frequently performed operation within the abdomen. Pancreatic surgery is less frequent , but because of the close relation between the biliary system and the pancreas, knowledge of pancreatic problems is equally essential to the surgeon. Acute and chronic pancreatitis and cancer of the pancreas are often encountered by surgeons, with apparently increasing frequency; their treatment remains difficult and perplexing. This review demonstrates the modern aspects of pancreatic surgery. Good study.
Operations on the gallbladder and bile ducts are among the surgical procedures most commonly performed by general surgeons. In most hospitals, cholecystectomy is the most frequently performed operation within the abdomen. Pancreatic surgery is less frequent , but because of the close relation between the biliary system and the pancreas, knowledge of pancreatic problems is equally essential to the surgeon. Acute and chronic pancreatitis and cancer of the pancreas are often encountered by surgeons, with apparently increasing frequency; their treatment remains difficult and perplexing. This review demonstrates the modern aspects of pancreatic surgery. Good study.
AULA: PRÍNCIPIOS MODERNOS DA CIRURGIA PANCREÁTICA
Palestras e Vídeoaulas

Vejam nos links a seguir algumas de nossas palestras disponíveis para download no Canal do SlideShare e Videoaulas presentes no You Tube.
Postoperative Delirium

Postoperative delirium is recognized as the most common surgical complication in older adults,occurring in 5% to 50% of older patients after an operation. With more than one-third of all inpatient operations in the United States being performed on patients 65 years or older, it is imperative that clinicians caring for surgical patients understand optimal delirium care. Delirium is a serious complication for older adults because an episode of delirium can initiate a cascade of deleterious clinical events, including other major postoperative complications, prolonged hospitalization, loss of functional independence, reduced cognitive function, and death. The annual cost of delirium in the United States is estimated to be $150 billion. Delirium is particularly compelling as a quality improvement target, because it is preventable in up to 40% of patients; therefore, it is an ideal candidate for preventive interventions targeted to improve the outcomes of older adults in the perioperative setting. Delirium diagnosis and treatment are essential components of optimal surgical care of older adults, yet the topic of delirium is under-represented in surgical teaching.
Postoperative Delirium in Older Adults
Surgical treatment of ACUTE PANCREATITIS
Acute pancreatitis is more of a range of diseases than it is a single pathologic entity. Its clinical manifestations range from mild, perhaps even subclinical, symptoms to a life-threatening or life-ending process. The classification of acute pancreatitis and its forms are discussed in fuller detail by Sarr and colleagues elsewhere in this issue. For the purposes of this discussion, the focus is on the operative interventions for acute pancreatitis and its attendant disorders. The most important thing to consider when contemplating operative management for acute pancreatitis is that we do not operate as much for the acute inflammatory process as for the complications that may arise from inflammation of the pancreas. In brieSurgical treatment of acute pancreatitisf, the complications are related to: necrosis of the parenchyma, infection of the pancreas or surrounding tissue, failure of pancreatic juice to safely find its way to the lumen of the alimentary tract, erosion into vascular or other structures, and a persistent systemic inflammatory state. The operations may be divided into three major categories: those designed to ameliorate the emergent problems associated with the ongoing inflammatory state, those designed to ameliorate chronic sequelae of an inflammatory event, and those designed to prevent a subsequent episode of acute pancreatitis. This article provides a review of the above.
SURGICAL TREATMENT OF ACUTE PANCREATITIS
O TEMPLO DO CIRURGIÃO.
Templo (do latim templum, “local sagrado”) é uma estrutura arquitetônica dedicada ao serviço religioso. O termo também pode ser usado em sentido figurado. Neste sentido, é o reflexo do mundo divino, a habitação de Deus sobre a terra, o lugar da Presença Real. É o resumo do macrocosmo e também a imagem do microcosmo: ‘o corpo é o templo do Espírito Santo’ (I, Coríntios, 6, 19).
Dos locais especiais, O corpo humano (morada da alma), a Cavidade Peritoneal e o Bloco Cirúrgico, se bem analisados, são muito semelhantes e merecem atitudes e comportamentos respeitáveis. O Templo, em todos os credos, induz à meditação, absoluto silêncio tentando ouvir o Ser Supremo. A cavidade peritoneal | abdominal , espaço imaculado da homeostase, quando injuriada, reage gritando em dor, implorando uma precoce e efetiva ação terapêutica.
O Bloco Cirúrgico, abrigo momentâneo do indivíduo solitário, que mudo e quase morto de medo, recorre à prece implorando a troca do acidente, da complicação, da recorrência, da seqüela, da mutilação, da iatrogenia e do risco de óbito pela agressiva e controlada intervenção que lhe restaure a saúde, patrimônio magno de todo ser vivo.
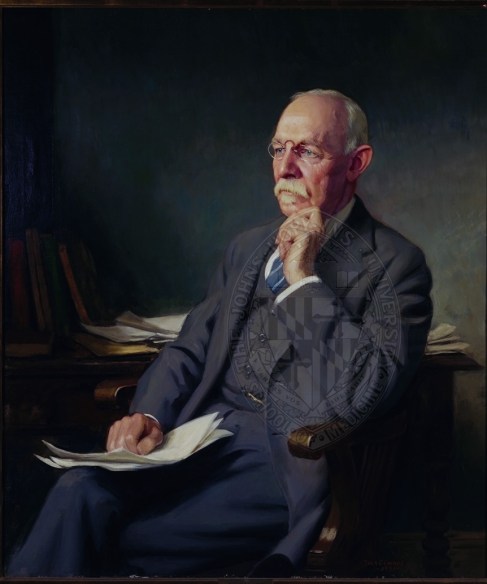
O Bloco Cirúrgico clama por respeito ao paciente cirúrgico, antes mesmo de ser tomado por local banal, misturando condutas vulgares, atitudes menores, desvio de comportamento e propósitos secundários. Trabalhar no Bloco Cirúrgico significa buscar a perfeição técnica, revivendo os ensinamentos de William Stewart Halsted , precursor da arte de operar, dissecando para facilitar, pinçando e ligando um vaso sangüíneo, removendo tecido macerado, evitando corpos estranhos e reduzindo espaço vazio, numa síntese feita com a ansiedade e vontade da primeira e a necessidade e experiência da última.
Mas, se a cirurgia e o cirurgião vêm sofrendo grande evolução, técnica a primeira e científica o segundo, desde o início do século, a imagem que todo doente faz persiste numa simbiose entre mitos e verdades. A cirurgia significa enfrentar ambiente desconhecido chamado “sala de cirurgia” onde a fobia ganha espaço rumo ao infinito. O medo ainda prepondera em muitos.
A confiança neste momento além de um reconhecimento é um troféu que o cirurgião recebe dos pacientes e seus familiares. Tanto a CONFIANÇA quanto a SEGURANÇA têm que ser preservadas a qualquer custo. Não podem correr o risco de serem corroídas por palavras e atitudes de qualquer membro da equipe cirúrgica. Não foi tarefa fácil transformar, para a população, o ato cirúrgico numa atividade científica, indispensável, útil e por demais segura. Da conquista da cirurgia, como excelente arma terapêutica para a manutenção de um alto padrão de qualidade técnica, resta a responsabilidade dos cirurgiões, os herdeiros do suor e sangue, que se iniciou com o trabalho desenvolvido por Billroth, Lister, Halsted, Moyniham, Kocher e uma legião de figuras humanas dignas do maior respeito, admiração e gratidão universal.
No ato operatório os pacientes SÃO TODOS SEMELHANTES EM SUAS DIFERENÇAS, desde a afecção, ao prognóstico, ao caráter da cirurgia e especialmente sua relação com o ato operatório. Logo, o cirurgião tem por dever de ofício entrar no bloco cirúrgico com esperança e não deve sair com dúvida. Nosso trabalho é de equipe, cada um contribui com uma parcela, maior ou menor, para a concretização do todo, do ato cirúrgico por completo, com muita dedicação, profissionalismo e sabedoria. Toda tarefa, da limpeza do chão ao ato de operar, num crescendo, se faz em função de cada um e em benefício da maioria, o mais perfeito possível e de uma só vez, quase sempre sem oportunidade de repetição e previsão de término.
O trabalho do CIRURGIÃO é feito com carinho, muita dignidade, humildade e executado em função da alegria do resultado obtido aliado a dimensão ética do dever cumprido que transcende a sua existência. A vida do cirurgião se materializa no ato operatório e o bloco cirúrgico, palco do nosso trabalho não tolera e jamais permite atitudes menores, inferiores, ambas prejudiciais a todos os pacientes e a cada cirurgião. Como ambiente de trabalho de uma equipe diversificada, precisamos manter, a todo custo, o controle de qualidade, eficiência, eficácia e efetividade técnina associados aos mais altos valores ético, pois lidamos com o que há de mais precioso da criação divina na Terra: O SER HUMANO.
“Tem presença de Deus, como já a tens. Ontem estive com um doente, um doente a quem quero com todo o meu coração de Pai, e compreendo o grande trabalho sacerdotal que os médicos levam a cabo. Mas não se ponham orgulhosos, porque todas as almas são sacerdotais. Devem pôr em prática esse sacerdócio! Ao lavares as mãos, ao vestires a bata, ao calçares as luvas, pensa em Deus, e pensa nesse sacerdócio real de que fala São Pedro, e então não se te meterá a rotina: farás bem aos corpos e às almas” São Josemaria Escriva
Bariatric Complications

Over the past decade, following the publication of several long-term outcome studies that showed a significant improvement in cardiovascular risk and mortality after bariatric surgery, the number of bariatric procedures being carried out annually in the UK has grown exponentially. Surgery remains the only way to produce significant, sustainable weight loss and resolution of comorbidities. Nevertheless, relatively few surgeons have developed an interest in this field. Most bariatric surgery is now performed in centres staffed by surgeons with a bariatric interest, usually as part of a multidisciplinary team.
The commonest weight loss procedures performed around the world at present are the gastric band, the gastric bypass and the sleeve gastrectomy. In very obese patients, an alternative operation is the duodenal switch, while the new ileal transposition procedure represents one of the few purely metabolic operations designed specifically for the treatment of type II diabetes. Older operations such as vertical banded gastroplasty and jejuno-ileal bypass are now obsolete, although patients who have undergone such procedures in the distant past may still present to hospital with complications. The main endoscopic option at present is insertion of a gastric balloon, with newer procedures like the endoscopic duodenojejunal barrier and gastric plication on the horizon. Implantable neuroregulatory devices (gastric ‘pacemakers’) represent a new direction for surgical weight control by harnessing neural feedback signals to help control eating.
It should be within the capability of any abdominal surgeon to manage the general complications of bariatric surgery, which include pulmonary atelectasis/pneumonia, intra-abdominal bleeding, anastomotic or staple-line leak with or without abscess formation, deep vein thrombosis (DVT)/pulmonary embolus and superficial wound infections. Patients may be expected to present with malaise, pallor, features of sepsis or obvious wound problems. However, clinical features may be difficult to recognise owing to body habitus. Abdominal distension, tenderness and guarding may be impossible to determine clinically due to the patient’s obesity. Pallor is non-specific. Fever and leucocytosis may be absent. Wound collections may be very deep. These complications in a bariatric patient should be actively sought with appropriate investigations. In particular, it is vital for life-threatening complications such as bleeding, sepsis and bowel obstruction to be recognised promptly and treated appropriately. A persistent tachycardia may be the only sign heralding significant complications and should always be taken seriously. It is useful to classify complications as ‘early’, ‘medium’ and ‘late’ because, from the receiving clinician’s point of view, the differential diagnosis will differ accordingly.
Complications of bariatric surgery presenting to the GENERAL SURGEON
A “PROFISSÃO” CIRÚRGICA
 “A arte de curar vem do coração e da mente mais do que das mãos.” – Hipócrates
“A arte de curar vem do coração e da mente mais do que das mãos.” – Hipócrates
Na complexa tapeçaria da sociedade moderna, as profissões desempenham papéis fundamentais na organização dos serviços necessários ao bem-estar coletivo. Definida pelo American College of Surgeons, uma profissão é um campo onde a maestria de um corpo complexo de conhecimento e habilidades é essencial. É uma vocação em que o conhecimento científico ou a prática de uma arte, fundamentada nesse conhecimento, é empregada em benefício dos outros. O compromisso com a competência, a integridade e a moralidade forma a base de um contrato social entre a profissão e a sociedade, que concede à profissão um monopólio sobre o uso de seu conhecimento, considerável autonomia na prática e o privilégio da auto-regulação. Em troca, a profissão deve prestar contas a quem serve e à sociedade como um todo.
Os Elementos Essenciais da Profissão
No cerne de toda profissão estão quatro elementos fundamentais:
- Monopólio do Conhecimento Especializado: Profissionais detêm o direito exclusivo de utilizar conhecimentos e habilidades especializados, o que lhes confere uma posição única na sociedade.
- Autonomia e Auto-Regulação: Em troca deste monopólio, profissionais desfrutam de uma relativa autonomia na prática e são responsáveis pela sua própria regulação.
- Serviço Altruísta: A profissão deve servir tanto indivíduos quanto a sociedade de forma altruísta, colocando o bem-estar do paciente acima de outros interesses.
- Responsabilidade pela Manutenção e Expansão do Conhecimento: Profissionais são responsáveis por atualizar e expandir continuamente seu conhecimento e habilidades.
O Que é Profissionalismo?
Profissionalismo descreve as qualidades cognitivas, morais e colegiais de um profissional. É o conjunto de razões pelas quais um pai se orgulha de dizer que seu filho é um médico e cirurgião. Profissionalismo é mais do que apenas conhecimento técnico; é uma combinação de ética, respeito e dedicação ao ofício e ao paciente.
Por Que Precisamos de um Código de Conduta Profissional?
A confiança é o alicerce da prática cirúrgica. O Código de Conduta Profissional esclarece a relação entre a profissão cirúrgica e a sociedade que serve, frequentemente referido como contrato social. Para os pacientes, o código cristaliza o compromisso da comunidade cirúrgica em relação aos indivíduos e suas comunidades. A confiança é construída, tijolo por tijolo.
O Código de Conduta Profissional
O Código de Conduta Profissional aplica os princípios gerais do profissionalismo à prática cirúrgica e serve como a fundação sobre a qual os privilégios profissionais e a confiança dos pacientes e do público são conquistados. Durante o cuidado pré-operatório, intraoperatório e pós-operatório, os cirurgiões têm a responsabilidade de:
- Advogar Eficazmente pelos interesses dos pacientes.
- Divulgar Opções Terapêuticas incluindo seus riscos e benefícios.
- Divulgar e Resolver Conflitos de Interesse que possam influenciar as decisões de cuidado.
- Ser Sensível e Respeitoso com os pacientes, compreendendo sua vulnerabilidade durante o período perioperatório.
- Divulgar Completamente Eventos Adversos e Erros Médicos.
- Reconhecer Necessidades Psicológicas, Sociais, Culturais e Espirituais dos pacientes.
- Incorporar Cuidados Especiais para Pacientes Terminais.
- Reconhecer e Apoiar as Necessidades das Famílias dos Pacientes.
- Respeitar o Conhecimento, Dignidade e Perspectiva de outros profissionais de saúde.
A Necessidade do Código de Profissionalismo para Cirurgiões
Procedimentos cirúrgicos são experiências extremas que impactam os pacientes fisiológica, psicológica e socialmente. Quando os pacientes se submetem a uma experiência cirúrgica, devem confiar que o cirurgião colocará seu bem-estar acima de todas as outras considerações. O código escrito ajuda a reforçar esses valores, garantindo que a confiança e o compromisso sejam mantidos.
Princípios Fundamentais do Código de Conduta Profissional
- Primazia do Bem-Estar do Paciente: Os interesses do paciente sempre devem vir em primeiro lugar. O altruísmo é central para esse conceito, e é o altruísmo do cirurgião que fomenta a confiança na relação médico-paciente.
- Autonomia do Paciente: Pacientes devem entender e tomar suas próprias decisões informadas sobre o tratamento. Os médicos devem ser honestos para que os pacientes façam escolhas educadas, garantindo que essas decisões estejam alinhadas com práticas éticas.
- Justiça Social: Como médicos, devemos advogar pelos pacientes individuais enquanto promovemos a saúde do sistema de saúde como um todo. Precisamos equilibrar as necessidades dos pacientes (autonomia) sem desviar recursos escassos que beneficiariam a sociedade (justiça social).
“Não há maior coisa a ser conquistada do que a confiança dos pacientes e da sociedade, pois ela é a base sobre a qual construímos nossas práticas e nossa profissão.” – William Osler
Tratamento Cirúrgico da Hemorragia digestiva alta por varizes esofágicas | Hipertensão Porta
O sistema portal é uma rede venosa de baixa pressão, com níveis fisiológicos <5 mmHg. Desta forma, o termo hipertensão portal (HP) designa uma síndrome clínica caracterizada pelo aumento mantido na pressão venosa em níveis acima dos fisiológicos. Ela é considerada clinicamente significante quando acima de 10 mmHg; neste nível existe o risco de surgimento de varizes esofagogástricas (VEG). Por sua vez, valores acima de 12 mmHg cursam com risco de rompimento dessas varizes, sua principal complicação.
ARTIGO DE REVISÃO – HIPERTENSÃO PORTAL
O aumento do fluxo como fator preponderante inicial da HP é raro e representado por fístulas arterioportais congênitas, traumáticas ou neoplásicas. O aumento da resistência é a condição fisiopatológica inicial mais comum e pode ser classificada de acordo com o local de obstrução ao fluxo em: pré-hepática, intra-hepática e pós-hepática. A HP intra-hepática responde pela grande maioria dos casos e pode ser subdividida de acordo com o local de acometimento estrutural no parênquima hepático em: pré-sinusoidal (ex: esquistossomose hepatoesplênica – EHE), sinusoidal (ex: cirrose hepática) e pós-sinusoidal (ex: doença venoclusiva). Em nosso meio, a maioria dos casos é decorrente da EHE e das hepatopatias crônicas complicadas com cirrose.
O tratamento da HP depende da causa subjacente, da condição clínica e do momento em que é realizado. Pacientes com função hepática comprometida têm abordagem diversa daqueles com ela preservada, como os portadores de EHE. Além disso, o tratamento pode ser emergencial (durante episódio agudo de hemorragia) ou eletivo, como profilaxia pré-primária, primária ou secundária. Por essa diversidade de situações clínicas, não existe modalidade única de tratamento.
O objetivo da aula abaixo foi avaliar os avanços e as estratégias atuais empregadas no tratamento emergencial e eletivo da hemorragia digestiva varicosa em pacientes cirróticos e esquistossomóticos.
AULA: TRATAMENTO CIRÚRGICO DA HIPERTENSÃO PORTAL
FERIDA PÓS-OPERATÓRIA

A avaliação e os cuidados de feridas pós-operatórias deve ser do domínio de todos os profissionais que atuam na clínica cirúrgica. O conhecimento a cerca dos processos relacionados a cicatrização tecidual é importante tanto nos cuidados como na prevenção de complicações, tais como: infecções e deiscência. Como tal, todos os profissionais médicos, sendo eles cirurgiões ou de outras especialidades, que participam do manejo clínico dos pacientes no período perioperatório devem apreciar a fisiologia da cicatrização de feridas e os princípios de tratamento de feridas pós-operatório. O objetivo deste artigo é atualizar os profissionais médicos de outras especialidades sobre os aspectos importantes do tratamento de feridas pós-operatório através de uma revisão da fisiologia da cicatrização de feridas, os métodos de limpeza e curativo, bem como um guia sobre complicações de feridas pós-operatórias mais prevalentes e como devem ser manejados nesta situação.
Esophagectomy: Anastomotic Complications (Leakage and Stricture)

Esophagectomy can be used to treat several esophageal diseases; it is most commonly used for treatment of esophageal cancer. Esophagectomy is a major procedure that may result in various complications. This article reviews only the important complications resulting from esophageal resection, which are anastomotic complications after esophageal reconstruction (leakage and stricture), delayed emptying or dumping syndrome, reflux, and chylothorax.
Causas de conversão da VIDEOCOLECISTECTOMIA
Atualmente, a colecistectomia laparoscópica é a abordagem preferida para o tratamento da litíase biliar, representando cerca de 90% dos procedimentos realizados, uma marca alcançada nos Estados Unidos em 1992. A popularidade dessa técnica se deve a suas vantagens evidentes: menos dor no pós-operatório, recuperação mais rápida, redução dos dias de trabalho perdidos e menor tempo de hospitalização. Apesar de ser considerada o padrão-ouro na cirurgia biliar, a colecistectomia laparoscópica não está isenta de desafios. Entre 2% e 15% dos casos podem exigir a conversão para cirurgia convencional. Os motivos mais comuns para essa conversão incluem dificuldades na identificação da anatomia, suspeita de lesão da árvore biliar e controle de sangramentos. Identificar os fatores que contribuem para uma maior taxa de conversão é essencial para a equipe cirúrgica. Isso não apenas permite uma avaliação mais precisa da complexidade do procedimento, mas também ajuda na preparação do paciente para possíveis riscos e na mobilização de cirurgiões mais experientes quando necessário. Em um cenário onde a precisão e a segurança são cruciais, a compreensão dos desafios e a preparação adequada podem fazer toda a diferença no resultado da cirurgia.
Relacionados ao Paciente: 1. Obesidade (IMC > 35), 2. Sexo Masculino, 3. Idade > 65 anos, 4. Diabetes Mellitus e 5. ASA > 2.
Relacionadas a Doença: 1. Colecistite Aguda, 2. Líquido Pericolecístico, 3. Pós – CPRE, 4. Síndrome de Mirizzi e 5. Edema da parede da vesícula > 5 mm.
Relacionadas a Cirurgia: 1. Hemorragia, 2. Aderências firmes, 3. Anatomia obscura, 4. Fístulas internas e 5. Cirurgia abdominal prévia.
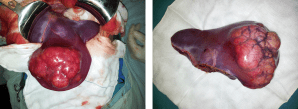
POST-HEPATECTOMY ADVERSE EVENTS
Hepatic resection had an impressive growth over time. It has been widely performed for the treatment of various liver diseases, such as malignant tumors, benign tumors, calculi in the intrahepatic ducts, hydatid disease, and abscesses. Management of hepatic resection is challenging. Despite technical advances and high experience of liver resection of specialized centers, it is still burdened by relatively high rates of postoperative morbidity and mortality. Especially, complex resections are being increasingly performed in high risk and older patient population. Operation on the liver is especially challenging because of its unique anatomic architecture and because of its vital functions. Common post-hepatectomy complications include venous catheter-related infection, pleural effusion, incisional infection, pulmonary atelectasis or infection, ascites, subphrenic infection, urinary tract infection, intraperitoneal hemorrhage, gastrointestinal tract bleeding, biliary tract hemorrhage, coagulation disorders, bile leakage, and liver failure. These problems are closely related to surgical manipulations, anesthesia, preoperative evaluation and preparation, and postoperative observation and management. The safety profile of hepatectomy probably can be improved if the surgeons and medical staff involved have comprehensive knowledge of the expected complications and expertise in their management.
Classroom: Hepatic Resections
The era of hepatic surgery began with a left lateral hepatic lobectomy performed successfully by Langenbuch in Germany in 1887. Since then, hepatectomy has been widely performed for the treatment of various liver diseases, such as malignant tumors, benign tumors, calculi in the intrahepatic ducts, hydatid disease, and abscesses. Operation on the liver is especially challenging because of its unique anatomic architecture and because of its vital functions. Despite technical advances and high experience of liver resection of specialized centers, it is still burdened by relatively high rates of postoperative morbidity (4.09%-47.7%) and mortality (0.24%-9.7%). This review article focuses on the major postoperative issues after hepatic resection and presents the current management.
REVIEW_ARTICLE_HEPATECTOMY_COMPLICATIONS
PANCREATIC PSEUDOCYST
Classroom: Principles of Pancreatic Surgery
The pancreatic pseudocyst is a collection of pancreatic secretions contained within a fibrous sac comprised of chronic inflammatory cells and fibroblasts in and adjacent to the pancreas contained by surrounding structures. Why a fibrous sac filled with pancreatic fluid is the source of so much interest, speculation, and emotion amongst surgeons and gastroenterologists is indeed hard to understand. Do we debate so vigorously about bilomas, urinomas, or other abdominal collections of visceral secretions? Perhaps it is because the pancreatic pseudocyst represents a sleeping tiger, which though frequently harmless, still can rise up unexpectedly and attack with its enzymatic claws into adjacent visceral and vascular structures and cause lifethreatening complications. Another part of the debate and puzzlement about pancreatic pseudocysts is related to confusion about pancreatic pseudocyst definition and nomenclature. The Atlanta classification, developed in 1992, was a pioneering effort in describing and defining morphologic entities in acute pancreatitis. Since then, a working group has been revising this system to incorporate more modern experience into the terminology. In the latest version of this system, pancreatitis is divided into acute interstitial edematous pancreatitis (IEP) and necrotizing pancreatitis (NP), based on the presence of pancreatic tissue necrosis. The fluid collections associated with these two “types” of pancreatitis are also differentiated. Early (<4 weeks into the disease course) peripancreatic fluid collections in IEP are referred to as acute peripancreatic fluid collections (APFC), whereas in NP, they are referred to as postnecrotic peripancreatic fluid collections (PNPFC). Late (>4 weeks) fluid collections in IEP are called pancreatic pseudocysts, and in NP, they are called walled-off pancreatic necrosis (WOPN).
10 Princípios da RELAÇÃO CIRURGIÃO-PACIENTE


Quando a perspectiva de uma cirurgia surge, seja para corrigir uma condição médica, melhorar a estética ou simplesmente enfrentar uma situação inesperada, o medo e a apreensão são reações naturais. A visão de dor, complicações e a sensação de perda de controle podem ser opressoras, especialmente diante dos avanços tecnológicos prometidos pela medicina. No entanto, para enfrentar esses desafios de forma eficaz e justa, é crucial entender o processo cirúrgico e os papéis envolvidos. Aqui estão algumas orientações para pacientes e familiares, com base em princípios éticos e práticos da medicina moderna.
1. Relação Paciente-Cirurgião (ã): Construindo Confiança
A confiança mútua entre paciente e médico é fundamental. Evite se submeter a pressões para procedimentos rápidos e impessoais. Um relacionamento humanizado, onde o médico dedica tempo para entender o paciente, é essencial para evitar acusações injustas e frustrações. As consultas devem ser um espaço para esclarecimentos detalhados e empáticos, não apenas para realizar procedimentos.
2. Clareza e Transparência na Informação
Informações claras sobre o procedimento, suas consequências e riscos são essenciais. Evite jargões técnicos e explique cada aspecto da cirurgia em termos compreensíveis. A comunicação aberta reduz a ansiedade e prepara os pacientes para os possíveis desdobramentos da cirurgia.
3. Expectativas Realistas
Especialmente em procedimentos estéticos, alinhar as expectativas do paciente com a realidade é crucial. Muitas vezes, expectativas irreais podem levar a descontentamentos. É importante discutir de maneira honesta o que a cirurgia pode realmente alcançar e o que pode ser meramente aspiracional.
4. Avaliação Abrangente do Risco
O risco cirúrgico não se limita a aspectos cardíacos. Uma avaliação completa deve considerar todos os sistemas do corpo e a saúde mental do paciente. Exames físicos completos e, se necessário, avaliações psicológicas são partes vitais do pré-operatório.
5. O Papel do Anestesiologista
A escolha e a administração da anestesia são responsabilidades cruciais e devem ser discutidas com o anestesiologista. A decisão sobre o tipo de anestesia deve considerar as melhores práticas e o estado de saúde do paciente, não apenas a preferência do cirurgião.
6. Preparação para Possíveis Mudanças
A cirurgia pode trazer surpresas. É importante que o paciente esteja ciente de que o plano cirúrgico pode mudar com base nas condições encontradas durante o procedimento. Essas mudanças podem influenciar o tempo de recuperação e os custos envolvidos.
7. Documentação Completa
Preencher adequadamente o prontuário médico é crucial. Todos os detalhes, desde os exames realizados até os esclarecimentos fornecidos, devem estar documentados com precisão. Essa prática não apenas protege o paciente, mas também o profissional médico.
8. Comunicação Detalhada do Procedimento
Descreva minuciosamente o ato cirúrgico e os materiais encaminhados para análise. Certifique-se de que todos os procedimentos sejam seguidos corretamente e que todos os materiais estejam devidamente identificados.
9. Pós-Operatório: Acompanhamento e Cuidados
O acompanhamento pós-operatório deve ser meticuloso. Registre as datas e horários das visitas médicas e todas as providências tomadas. Forneça orientações claras sobre a alta e o acompanhamento ambulatorial.
10. Atenção ao Estado Emocional do Paciente
Pacientes com instabilidade emocional podem ter uma experiência mais difícil com a cirurgia. É vital que essas questões sejam abordadas com apoio especializado para garantir que o paciente esteja mentalmente preparado para o procedimento.
Conclusão
A ética na medicina, especialmente na cirurgia, vai além dos conceitos de eficiência técnica e competência. Trata-se de respeito mútuo e comunicação aberta entre médico e paciente. A prática médica ideal exige não apenas habilidades técnicas e conhecimento, mas também empatia, compreensão e um compromisso com a integridade e o bem-estar do paciente. Assim, com preparação cuidadosa e uma abordagem centrada no paciente, é possível enfrentar os desafios da cirurgia com confiança e esperança. Esta abordagem humanizada e informativa ajuda a construir uma relação de confiança, minimizando o medo e a ansiedade associados ao tratamento cirúrgico e garantindo que todos os aspectos do cuidado sejam geridos com a maior consideração e respeito.
The General Surgery Job Market

There is a current shortage of general surgeons nationwide. A growing elderly population and ongoing trends toward increased health care use have contributed to a higher demand for surgical services, without a corresponding increase in the supply of surgeons. The number of general surgeons per 100,000 people in the United States declined by 26% from the 1980s to 2005. Cumulative growth in demand for general surgery is projected to exceed 25% by 2025. The Association of American Medical Colleges has projected a shortage of 41,000 general surgeons by 2025. General surgeons make up 33% of the total projected physician shortage, the second highest after primary care physicians, who make up 37% of the total shortage. Despite the demand for general surgeons, the percentage of general surgery trainees going directly into practice is decreasing while the percentage of trainees pursuing subspecialty training is increasing. A recent study reported that graduating residents who lacked confidence in their skills to operate independently were more likely to pursue subspecialty training. This suggests that some graduating residents are motivated to obtain subspecialty training to gain more experience rather than narrow their clinical scope of practice. Given the projected shortage of general surgeons, this will be a crucial distinction when reforming surgical education. General surgery trainees interested in career planning would benefit from understanding the demand for general and/or specialty skills in a job market heavily influenced by a constant stream of new graduates. However, little is currently known about the demand for subspecialty vs general surgical skills in the current job market. The goal of this study was to describe the current job market for general surgeons in the United States, using Oregon and Wisconsin as surrogates. Furthermore, we sought to compare the skills required by the job market with those of graduating trainees with the goal of gaining insight that might assist in workforce planning and surgical education reform.
PRINCIPLES OF OSTOMY MANAGEMENT

The creation of a stoma is a technical exercise. Like most undertakings, if done correctly, the stoma will usually function well with minimal complications for the remainder of the ostomate’s life. Conversely, if created poorly, stoma complications are common and can lead to years of misery. Intestinal stomas are in fact enterocutaneous anastomoses and all the principles that apply to creation of any anastomosis (i.e., using healthy intestine, avoiding ischemia and undue tension) are important in stoma creation.
MOST COMMOM POSTOPERATIVE PROBLEMS
Despite good preoperative assessment, surgical and anaesthetic technique and perioperative management, unexpected symptoms or signs arise after operation that may herald a complication. Detecting these early by regular monitoring and surgical review means early treatment can often forestall major deterioration. Managing problems such as pain, fever or collapse requires correct diagnosis then early treatment. Determining the cause can be challenging, particularly if the patient is anxious, in pain or not fully recovered from anaesthesia. It is vital to see and assess the patient and if necessary, arrange investigations, whatever the hour, when deterio-ration suggests potentially serious but often remediable complications. Consider also whether and when to call for senior help.
Survival Guide for SURGERY ROUND

SURGERY ROUND
Medical students are often attached to the various services. They can provide a significant contribution to patient care. However, their work requires supervision by the surgical intern/resident who takes primary clinical responsibility. Subinterns are senior medical students who are seeking additional clinical experience. Their assistance is needed and appreciated, but again, close supervision of their clinical responsibilities by the intern/resident is mandatory.Outside reading is recommended, including textbooks, reference sources, and monthly journals.Eating is prohibited in patient care areas.Maintain patient confidentiality at all times.At conferences use only patient initials in presentations; and speak carefully and respectfully on work rounds.
PRINCIPLES
1. Always be punctual (this includes ward rounds, operating room, clinics, conferences, morbidity and mortality). Personal appearance is very important. Maintain a high standard including clean shirt and tie (or equivalent) and a clean white coat. The day begins early. Be ready with all the data to start rounds with the senior resident or chief resident. Be sure to provide enough time each morning to examine your patients before rounds.
ABOUT NOTES
2.Aim to get all of your chart notes written as soon as possible; this will greatly increase your effi ciency during the day. Sign and print your name, and include your beeper number, date, and time. Progress notes on patients are required daily. Surgical progress notes should be succinct and accurate, briefl y summarizing the patient’s clinical status and plan of management. Someone unfamiliar with the case should be able to get a good understanding of the patient’s condition from one or two notes. Operative consent is obtained after admitting the patient, performing the history and physical examination, discussing the risks, benefi ts, and alternatives of the procedure(s), and having the patient’s nurse sign the consent with the patient. If you are unaware of the risks and benefi ts of a procedure, discuss this with the service chief resident. Blood transfusion attestation forms need to be signed by the counseling physician before each surgical procedure.
OPERATING ROOM
3. Arrive in the operating room with the patient and before the attending physician or chief resident. Make sure that the charts and all of the relevant x-rays are in the operating room. Make sure that the x-rays are on the x-ray view box prior to the commencement of the case. The intern or resident performing the case should be familiar with the patient’s history and physical exam, current medications, and comorbidities, and be familiar with the principles of the operation prior to arriving in the operating room. Make it a habit to introduce yourself to the patient before the operation. It is mandatory that the surgical resident involved with a case in the operating room attend the start of the case punctually. Scheduled operative cases do not necessarily occur at the listed time. For this reason, it is necessary to check with the operating room front desk frequently. Do not rely on being paged. Conduct in the operating room includes assisting with the preoperative positioning and preparation of the patient; this includes shaving, catheterization, protection of pressure points, and thromboembolism protection. The resident should escort the patient from the operating room to the intensive care unit (ICU) or the postanesthetic care unit with the anesthesiologists. The operating surgeon is responsible for dictating the case. The resident must record all cases performed. For cases admitted to the surgery ICU, a hand-over to the surgery ICU resident is mandatory.This includes discussing all the preoperative assessment, operative details, and postoperative management of the case with the ICU resident.
ROUNDS
4. Signing out to cross-cover services must be performed in a meticulous and careful fashion. All patients should be discussed between the surgical intern and the cross-covering intern to cover all potential problems. A sign-out list containing all the patients, patient locations, and the responsible attendings should be given personally to the cross-cover intern. Any investigations performed at night (e.g., lab studies, chest x-ray, electrocardiogram [ECG]) should be checked that night by the covering intern. No test order should go unchecked. Abnormal lab values should be reviewed and discussed with the senior resident or the attending staff, especially on preoperative patients. Starting antibiotics should be a decision left to the senior resident or attending staff. If consultants are asked to see patients, their recommendations mustbe discussed with your senior resident or attending priorto initiating any new plans. Independent thought is good; independent action is bad.
SUPERVISION
5. Document all procedures performed on patients—including arterial lines, chest tubes, and central lines—with a short procedure note in the chart. Every patient contact should be documented in the patient record.If you see a patient in the middle of the night, write a short note to describe your assessment and plan. Remember, if there is no documentation, then nobody responded to the patient’s complaint or needs. Obtain appropriate supervision for procedures. There are always more senior residents available if your chief is not. Protect yourself; practice universal precautions! Wash your hands before and after examining a patient. Wear gloves. All wounds should be inspected every day by the surgical intern as part of the clinical examination. Please re-dress them; the nursing staff is not always immediately available to do so. There should never be any surprises in the morning.
RESIDENTS
Your senior resident is responsible for the service and should be kept aware of any problems, regardless of the time of day. If the senior resident is not available, the attending staff should be contacted directly. There are always senior residents in the hospital who are available to be used as resources for emergencies. Always be aware of who is in-house (i.e., consult resident, ICU resident, trauma chief). A surgery resident’s days are long. They start early and they fi nish late. Always remember the three A’s to being a successful resident: Affable, Available, and Able. Be prepared to maintain a flexible daily schedule depending on the workload of the service and the requirement for additional manpower.
“COMO PODEMOS CURAR A MEDICINA?”
“Nos últimos anos percebemos que estávamos na mais profunda crise da existência da medicina, devido a algo sobre o que você normalmente não pensa quando você é um médico preocupado em fazer o bem para as pessoas, que é o custo do tratamento de saúde. Não há um país no mundo que não esteja perguntando agora se podemos custear o que médicos fazem. A luta política que desenvolvemos tornou-se aquela sobre se o governo é o problema ou se as companhias de seguro são o problema. E a resposta é sim e não; é mais profundo que tudo isso. A causa de nossos problemas é, na verdade, a complexidade que a ciência nos deu. E para entender isso, voltarei algumas gerações…”
“CIRURGIA: PASSADO, PRESENTE e FUTURO ROBÓTICO”
A cirurgiã e inventora Catherine Mohr nos guia pela história da cirurgia (e seu passado pré-anestesia e pré-antissepsia), e depois demonstra algumas das mais novas ferramentas para cirurgias realizadas através de pequenas incisões, usando ágeis mãos robóticas.
Ebook: Princípios da Cirurgia Hepatobiliar

Cirurgia Hepatobiliar
Considera-se que a cirurgia hepática começou após o advento da anestesia e da anti-sepsia. No entanto, muito antes disso, diversos autores já relatavam suas experiências com ressecções do fígado. As primeiras descrições de “cirurgias hepáticas” consistiam no relato de avulsões parciais ou totais de porções do fígado após lesões traumáticas do abdome. O relato de Elliot (1897) exemplifica muito dos temores dos cirurgiões da época: “O fígado (…) é tão friável, tão cheio de vasos e tão evidentemente impossível de ser suturado que parece ser improvável o manejo bem sucedido de grandes lesões de seu parênquima”.
CIRURGIA HEPATOBILIAR_ASPECTOS BÁSICOS
Lymph Node Dissection in Gastric Adenocarcinoma
Extent of lymph node dissection has been an area of controversy in gastric adenocarcinoma for many years. Some surgeons believe that cancer metastasizes through a stepwise progression, and an extensive lymphadenectomy is necessary to improve survival and/or cure the patient. Other physicians argue that extensive ly-mphadenectomies only add pe-rioperative morbidity and mor-tality and do not improve survival. Asian countries have been performing extended lymphadenectomies routinely for many years with promising survival data, although Western countries have not been able to reproduce those results. Much of the controversy surrounding lymphadenectomies started in the 1980s when Japanese studies reported superior survival rates matched stage for stage, compared to the United States. This was theorized to be secondary to the more extensive lymphadenectomy performed in Japan compared to the United States.

A United Kingdom study randomized 400 patients to either a D1 or a D2 lymph node dissection. Those patients with tumors in the upper or middle third of the stomach underwent a distal pancreaticosplenectomy to obtain retropancreatic and splenic hilar nodes. While the 5-year survival rates were not statistically significant between the two groups, on multivariate analyses it was noted that those patients in the D2 group that did not undergo the distal pancreaticosplenectomy had an increased survival compared with the D1 group. A trial in the Netherlands randomized 380 gastric cancer patients to a D1 lymphadenectomy and 331 patients to a D2 lymphadenectomy. Similar to the United Kingdom study, there was not a significant difference in survival between the two groups, even when followed out to 11 years. There was a significant increase in postoperative complications in the D2 group compared with the D1 group (43 % vs. 25 %, respectively) as well as mortality (10 % vs. 4 %, respectively).
The data from these two studies suggest that a pancreaticosplenectomy performed to harvest lymph nodes seems to only add morbidity and mortality while not improving survival. One concern raised about the prior two studies was the variation in surgical technique and lack of standardization of surgeon experience. A Taiwanese study accounted for this by performing the study at a single institution with three surgeons, each of whom had completed at least 25 D3 lymph node dissections prior to the study. Patients with gastric cancer were randomized to a D1 lymph node dissection (defined as resection of perigastric lymph nodes along the lesser and greater curves of the stomach) or a D3 lymph node dissection (defined as resection of additional lymph nodes surrounding the splenic, common hepatic, left gastric arteries, nodes in the hepatoduodenal ligament, and retropancreatic lymph nodes). There was an overall 5-year survival benefit with the D3 group of 60 % compared with the D1 group of 54 %. A Japanese study evaluated a more aggressive lymph node dissection and randomized patients to a D2 dissection or a para-aortic lymph node dissection (PAND). There was no significant difference in 5-year survival between the two groups with a trend toward an increase in complications in the PAND group. Multiple studies have shown that the number of positive lymph nodes is a significant predictor of survival. Current AJCC guidelines stipulate that at least 15 lymph nodes are needed for pathologic examination to obtain adequate staging.
Laparoscopic techniques have become an integral part of surgical practice over the past several decades. For gastric cancer, multiple retrospective studies have reported the advantages of laparoscopic gastrectomy (LG) over open gastrectomy (OG). A recent meta-analysis of 15 nonrandomized comparative studies has also shown that although LG had a longer operative time than OG, it was associated with lower intraoperative blood loss, overall complication rate, fewer wound-related complications, quicker recovery of gastrointestinal motility with shorter time to first flatus and oral intake, and shorter hospital stay. A randomized prospective trial comparing laparoscopic assisted with open subtotal gastrectomy reported that LG had a significantly lower blood loss (229 ± 144 ml versus 391 ± 136 ml; P< 0.001), shorter time to resumption of oral intake (5.1 ± 0.5 days versus 7.4 ± 2 days; P< 0.001), and earlier discharge from hospital (10.3 ± 3.6 days versus 14.5 ± 4.6 days; P< 0.001).
Como funciona o GRAMPEADOR INTESTINAL ?
O objetivo do cirurgião ao realizar qualquer intervenção é que esta seja segura e eficiente. O procedimento deve ser o mais rápido possível, com o menor trauma tecidual, restaurando a função, e conseqüentemente diminuindo ao máximo as possibilidades de intercorrências no pós-operatório. A moderna cirurgia atinge estes objetivos de forma bastante satisfatória, porém, as complicações relacionadas às suturas ainda ocorrem com alguma freqüência. Foi somente no final do século XIX, que as suturas gastrointestinais adquiriram confiabilidade, com o conhecimento básico dos princípios da cicatrização dos tecidos. Os fatores envolvidos no reparo tecidual relacionam-se não só à técnica, mas também ao paciente individualmente, e à área a ser operada. A presença de isquemia, edema, infecção e desnutrição são alguns dos elementos que retardam e prejudicam a cicatrização. A variação na habilidade dos cirurgiões serviu de motivação para o desenvolvimento de dispositivos, que superando as diferenças individuais, permitissem que as técnicas fossem executadas adequadamente, e cujo resultado final fosse o melhor possível. Toda técnica deve ser reproduzida de forma confiável pelo maior número de cirurgiões para que seus resultados sejam adotados e reconhecidos como eficazes.
POSTOPERATIVE ILEUS
POSTOPERATIVE ILEUS_REVIEW ARTICLE
 In systems that try to minimize hospital stay after abdominal surgery, one of the principal limiting factors is the recovery of adequate bowel function, which can delay discharge or lead to readmission. Postoperative ileus (POI) is the term given to the cessation of intestinal function following surgery. Although all surgical procedures put the patient at risk for POI, gastrointestinal tract surgeries in particular are associated with a temporary cessation of intestinal function. The duration of POI varies, lasting from a few hours to several weeks. Prolonged postoperative ileus, also known as pathologic postoperative ileus, can be caused by a myriad of pathologic processes that are treated with limited success by clinical and pharmacologic management. Studies of large administrative databases show that, on average, patients with a diagnosis of POI stay 5 days longer in hospital after abdominal surgery than patients without POI. Over the last decade, substantial efforts have been made to minimize the duration of POI, as there appears to be no associated physiologic benefit, and it is currently the primary factor delaying recovery for most patients. In this review, we define POI, describe the pathogenesis and briefly discuss clinical management before detailing current pharmacologic management options.
In systems that try to minimize hospital stay after abdominal surgery, one of the principal limiting factors is the recovery of adequate bowel function, which can delay discharge or lead to readmission. Postoperative ileus (POI) is the term given to the cessation of intestinal function following surgery. Although all surgical procedures put the patient at risk for POI, gastrointestinal tract surgeries in particular are associated with a temporary cessation of intestinal function. The duration of POI varies, lasting from a few hours to several weeks. Prolonged postoperative ileus, also known as pathologic postoperative ileus, can be caused by a myriad of pathologic processes that are treated with limited success by clinical and pharmacologic management. Studies of large administrative databases show that, on average, patients with a diagnosis of POI stay 5 days longer in hospital after abdominal surgery than patients without POI. Over the last decade, substantial efforts have been made to minimize the duration of POI, as there appears to be no associated physiologic benefit, and it is currently the primary factor delaying recovery for most patients. In this review, we define POI, describe the pathogenesis and briefly discuss clinical management before detailing current pharmacologic management options.
Prontuário Médico | EVOLUÇÃO CIRÚRGICA S.O.A.P

INTRODUÇÃO
O prontuário médico é o conjunto de documentos padronizados e ordenados, onde devem ser registrados todos os cuidados profissionais prestados aos pacientes e que atesta o atendimento médico a uma pessoa numa instituição de assistência médica ou num consultório médico. É também o documento repositório do segredo médico do paciente. O preenchimento do prontuário médico é obrigação e responsabilidade intransferíveis do médico, fazendo-se exceção aos hospitais de ensino, onde alunos de medicina o fazem sob supervisão, correção e responsabilidade de médicos, sejam professores de medicina ou do staff do hospital de ensino. É prática antiética e ilegal, portanto condenável, delegar seu preenchimento a outrem que não médico habilitado perante o Conselho de Medicina. O prontuário médico corretamente preenchido é, e efetivamente tem sido, a principal peça de defesa do médico nos casos de denúncias por mal atendimento com indícios de imperícia, imprudência ou negligência, ou seja, na presunção da existência de erro médico. Este é o primeiro documento que a polícia, a Justiça e o próprio Conselho solicitam aos hospitais/médicos denunciados para apreciação dos fatos da denúncia.
ASPECTOS HISTÓRICOS
Na década de 1960, Lawrence Weed publicou um artigo (Weed LL. Medical records that guide and teach. N Engl J Med; 1968) que descreve um modelo de prontuário que é atualmente adotado em diversos centros médicos de todo o mundo. O modelo de Weed se destaca pela objetividade, organização, maior facilidade de acesso às informações para tomada de decisões e pela descrição sistemática das evidencias e das razões que apoiam as conclusões e os planos diagnósticos e terapêuticos durante o acompanhamento do paciente. O termo originalmente utilizado por Weed para o seu modelo de prontuário foi Prontuário Médico Orientado por Problemas (Problem-Oriented Medical Record).
No Brasil este modelo ficou conhecido como Prontuário Orientado por Problemas e Evidências (POPE) para destacar uma das características básicas deste modelo que é a ênfase nas evidências clínicas e científicas. No POPE as notas de evolução são orientadas pelos problemas ativos do paciente e segue o contexto descrito como SOAP. Cada letra da sigla SOAP se refere a um dos quatro aspectos fundamentais das notas de evolução diária, ou seja os dados subjetivos (S), os dados objetivos (O), a avaliação (A) e o planejamento (P).
COMO DEVE SER PREENCHIDO O PRONTUÁRIO NO SISTEMA S.O.A.P.?
No momento da realização das anotações o médico deverá identificar o paciente pelo nome e sobrenome, juntamente com a idade, a Clínica ao qual esta internado e o horário. Os itens de evolução médica são assim transcritos:
1. Os dados subjetivos (S) compreendem as queixas dos pacientes e outras informações fornecidas pelos pacientes, parentes ou acompanhantes.
2. Os dados objetivos (O) incluem os achados de exame físico e os achados de exames complementares.
3. A avaliação (A) se refere às conclusões sobre a situação do paciente, os pensamentos relativos ao diagnóstico e a resposta ao tratamento, tomando por base os achados subjetivos e objetivos.
4. Os planos (P) inclui os exames a serem solicitados visando o diagnóstico, as razões para inclusão, modificação de doses ou retirada de itens da terapêutica e as informações prestadas aos pacientes e familiares visando orientação e educação.
ASPECTOS ÉTICOS E LEGAIS
A “medicina de defesa” reforça a importância do prontuário e de seu preenchimento completo. O documento, para ser admitido em juízo como elemento de prova, necessita de ter sua autenticidade reconhecida, estar datado e assinado. A ausência desses elementos demonstra má qualidade da assistência prestada ao paciente. Rasuras comprometem o valor legal. Em casos de retificações, aconselha-se a escrever entre parênteses indicações como sem efeito, digo ou expressões análogas e, a seguir, escrever a correção.
Segundo o artigo 299 do Código Penal, a anotação incorreta, incompleta, falseada ou inexistente no prontuário quanto aos fatos relacionados com o paciente pode caracterizar falsidade ideológica: “Omitir, em documento público ou particular, declaração que dele devia constar ou nele inserir ou fazer inserir declaração falsa ou diversa da que devia ser escrita, com o fim de prejudicar direito, criar obrigação ou alterar a verdade sobre fato juridicamente relevante. Pena – reclusão de 1 (um) a 5 (cinco) anos, e multa, se o documento é público, e reclusão de 1 (um) ano a 3 (três) anos, e multa, se o documento é particular”. Se o agente for funcionário público e cometer o crime, prevalecendo-se do cargo, aumenta-se a pena de sexta parte.
Desta forma deverão constar em cada folha de evolução clínica do paciente as seguintes informações:
1. Identificação: Nome, idade e sexo; 2. Dias de Internação; 3. Diagnósticos (Sindrômico, Anatômico e Etiológico); 4. Terapêutica Básica; e 5.Data e hora de atendimento;
Os autores de todos os registros no prontuário deverão ser identificados através do nome completo e assinatura do profissional assistente com seu número de inscrição no respectivo conselho de classe. Recomenda-se SEMPRE USAR CARIMBO. Em caso de não-profissionais assistentes, como alunos em treinamento, é necessário que sua assinatura conste ao lado da do titular atendente.
A caligrafia faz parte da ética profissional do médico. As anotações precisam ser legíveis. “É vedado ao médico receitar ou atestar de forma secreta ou ilegível, assim como assinar em branco papeletas de receituários, laudos, atestados ou quaisquer outros documentos médicos” (artigo 39 do Código de Ética Médica). Nos prontuários em suporte de papel, é obrigatória a legibilidade da letra do profissional que atendeu o paciente (Resolução CFM n.º 1.638/02).
LIFE AS A SURGEON

Life as a Surgeon
Surgical careers begin long before one is known as a surgeon. Medicine in general, and surgery in particular, is competitive from the start. As the competition begins, in college or earlier, students are confronted with choices of doing what interests them and what they may truly enjoy vs doing what is required to get to the next step. It is easy to get caught up in the routine of what is required and to lose track of why one wanted to become a doctor, much less a surgeon, in the first place. The professions of medicine and surgery are vocations that require extensive knowledge and skill. They also require a high level of discretion and trustworthiness. The social contract between the medical profession and the public holds professionals to very high standards of competence and moral responsibility. Tom Krizek goes on to explain that a profession is a declaration of a way of life ‘‘in which expert knowledge is used not primarily for personal gain, but for the benefit of those who need that knowledge.’’
For physicians, part of professionalism requires that when confronted with a choice between what is good for the physician and what is good for the patient, they choose the latter. This occurs and is expected sometimes to the detriment of personal good and that of physicians’ families. Tom Krizek even goes so far as to question whether surgery is an ‘‘impairing profession.’’ This forces one to consider the anticipated lifestyle. In sorting this out, it is neither an ethical breach nor a sign of weakness to allocate high priority to families and to personal well-being. When trying to explain why surgery may be an impairing profession, Krizek expands with a cynical description of the selection process. Medical schools seek applicants with high intelligence; responsible behavior; a studious, hard-working nature; a logical and scientific approach to life and academics; and concern for living creatures. He goes further to explain that in addition to these characteristics, medical schools also look for intensity and drive, but are often unable to make distinctions among those who are too intense, have too much drive, or are too ingratiating.
Medical School
There are many ethical challenges confronting medical students. As they start, medical students often have altruistic intentions, and at the same time are concerned with financial security. The cost of medical education is significant. This can encourage graduates to choose specialty training according to what will provide them the most expedient means of repaying their debt. This can have a significant, and deleterious, impact on the health care system in that the majority of medical graduates choose to pursue specialty training, leaving a gap in the availability of primary care providers. As medical students move into their clinical training, they begin interacting with patients. One concern during this time is how medical students should respond and carry on once they believe that a mistake on their part has resulted in the injury or death of another human being. In addition, the demands of studying for tests, giving presentations, writing notes, and seeing patients can be overwhelming. The humanistic and altruistic values that medical students have when they enter medical school can be lost as they take on so much responsibility. They can start to see patient interactions as obstacles that get in the way of their other work requirements. During their clinical years, medical students decide what field they will ultimately pursue. For students to make an informed decision about a career in surgery, they need to know what surgeons do, why they do it, and how surgery differs from other branches of medicine. It is important for them to be aware of what the life of a surgeon entails and whether it is possible for them to balance a surgical career with a rewarding family life.
Surgical Residency
Beginning residents are confronted with a seemingly unbearable workload, and they experience exhaustion to the point where the patient may seem like ‘‘the enemy.’’ At the same time, they must learn how to establish strong trusting relationships with patients. For the first time, they face the challenge of accepting morbidity and death that may have resulted directly from their own actions. It is important that residents learn ways to communicate their experience to friends and family, who may not understand the details of a surgeon’s work but can provide valuable support. The mid-level resident confronts the ethical management of ascending levels of responsibility and risks, along with increasing emphasis on technical knowledge and skills. It is at this level that the surgical education process is challenged to deal with the resident who does not display the ability to gain the skills required to complete training as a surgeon. Residents at this level also must deal with the increasing level of responsibility to the more junior residents and medical students who are dependent on them as teacher, organizer, and role model. All of this increasing responsibility comes at a time when the resident must read extensively, maintain a family life, and begin to put long-range plans into practice in preparation for the last rotation into the chosen final career path. The senior surgical resident should have acquired the basics of surgical technique and patient management, accepting nearly independent responsibility for patient care. The resident at this level must efficiently and fairly coordinate the functioning team, engage in teaching activities, and work closely with all complements of the staff. As far as ethics education is concerned, residents at this stage should be able to teach leadership, teamwork, and decision-making. They should be prepared to take on the value judgments that guide the financial and political aspects of the medical and surgical practice.
The Complete Surgeon
The trained surgeon must be aware of the need to differentiate between the business incentives of medical care and doing what is right for a sick individual. As financial and professional pressures become more intense, the challenge increases to appropriately prioritize and balance the demands of patient care, family, education, teaching, and research. For example, how does the surgeon deal with the choice between attending a child’s graduation or operating on an old patient who requests him rather than an extremely well-trained associate who is on call? How many times do surgeons make poor choices with respect to the balance of family vs work commitments? Someone else can
competently care for patients, but only parents can be uniquely present in the lives of their children. Time flies, and surgeons must often remind themselves that their lives and the lives of their family members are not just a dress rehearsal.
Knowing When to Quit
A 65-year-old surgeon who maintains a full operating and office schedule, is active in community and medical organizations, and has trained most of her surgical colleagues is considering where to go next with her career. Recently, her hospital acquired the equipment to allow robotic dissection in the area where she does her most complicated procedures. She has just signed up to learn this new technology, but is beginning to reflect on the advisability of doing this. How long should she continue at this pace, and how does she know when to slow down and eventually quit operating and taking the responsibility of caring for patients? Murray Brennan summarizes the dilemma of the senior surgeon well. The senior surgeon is old enough and experienced enough to do what he does well. He yearns for the less complicated days where he works and is rewarded for his endeavors. He becomes frustrated by restrictive legislation, the tyranny of compliance, and the loss of autonomy. Now regulated, restricted, and burdened with compliance, with every medical decision questioned by an algorithm or guideline, he watches his autonomy of care be ever eroded. Frustrated at not being able to provide the care, the education, and the role model for his juniors, he abandons the challenge.
Finishing with Grace
Each surgeon should continuously map a career pathway that integrates personal and professional goals with the outcome of maintaining value, balance, and personal satisfaction throughout his or her professional career. He or she should cultivate habits of personal renewal, emotional self-awareness, and connection with colleagues and support systems, and must find genuine meaning in work to combat the many challenges. Surgeons also need to set an example of good health for their patients. Maintaining these values and healthy habits is the work of a lifetime. Rothenberger describes the master surgeon as a person who not only knows when rules apply, recognizes patterns, and has the experience to know what to do, but also knows when rules do not apply, when they must be altered to fit the specifics of an individual case, and when inaction is the best course of action. Every occasion is used to learn more, to gain perspective and nuance. In surgery, this is the rare individual who puts it all together, combining the cognitive abilities, the technical skills, and the individualized decision-making needed to tailor care to a specific patient’s illness, needs, and preferences despite incomplete and conflicting data. The master surgeon has an intuitive grasp of clinical situations and recognizes potential difficulties before they become major problems. He prioritizes and focuses on real problems. He possesses insight and finds creative ways to manage unusual and complex situations. He is realistic, self-critical, and humble. He understands his limitations and is willing to seek help without hesitation. He adjusts his plans to fit the specifics of the situation. He worries about his decisions, but is emotionally stable.
Cystic Disorders of the Bile Ducts
 OVERVIEW
OVERVIEW
Cystic disorders of the bile ducts, although rare, are well-defined malformations of the intrahepatic and/or extrahepatic biliary tree. These lesions are commonly referred to as choledochal cysts,which is a misnomer, as these cysts often extend beyond the common bile duct (choledochus).
EPIDEMIOLOGY
Cystic disorders of the bile ducts account for approximately 1% of all benign biliary disease. Also, biliary cysts are four times more common in females than males. The majority of patients (60%) with bile duct cysts are diagnosed in the first decade of life, and approxi-mately 20% are diagnosed in adulthood.
CLASSIFICATION
Cystic dilatation of the bile ducts occurs in various shapes—fusi-form, cystic, saccular, and so on—and in different locations through-out the biliary tree. The most commonly used classification is the Todani modification of the Alonso-Lej classification.
ETIOLOGY
The exact etiology of biliary cysts is unknown.
CLINICAL PRESENTATION
The initial clinical presentation varies significantly between children and adults. In children, the most common symptoms are intermittent abdominal pain, nausea and vomiting, mild jaundice, and an abdom-inal mass. The classical triad of abdominal pain, jaundice, and a pal-pable abdominal mass associated with choledochal cyst is observed in only 10% to 15% of children, and it is rarely seen in adults. Symp-toms in adults often mimic those seen in patients with biliary tract disease or pancre-atitis.
SURGICAL MANAGEMENT
The definitive treatment of bile duct cysts usually includes surgical excision of the abnormal extrahepatic bile duct with biliary-enteric reconstruction. This approach relieves biliary obstruction, prevent-ing future episodes of cholangitis, stone formation, or biliary cirrho-sis and thus interrupting the inflammatory liver injury cycle. It also stops pancreatic juice reflux, and more importantly, it removes tissue at risk of malignant transformation.
Ethics in Surgery : R.I.S.K.
Renewed public attention is being paid to ethics today. There are governmental ethics commissions, research ethics boards, and corporate ethics committees. Some of these institutional entities are little more than window dressing, whereas others are investigative bodies called into being, for example, on suspicion that financial records have been altered or data have been presented in a deceptive manner. However, many of these groups do important work, and the fact that they have been established at all suggests that we are not as certain as we once were, or thought we were, about where the moral boundaries are and how we would know if we overstepped them. In search of insight and guidance, we turn to ethics. In the professions, which are largely self-regulating, and especially in the medical profession, whose primary purpose is to be responsive to people in need, ethics is at the heart of the enterprise.
Responsibility to the patient in contemporary clinical ethics entails maximal patient participation, as permitted by the patient’s condition, in decisions regarding the course of care. For the surgeon, this means arriving at an accurate diagnosis of the patient’s complaint, making a treatment recommendation based on the best knowledge available, and then talking with the patient about the merits and drawbacks of the recommended course in light of the patient’s life values. For the patient, maximal participation in decision making means having a conversation with the surgeon about the recommendation, why it seems reasonable and desirable, what the alternatives are, if any, and what the probable risks are of accepting the recommendation or pursuing an alternative course.
This view of ethically sound clinical care has evolved over the latter half of the 20th century from a doctor-knows-best ethic that worked reasonably well for both patients and physicians at a time when medical knowledge was limited and most of what medicine could do for patients could be carried in the doctor’s black bag or handled in a small, uncluttered office or operating room. What practical steps can be taken by clinicians to evaluate patient attitudes and behavior relative to the patient’s cultural context so that the physician and patient together can reach mutually desired goals of care? Marjorie Kagawa-Singer and her colleagues at the University of California, Los Angeles, developed a useful tool for ascertaining patients’ levels of cultural influence. It goes by the acronym RISK:
Resources: On what tangible resources can the patient draw, and how readily available are they?
Individual identity and acculturation: What is the context of the patient’s personal circumstances and her degree of integration within her community?
Skills: What skills are available to the patient that allow him to adapt to the demands of the condition?
Knowledge: What can be discerned from a conversation with the patient about the beliefs and customs prevalent in her community and relevant to illness and health, including attitudes about decision making and other issues that may affect the physician-patient relationship.
TRATAMENTO DA TROMBOSE HEMORROIDÁRIA

A trombose hemorroidária é uma condição dolorosa e desconfortável que ocorre quando um coágulo de sangue se forma dentro de uma hemorróida. Essa condição é mais comum em gestantes, pessoas com constipação intestinal crônica, e em situações que aumentam a pressão intra-abdominal, como exercícios físicos intensos e levantamento de peso. Neste artigo, exploraremos as causas, sintomas e opções de tratamento para a trombose hemorroidária, ajudando você a entender melhor essa condição e a buscar a melhor abordagem para o seu caso.
Causas da Trombose Hemorroidária
A trombose hemorroidária geralmente está relacionada a fatores de estilo de vida e hábitos pessoais. Os principais gatilhos incluem:
- Obstipação (prisão de ventre): O esforço excessivo para evacuar aumenta a pressão nas veias do ânus, e as fezes endurecidas podem causar traumatismo no tecido anal.
- Gravidez: A pressão adicional no abdômen durante a gravidez pode contribuir para o desenvolvimento da trombose.
- Esforços prolongados e levantamento de peso: Atividades que aumentam a pressão intra-abdominal são fatores de risco.
- Higiene inadequada: A falta de cuidados apropriados na região anal pode exacerbar a condição.
- Fatores adicionais: Permanecer sentado por longos períodos, consumo excessivo de alimentos picantes e bebidas alcoólicas, e prática de sexo anal.
Sintomas da Trombose Hemorroidária
Os principais sinais de trombose hemorroidária incluem:
- Dor intensa na região anal: A dor é geralmente súbita e pode ser bastante severa.
- Sangramento: Frequentemente observado durante a evacuação.
- Inchaço e aumento de volume: Um nódulo na região anal pode se tornar arroxeado ou preto, indicando a presença de um trombo.
Tratamentos Indicados
O tratamento da trombose hemorroidária varia conforme a gravidade da condição. Entre as abordagens recomendadas estão:
- Uso de analgésicos e pomadas anestésicas: Para alívio da dor e desconforto.
- Banhos de assento: Utilizar água morna para aliviar os sintomas e reduzir o inchaço.
- Correção dos hábitos alimentares: Aumentar a ingestão de fibras e líquidos para prevenir a obstipação.
- Tratamento cirúrgico: Em casos mais graves, pode ser necessário realizar uma cirurgia para remover a hemorróida e o trombo.
Se você apresenta sintomas semelhantes, é crucial consultar um médico para uma avaliação adequada e receber o tratamento adequado.
Gostou ❔ Nos deixe um comentário ✍️, ou mande sua dúvida pelo 💬 Chat On-line.
Lembre-se: A informação aqui fornecida é para orientação geral. Sempre consulte seu médico para aconselhamento específico sobre sua situação.
Não Deixe Sua Saúde Esperar! Entre em Contato Conosco Agora!
☎️ CHAT ONLINE 📞
Entre em contato conosco através da nossa central de atendimento dedicada. Nossos especialistas estão prontos para fornecer orientações personalizadas e responder a todas as suas perguntas. Juntos, podemos trabalhar para garantir o melhor para a sua saúde.
🩺(98)991304454 & (98)988664454📲
ATENDIMENTO REMOTO (TELEMEDICINA)
🤳🏻 Agende com os nossos #especialistas pelo WhatsApp ou Telefone
📲 👩🏽⚕️ Clínico: (98) 9 9130 4454
📲 👨🏻⚕️ Cirúrgico: (98) 9 8866 4454
#TromboseHemorroidária #SaúdeDigestiva #TratamentoHemorroidário #BemEstar #CuidadosComASaúde
VEJA AQUI ONDE FAZER UMA AVALIAÇÃO ESPECIALIZADA E RECEBER UMA SEGUNDA OPINIÃO
Leadership in SURGICAL TEAM

Leadership is a process of social influence in which one person can enlist the aid and support of others in the accomplishment of a common task. Successful leaders can predict the future and set the most suitable goals for organizations. Effective leadership among medical professionals is crucial for the efficient performance of a healthcare system. Recently, as a result of various events and reports such as the ‘Bristol Inquiry’, and ‘To Err is Human’ by the Institute of Medicine, the healthcare organizations across different regions have emphasized the need for effective leadership at all levels within clinical and academic fields. Traditionally, leadership in clinical disciplines needed to display excellence in three areas: patient care, research and education.
Within the field of surgery, the last decade has seen various transformations such as technology innovation, changes to training requirements, redistribution of working roles, multi-disciplinary collaboration and financial challenges. Therefore, the current concept of leadership demands to set up agendas in line with the changing healthcare scenario. This entails identifying the needs and initiating changes to allow substantive development and implementation of up-to-date evidence. This article delineates the definition and concept of leadership in surgery. We identify the leadership attributes of surgeons and consider leadership training and assessment. We also consider future challenges and recommendations for the role of leadership in surgery.
PRINCIPLES OF LEADERSHIP FOR GENERAL SURGEONS
BILIARY-ENTERIC ANASTOMOSIS
 The operative conduct of the biliary-enteric anastomosis centers around three technical steps: 1) identification of healthy bile duct mucosa proximal to the site of obstruction; 2) preparation of a segment of alimentary tract, most often a Roux-en-Y jejunal limb; and 3) construction of a direct mucosa-to-mucosa anastomosis between these two. Selection of the proper anastomosis is dictated by the indication for biliary decompression and the anatomic location of the biliary obstruction. A right subcostal incision with or without an upper midline extension or left subcostal extension provides adequate exposure for construction of the biliary-enteric anastomosis. Use of retractors capable of upward elevation and cephalad retraction of the costal edges are quite valuable for optimizing visual exposure of the relevant hilar anatomy.
The operative conduct of the biliary-enteric anastomosis centers around three technical steps: 1) identification of healthy bile duct mucosa proximal to the site of obstruction; 2) preparation of a segment of alimentary tract, most often a Roux-en-Y jejunal limb; and 3) construction of a direct mucosa-to-mucosa anastomosis between these two. Selection of the proper anastomosis is dictated by the indication for biliary decompression and the anatomic location of the biliary obstruction. A right subcostal incision with or without an upper midline extension or left subcostal extension provides adequate exposure for construction of the biliary-enteric anastomosis. Use of retractors capable of upward elevation and cephalad retraction of the costal edges are quite valuable for optimizing visual exposure of the relevant hilar anatomy.

Division of the ligamentum teres and mobilization of the falciform ligament off the anterior surface of the liver also facilitate operative exposure; anterocephalad retraction of the ligamentum teres and division of the bridge of tissue overlying the umbilical fissure are critical for optimal visualization of the vascular inflow and biliary drainage of segments II, III, and IV. Cholecystectomy also exposes the cystic plate, which runs in continuity with the hilar plate. Lowering of the hilar plate permits exposure of the left hepatic duct as it courses along the base of segment IVb. In cases of unilateral hepatic atrophy as a result of long-standing biliary obstruction or preoperative portal vein embolization, it is critical to understand that the normal anatomic relationships of the portal structures are altered. In the more common circumstance of right-sided atrophy, the portal and hilar structures are rotated posteriorly and to the right; as a result, the portal vein, which is typically most posterior, is often encountered first; meticulous dissection is necessary to identify the common bile duct and hepatic duct deep within the porta hepatis.
BILIARY-ENTERIC ANASTOMOSIS_THECNICAL ASPECTS
GASTROINTESTINAL STROMAL TUMORS (GIST)
INTRODUÇÃO
GIST, da sigla em inglês gastrointestinal stromal tumors, pertence a um grupo de tumores chamados sarcoma de partes moles. Essa neoplasia se diferencia dos outros tipos de tumores por iniciar-se na parede dos órgãos, junto às camadas musculares do trato gastrointestinal, mais especificamente, nas células do plexo mioenterico, chamadas células de Cajal. Tais células são responsáveis pela motilidade intestinal, sendo consideradas o marca-passo do trato gastrointestinal.
O tumor de GIST é relativamente raro, com estudos atuais mostrando uma prevalência anual em torno de 20 a 40 casos por milhão de habitantes. É mais comum entre pessoas de 50 a 60 anos de idade, sendo extremamente raros até os 20 anos. Por representar um tumor raro, recomenda-se que seja tratado por serviços especializados com cirurgiões do aparelho digestivo, que tenham experiência multidisciplinar na condução e no tratamento dos pacientes com este tumor.
O GIST pode se originar em qualquer local do trato gastrointestinal, do esôfago ao ânus. Em relação à distribuição, 50% a 60% das lesões são provenientes do estômago, 20% a 30% do intestino delgado, 10% do intestino grosso, 5% do esôfago e 5% de outros locais da cavidade abdominal.
DIAGNÓSTICO
A apresentação clínica dos pacientes portadores de GIST não é especifica e depende da localização e do tamanho do tumor. O GIST tem uma característica biológica que é uma mutação genética, com ativação do proto-oncogene Kit e a superexpressão do receptor tirosina quinase (c-Kit). Geralmente, o diagnóstico é feito por uma biópsia da lesão, que a depender da localização, pode ser feita por endoscopia, colonoscopia, ou ecoendoscopia. A tomografia computadorizada do abdômen é importante para avaliação da extensão do tumor e também pode ser utilizada em alguns casos para realização de biópsia do tumor. Não apresentam sinais e/ou sintomas específicos. Podem causar náuseas, vômitos, hemorragias intestinais (vômitos com sangue ou evacuações com sangue ou fezes enegrecidas), sensação de plenitude após alimentação, dor e distensão abdominal, ou presença de uma massa ou tumor palpável no abdômen.
TRATAMENTO
O tratamento padrão para pacientes com GIST não metastático, ou seja, não provenientes de outros órgãos, é a ressecção cirúrgica completa da lesão. Muitas vezes é necessária a cirurgia radical e de grande porte, com a retirada de estruturas e órgãos aderidos, oferecendo a maior chance de cura. O tratamento com imatinib, e mais atualmente ao sunitinib, é utilizado para doença metastática ou irressecável, com intuito de diminuir o tamanho da lesão para que a cirurgia possa ser realizada em melhores condições locais. Tais drogas também podem ser utilizadas após a cirurgia. Para o tratamento sistêmico pode ser necessário estudo genético específico para saber qual a mutação presente no tumor, com intuito de guiar a terapia em relação à dose e tipo de medicação utilizada.
FATORES DE RISCO
Não há fatores de risco diretamente relacionados a essa neoplasia. Manter hábitos de vida saudáveis, uma alimentação balanceada e a prática de exercícios físicos ajudam, de maneira geral, na prevenção do câncer.
PARA MAIS INFORMAÇÕES: http://www.gistsupport.org/
Avanços no tratamento cirúrgico das METÁSTASES HEPÁTICAS DE ORIGEM COLORRETAL
O câncer colorretal é o terceiro tumor mais frequente no ocidente. Cerca de 50% dos pacientes desenvolvem metástases hepáticas na evolução da doença, as quais são responsáveis por, no mínimo, dois terços das mortes. O avanço nas técnicas cirúrgicas e a melhora dos esquemas quimioterápicos têm permitido oferecer tratamento com intuito curativo a um número cada vez maior de pacientes. Os avanços recentes do tratamento das metástases hepáticas, incluindo estratégias para aumentar as ressecções (por exemplo: embolização da veia porta, ablação por radiofrequência, hepatectomia em dois tempos, quimioterapia de conversão e estratégia inversa de tratamento) e hepatectomias na presença de doença extra-hepática possibilitam uma melhor sobrevida dos pacientes.
TRANSPLANTE DE FÍGADO
Este artigo é destinado a pacientes que irão passar por um transplante hepático e seus familiares. Ele visa esclarecer dúvidas comuns e fornecer informações importantes para enfrentar a experiência de forma mais tranquila e informada.
1. Quando está indicado o transplante?
O transplante hepático é recomendado em casos de:
- Cirrose Hepática: Quando exames mostram função hepática diminuída ou sintomas como ascite, sangramento digestivo, encefalopatia hepática ou peritonite bacteriana.
- Hepatocarcinoma: Tumores originários do fígado, muitas vezes associados à cirrose, podem ser tratados com transplante.
- Colangite Esclerosante e Obstrução Intratável de Vias Biliares: Doenças que causam obstrução das vias biliares e infecções graves.
- Hepatite Fulminante e Perda do Fígado Transplantado: Em casos de hepatite grave ou perda do enxerto transplantado dentro de 30 dias, a urgência é priorizada.
2. Quais são as contra-indicações ao transplante hepático?
Não é indicado realizar o transplante em situações como:
- Doença avançada em outros órgãos.
- Tumores fora do fígado.
- Abuso atual de drogas ou álcool.
- Incapacidade de seguir orientações médicas.
- Infecção ativa (o transplante pode ser realizado após a infecção ser controlada).
A idade avançada não é mais uma contra-indicação absoluta, mas deve ser avaliada individualmente.
3. A fila de transplante
Atualmente, a fila de transplante no Brasil é organizada pelo sistema Meld/Peld, que prioriza pacientes com base na gravidade da doença. A fila é subdividida por grupo sanguíneo (A, B, AB, O) e compatibilidade com o tamanho do paciente. Pacientes com grupo sanguíneo raro (AB) podem receber órgãos de todos os grupos.
4. O fígado “não ideal” (marginal)
Órgãos “não ideais” ou marginais podem ter características menos perfeitas, como mais gordura ou doadores com condições subótimas. Eles são destinados a pacientes com necessidades urgentes, como aqueles com tumores hepáticos.
5. A equipe
A equipe de transplante é composta por diversos profissionais, incluindo médicos, enfermeiros, nutricionistas, psicólogos e fisioterapeutas. Cada paciente passa por avaliações detalhadas de todos esses profissionais.
6. Como proceder em caso de emergências durante a espera pelo transplante
Em situações urgentes, dirija-se ao pronto-socorro ou entre em contato com sua equipe médica. As emergências incluem:
- Vômitos com sangue.
- Fezes com sangue ou escurecidas.
- Queda de pressão, mal-estar súbito.
- Colangite (febre, dor abdominal, icterícia).
- Peritonite (infecção abdominal).
7. As reuniões com a Coordenação de Enfermagem de Transplantes
Reuniões regulares são realizadas para pacientes na fila e seus familiares, oferecendo a oportunidade de trocar experiências, fazer perguntas e receber atualizações sobre a lista de espera.
8. A doação de órgãos através de doador em morte encefálica
A doação é um ato voluntário feito com consentimento familiar. O paciente deve estar em morte encefálica, uma condição onde não há atividade cerebral, mas o coração e outros órgãos ainda funcionam. A entidade responsável é o Rio Transplante e os dados do doador são confidenciais.
9. Chamada para o transplante
Mantenha-se disponível e acessível para a equipe de transplante, com telefone atualizado e a uma distância máxima de duas horas do hospital. Caso seja chamado, esteja preparado para o possível ajuste no órgão doado.
A CIRURGIA DE TRANSPLANTE HEPÁTICO
A cirurgia dura entre 5 a 8 horas e é dividida em duas etapas principais:
- Captação: Retirada do fígado doado, que pode ser considerado apto, marginal ou inapto.
- Transplante: O fígado doente é retirado e o novo órgão é implantado, com a realização das anastomoses das veias, artéria hepática e via biliar.
Pós-operatório Imediato
Você será monitorado na UTI por aproximadamente 48 horas. Equipamentos como tubos respiratórios, eletrodos, sondas e drenos serão usados para garantir segurança e monitoramento.
Pós-operatório
A internação média é de 2 semanas, variando conforme o paciente. É importante realizar exames regularmente e seguir orientações médicas para movimentação e exercícios respiratórios.
Medicação
Os imunosupressores, fornecidos pelo SUS, são essenciais para evitar a rejeição do transplante. Familiarize-se com o processo de obtenção e renovação desses medicamentos. Outras medicações de rotina devem ser providenciadas pela família.
Intercorrências após o Transplante
Monitorar sinais de rejeição e infecções é crucial. Mantenha-se saudável, evite álcool e siga as orientações médicas rigorosamente.
Alta Hospitalar
Antes da alta, você receberá orientações detalhadas e agendamentos para consultas e exames. Siga as recomendações de fisioterapia, nutrição e outros cuidados necessários.
Seguimento Inicial e Tardio
O acompanhamento pós-transplante é fundamental. As consultas variam ao longo do tempo, com exames laboratoriais e visitas regulares ao hospital.
Efeitos Colaterais
Os imunosupressores podem causar efeitos colaterais, como tremores e aumento da glicose. Informe seu médico sobre qualquer efeito adverso e não suspenda a medicação por conta própria.
Cuidados Gerais
Controle o peso, colesterol, glicose e pressão arterial. Evite bebidas alcoólicas, use máscara em locais públicos, evite contato com pessoas doentes e exposição solar excessiva. Mantenha acompanhamento ginecológico e dentário regular e consulte seu médico antes de tomar novos medicamentos. Este artigo é uma referência para ajudar você a entender e gerenciar o processo de transplante hepático. Mantenha-se em contato com sua equipe médica para qualquer dúvida ou preocupação.
A cirurgia é uma forma de terapia para as doenças que é motivada pelo CORAÇÃO, planejada na CABEÇA e executada pelas MÃOS.
“A cirurgia é uma forma de terapia para as doenças que é motivada pelo CORAÇÃO, planejada na CABEÇA e executada pelas MÃOS.”
Prof . Phd. Tom DeMeester
DEFINIÇÃO DE CIRURGIA (By Tom DeMeester / Gastrão 2012)
Lesão de Vias Biliares na Colecistectomia: Prevenção e Tratamento
A via laparoscópica tem sido reconhecida como padrão de excelência para a colecistectomias. Phillipe Mouret foi quem primeiro a realizou em 1987, mas outros procedimentos já haviam sido realizados por laparoscopia e foram descritos por ginecologistas. Desenvolvida no final da década de 80 e início dos anos 90, a videolaparoscopia mudou os conceitos de acesso cirúrgico e campo operatório, introduzindo a concepção de “cirurgia minimamente invasiva”.A colecistectomia é um dos procedimentos cirúrgicos mais realizados no mundo. Com o advento da videolaparoscopia, tornou-se uma cirurgia menos traumática, mais estética, com períodos mais curtos de internação. Em contrapartida, observou-se o aumento da incidência de lesões de via biliar extra-hepática quando comparado ao procedimento aberto, fato preocupante devido à morbidade elevada desse tipo de lesão, cuja mortalidade não é desprezível.