Surgical Technique of Liver Resection for the Treatment of HCC
The incidence of HCC is increasing in the worldwide. Surgery in the form of liver resection or transplantation remains the mainstay of curative treatment for HCC, even though selected patients with small tumours may also be cured with ablation. Liver resection and transplantation are not necessarily two binary choices in most patients and, despite all the debates, are often complementary treatment modalities ideally suited to different patient groups. Thus characterisation of patient and tumour characteristics to guide decision making is vital to achieve the best outcome for patients.
1.Anatomical Resection or Not?
The aim of liver resection in patients with HCC and CLD is that it should be curative with resection of tumour vascular territories and also preserve as much liver volume as possible to prevent postoperative liver failure. EASL guidelines recommend anatomical resection of HCC, whereby the lines of resection match the limits of one or more functional segments of the liver. This is based on evidence suggesting superior oncological outcomes in addition to a reduction in the risk of bleeding and biliary fistula. Although there are no randomised data, a meta-analysis including 2000 patients from 12 non-randomised comparative trials did not show any benefit of anatomical compared with non-anatomical resection in 1-, 3- and 5-year survival, recurrence rate, postoperative morbidity or blood loss . It is practice to perform an anatomical resection for tumours >2 cm, and for smaller tumours in anatomically favourable positions, a wedge with adequate margin is often sufficient. Modifying techniques to maximise parenchymal preservation preserving adequate margins are often the key in these patients.
2. Anterior Approach
The anterior approach, as described by Professor Belghiti , has been advocated for large right-sided tumours. This technique involves transection of the liver parenchyma to the IVC without mobilisation of the liver with the theoretical advantage of less tumour seeding. A prospective randomised controlled trial compared the anterior and conventional approach on 120 patients with large (>5 cm) HCCs. The anterior approach group had less blood transfusion requirements and a significantly longer overall survival (68.1 v 22.6 months; p = 0.006).
3.Parenchymal Transection
As in liver resection for other indications, there is no good evidence to indicate that a single method of parenchymal transection, application of fibrin sealants or intermittent inflow occlusion is beneficial in surgery for HCC. There is also no evidence to suggest that using special equipment for liver resection is of any benefit in decreasing the mortality, morbidity, or blood transfusion requirements. Surgeons should use techniques in which they have been trained and can demonstrate acceptable outcomes.
4. Laparoscopic Approach
Laparoscopic HCC resections are gaining popularity as the approach is more widely adopted across centres. It is important that patients for laparoscopic resection are selected based on the technical capabilities of the surgeon and centre, and the proper mentoring takes place during the learning curve. A summary of published metaanalyses concluded that the laparoscopic approach was associated with improved short-term outcomes (blood loss, complication rates and hospital length of stay) without compromising long-term oncological outcomes. It is worth noting that there are no randomised data; however a number of trials are in progress. Furthermore,their analysis suggested that the incidence of postoperative ascites and liver failure is decreased in the selected group of laparoscopic liver resections . A further metaanalysis of cirrhotic patients up to Child-Pugh B undergoing laparoscopic compared with open liver resection for HCC confirmed these perioperative benefits .
5. Robotic Approach
Although still very much in its infancy, the application of robotic surgery to HCC resection can theoretically yield similar advantages in short-term outcomes to the laparoscopic technique. The only comparative study between robotic and open liver resection for HCC included 183 patients undergoing robotic hepatectomy who were compared using propensity scoring with a cohort of 275 open resections. The robotic group required longer operating time (343 vs 220 min), shorter hospital stays (7.5 vs 10.1 days) and lower dosages of postoperative patient-controlled analgesia (350 vs 554 ng/kg). The 3-year disease-free survival of the robotic group was comparable with that of the open group (72.2% vs 58.0%; p = 0.062), as was the 3-year overall survival (92.6 vs 93.7%; p = 0.431). The associated financial costs of robotic surgery still pose a limitation to its adoption, and it is unclear if this approach is associated with any significant advantages over laparoscopic rather than open resection.
6. Associating Liver Partition with Portal Vein Ligation for Staged
Hepatectomy (ALPPS)/TAE/PVE
ALPPS is still considered an experimental technique in which a first-stage procedure consisting of physical liver splitting and portal vein ligation is followed by a second stage of resection of the HCC and associated liver segments. The advantage seen in colorectal liver metastases is that of rapid hypertrophy for the FLR. There are only limited data describing outcomes of ALPPS for HCC; however an analysis of 35 patients in the international ALPPS registry showed an impressive FLR hypertrophy of 47% following the first stage of the procedure that was associated with a 31% perioperative mortality rate. The majority of these patients were in the intermediate-stage category of the BCLC algorithm. Further evaluation is required prior to routine use of ALPPS for HCC resection, and it is the view of the authors that ALPPS may be a procedure best reserved for carefully selected patients who have bilateral disease.
7. Combined Resection with RFA for Bilobar HCC
For patients with multiple or bilobar HCC in whom resection is contraindicated due to inadequate FLR, combined resection and radiofrequency ablation (RFA) may yield better results than alternative treatments. A single-centre study compared patients with bilobar liver HCCs who underwent resection (n = 89), combination of resection and RFA (n = 114) and TACE (n = 161). The results showed that 1-, 3- and 5-year survival was better in both resection and combined resection, and RFA groups compared with TACE and survival and disease-free survival were comparable between both surgical groups. They concluded that resection combined with RFA provided a chance for cure in patients with bilobar HCC, and provided liver function is preserved, aggressive treatment can improve prognosis.
Principles of Surgical Resection of Hepatocellular Carcinoma
INTRODUCTION
There has been significant improvement in the perioperative results following liver resection, mainly due to techniques that help reduce blood loss during the operation. Extent of liver resection required in HCC for optimal oncologic results is still controversial. On this basis, the rationale for anatomically removing the entire segment or lobe bearing the tumor, would be to remove undetectable tumor metastases along with the primary tumor.
SIZE OF TUMOR VERSUS TUMOR FREE-MARGIN
Several retrospective studies and meta-analyses have shown that anatomical resections are safe in patients with HCC and liver dysfunction, and may offer a survival benefit. It should be noted, that most studies are biased, as non-anatomical resections are more commonly performed in patients with more advanced liver disease, which affects both recurrence and survival. It therefore remains unclear whether anatomical resections have a true long-term survival benefit in patients with HCC. Some authors have suggested that anatomical resections may provide a survival benefit in tumors between 2 and 5 cm. The rational is that smaller tumors rarely involve portal structures, and in larger tumors presence of macrovascular invasion and satellite nodules would offset the effect of aggressive surgical approach. Another important predictor of local recurrence is margin status. Generally, a tumor-free margin of 1 cm is considered necessary for optimal oncologic results. A prospective randomized trial on 169 patients with solitary HCC demonstrated that a resection margin aiming at 2 cm, safely decreased recurrence rate and improved long-term survival, when compared to a resection margin aiming at 1 cm. Therefore, wide resection margins of 2 cm is recommended, provided patient safety is not compromised.
THECNICAL ASPECTS
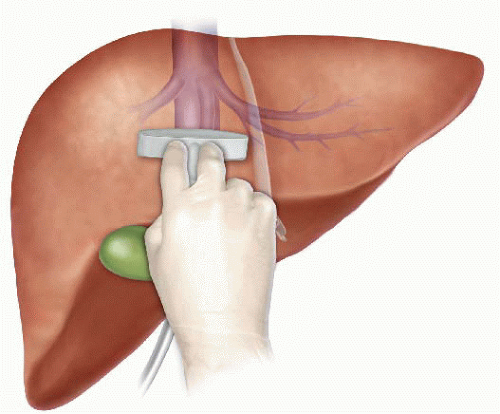
Intraoperative ultrasound (IOUS) is an extremely important tool when performing liver resections, specifically for patients with HCC and compromised liver function. IOUS allows for localization of the primary tumor, detection of additional tumors, satellite nodules, tumor thrombus, and define relationship with bilio-vascular structures within the liver. Finally, intraoperative US-guided injection of dye, such as methylene-blue, to portal branches can clearly define the margins of the segment supplied by the portal branch and facilitate safe anatomical resection.
The anterior approach to liver resection is a technique aimed at limiting tumor manipulation to avoid tumoral dissemination, decrease potential for blood loss caused by avulsion of hepatic veins, and decrease ischemia of the remnant liver caused by rotation of the hepatoduodenal ligament. This technique is described for large HCCs located in the right lobe, and was shown in a prospective, randomized trial to reduce frequency of massive bleeding, number of patients requiring blood transfusions, and improve overall survival in this setting. This approach can be challenging, and can be facilitated by the use of the hanging maneuver.

Multiple studies have demonstrated that blood loss and blood transfusion administration are significantly associated with both short-term perioperative, and long-term oncological results in patients undergoing resection for HCC. This has led surgeons to focus on limiting operative blood loss as a major objective in liver resection. Transfusion rates of <20 % are expected in most experienced liver surgery centers. Inflow occlusion, by the use of the Pringle Maneuver represents the most commonly performed method to limit blood loss. Cirrhotic patients can tolerate total clamping time of up to 90 min, and the benefit of reduced blood loss outweighs the risks of inflow occlusion, as long as ischemia periods of 15 min are separated by at least 5 min of reperfusion. Total ischemia time of above 120 min may be associated with postoperative liver dysfunction. Additional techniques aimed at reducing blood loss include total vascular isolation, by occluding the inferior vena cava (IVC) above and below the liver, however, the hemodynamic results of IVC occlusion may be significant, and this technique has a role mainly in tumors that are adjacent to the IVC or hepatic veins.

Anesthesiologists need to assure central venous pressure is low (below 5 mmHg) by limiting fluid administration, and use of diuretics, even at the expense 470 N. Lubezky et al. of low systemic pressure and use of inotropes. After completion of the resection, large amount of crystalloids can be administered to replenish losses during parenchymal dissection.
LAPAROSCOPIC RESECTIONS
Laparoscopic liver resections were shown to provide benefits of reduced surgical trauma, including a reduction in postoperative pain, incision-related morbidity, and shorten hospital stay. Some studies have demonstrated reduced operative bleeding with laparoscopy, attributed to the increased intra-abdominal pressure which reduces bleeding from the low-pressured hepatic veins. Additional potential benefits include a decrease in postoperative ascites and ascites-related wound complications, and fewer postoperative adhesions, which may be important in patients undergoing salvage liver transplantation. There has been a delay with the use of laparoscopy in the setting of liver cirrhosis, due to difficulties with hemostasis in the resection planes, and concerns for possible reduction of portal flow secondary to increased intraabdominal pressure. However, several recent studies have suggested that laparoscopic resection of HCC in patients with cirrhosis is safe and provides improved outcomes when compared to open resections.

Resections of small HCCs in anterior or left lateral segments are most amenable for laparoscopic resections. Larger resections, and resection of posterior-sector tumors are more challenging and should only be performed by very experienced surgeons. Long-term oncological outcomes of laparoscopic resections was shown to be equivalent to open resections on retrospective studies , but prospective studies are needed to confirm these findings. In recent years, robotic-assisted liver resections are being explored. Feasibility and safety of robotic-assisted surgery for HCC has been demonstrated in small non-randomized studies, but more experience is needed, and long-term oncologic results need to be studied, before widespread use of this technique will be recommended.
ALPPS: Associating Liver Partition with Portal vein ligation for Staged hepatectomy
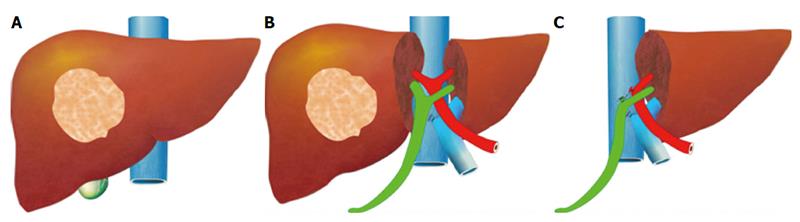
The pre-operative options for inducing atrophy of the resected part and hypertrophy of the FLR, mainly PVE, were described earlier. Associating Liver Partition with Portal vein ligation for Staged hepatectomy (ALPPS) is another surgical option aimed to induce rapid hypertrophy of the FLR in patients with HCC. This technique involves a 2-stage procedure. In the first stage splitting of the liver along the resection plane and ligation of the portal vein is performed, and in the second stage, performed at least 2 weeks following the first stage, completion of the resection is performed. Patient safety is a major concern, and some studies have reported increased morbidity and mortality with the procedure. Few reports exist of this procedure in the setting of liver cirrhosis. Currently, the role of ALPPS in the setting of HCC and liver dysfunction needs to be better delineated before more widespread use is recommended.










