Mechanism of Bile Duct Injury: Understanding the Risks in Laparoscopic Cholecystectomy
Introduction
Laparoscopic cholecystectomy, the “gold standard” for treating symptomatic gallbladder disease, has transformed surgical practice since its introduction in the early 1990s. Despite its widespread adoption and the improved safety profile over time, the procedure remains fraught with risks, particularly bile duct injuries (BDIs). The incidence of BDIs during laparoscopic cholecystectomy has declined from its peak, but this complication still represents a significant challenge in digestive surgery, leading to substantial morbidity, mortality, and legal consequences. In Brazil, where an estimated 300,000 cholecystectomies are performed annually, BDIs continue to be a significant concern. This article delves into the mechanisms of bile duct injuries during laparoscopic cholecystectomy, exploring the factors that contribute to these adverse events and their implications for surgical practice.
Development of the Theme
The advent of laparoscopic cholecystectomy marked a turning point in the management of gallbladder disease, offering patients reduced postoperative pain, shorter hospital stays, and faster recovery times. However, the initial enthusiasm for this minimally invasive approach was tempered by a notable increase in bile duct injuries. As surgeons adapted to the new technique, the incidence of BDIs spiked, with early reports indicating injury rates as high as 0.7%. Today, with increased experience and refined techniques, the incidence has decreased to approximately 0.1% to 0.2%. Despite these improvements, the risk remains significant, with estimates suggesting that one in three general surgeons will cause a bile duct injury at some point in their careers.
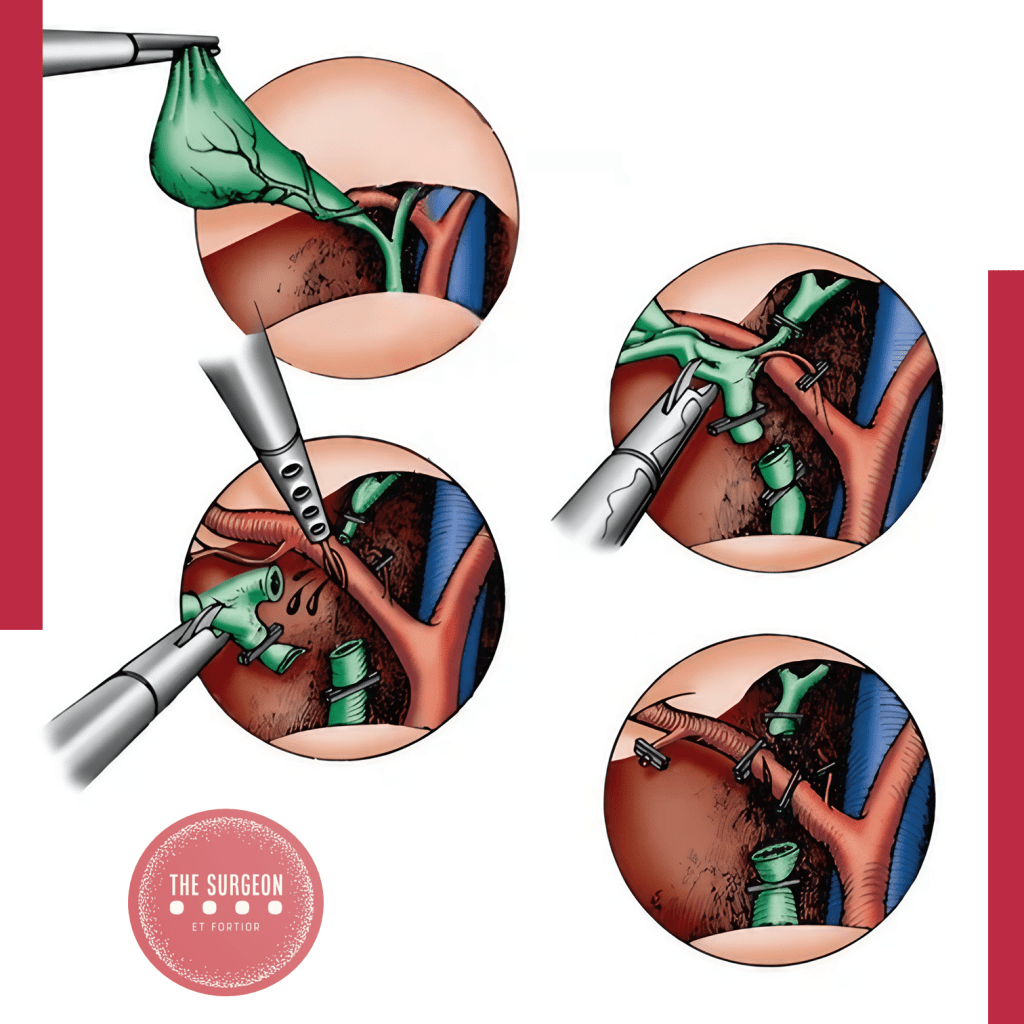
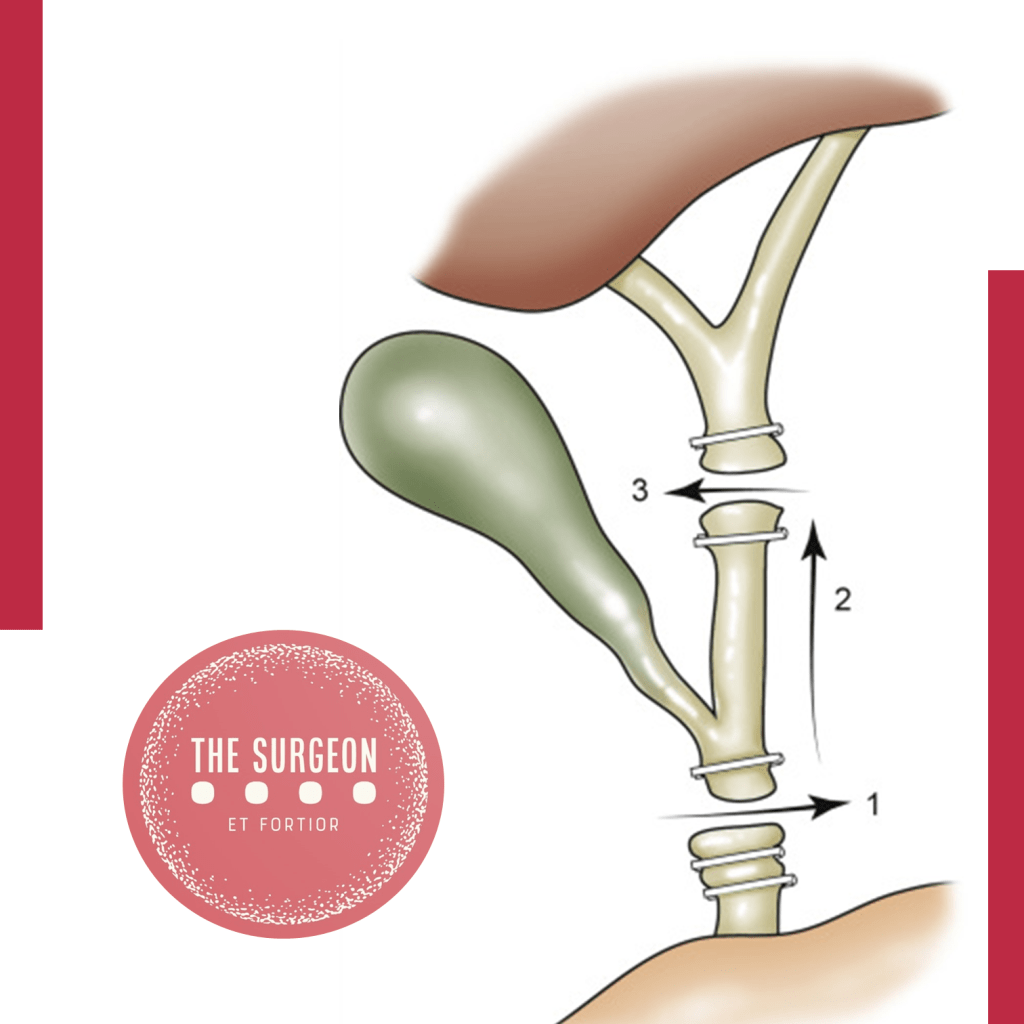
Iatrogenic bile duct injuries are most often the result of perceptual errors in identifying biliary anatomy during surgery. The most common injury involves a complete transection of the common bile duct, which is also the most difficult to manage. Typically, excessive cephalad retraction of the gallbladder fundus or insufficient lateral retraction on the infundibulum leads to an alignment of the cystic and common bile ducts, causing the common bile duct to be mistaken for the cystic duct. This misidentification results in clipping and transecting the common bile duct—a scenario that can lead to devastating outcomes if not promptly recognized and appropriately managed.
Inflammatory conditions, such as acute or chronic cholecystitis, further complicate the surgical landscape. Thickened and friable tissue, along with adhesions, can obscure normal anatomical landmarks, increasing the difficulty of the procedure. Aberrant biliary anatomy, such as a low-lying right hepatic duct, poses additional risks, as these anatomical variations can be easily overlooked during surgery, leading to unintended ductal injury.
Energy sources used for hemostasis, such as electrocautery, introduce another layer of complexity. Excessive or inappropriate use of these tools can damage the bile duct or its blood supply, resulting in stricture formation or bile leaks. Another common mechanism of injury occurs when a clip is inadvertently placed across the common bile duct, often in a hurried attempt to control bleeding from the hilum without a clear view of the anatomy.
In the context of laparoscopic cholecystectomy, BDIs are particularly perilous when the common bile duct is mistaken for the cystic duct. This classical injury pattern, first described by Davidoff and colleagues, typically involves clipping and dividing the common bile duct, with further proximal dissection leading to injury of the right hepatic artery and more proximal ductal structures, including the common hepatic duct and intrahepatic ducts. Poor visualization due to inadequate illumination, excessive smoke, or intraoperative bleeding exacerbates these risks, making meticulous surgical technique and optimal visualization crucial to avoiding these injuries.
Key Points
- Perceptual Errors: The primary mechanism of bile duct injury during laparoscopic cholecystectomy is the misidentification of biliary anatomy, particularly the confusion between the cystic and common bile ducts.
- Risk Factors: Inflammatory conditions, aberrant anatomy, and excessive use of energy devices significantly increase the risk of bile duct injuries.
- Incidence: Despite advancements in technique, bile duct injuries remain a significant concern, with a 0.1% to 0.2% incidence in laparoscopic cholecystectomy. In Brazil, the annual rate of cholecystectomies underscores the importance of vigilance in preventing these injuries.
- Complications: Bile duct injuries can lead to severe complications, including biliary stricture, leakage, infection, and even death. The financial and legal implications further highlight the need for preventive measures.
Conclusion
Understanding the mechanisms of bile duct injury during laparoscopic cholecystectomy is crucial for improving surgical outcomes and minimizing patient morbidity. Surgeons must remain vigilant in identifying biliary anatomy, particularly in the presence of risk factors such as inflammation and aberrant anatomy. Enhanced visualization techniques, careful dissection, and judicious use of energy devices are essential strategies to reduce the incidence of BDIs. As the field of minimally invasive surgery continues to evolve, ongoing education and training in these areas are paramount to ensuring patient safety and improving the quality of care.
In the words of Alexis Carrel, “There is no such thing as minor surgery, but there are many minor surgeons”. This sentiment is particularly relevant to the surgical treatment of biliary diseases, where the combination of skill, experience, and compassion is vital to patient outcomes.
Did you like it? Leave us a comment ✍️, share on your social networks, and | or send your question via 💬 Online Chat in our Instagram DM.